On December 2019, the SARS-CoV-2, the Coronavirus-19 (COVID-19) disease agent, was first reported in China. In Brazil, it was first reported on February 26th, and since then, Brazil has been witnessing a massive increase in the number of cases and deaths resulting from COVID-19, becoming the new Coronavirus-19 hotspot.1 We read with interest the paper by Parras et al.2, reporting a case of coinfection of COVID-19 and Influenza A, which may impact the diagnosis and the diseases development. Giving the possibility of coinfection with other respiratory pathogens (with similar symptoms), we would like to highlight the coinfection by SARS-CoV-2 and Tuberculosis (TB) and the increased risk of complications and fatality rates. Nevertheless, here we raise awareness of the Brazilian pandemic scenario, which can be aggravated in the exposition of vulnerable and marginalized population, who are likely to be the most affected by both diseases and more exposed to socioeconomic and epidemiologic risks.3
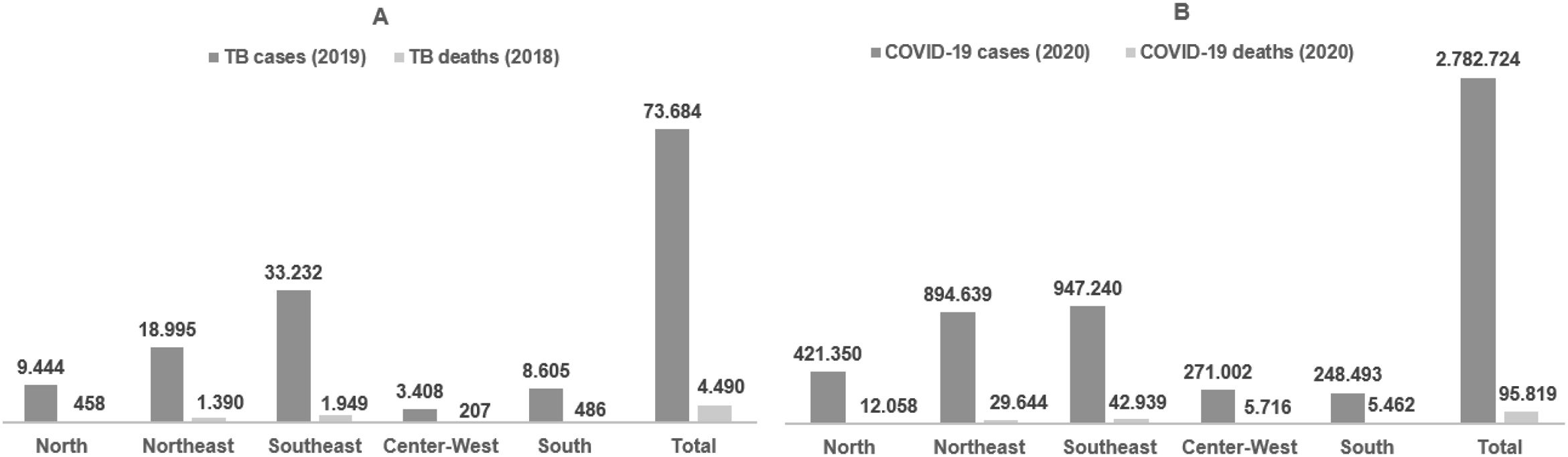
TB is the most mortal infectious disease in the world, where 1.5 million people died, and another ten million people were affected by the disease in 2018.4 Although Brazil is developing several actions to reduce morbidity and mortality (i.e., BCG vaccine implementation, investigation of latent infection, treatment, incorporation of technologies to fight TB in the National Health System – Sistema Único de Saúde - SUS), in 2019, 73,864 new TB cases were registered (200 new cases/day), with an incidence of 35 cases per 100,000 habitants, and increased incidence coefficient in the years of 2017 and 2018.5
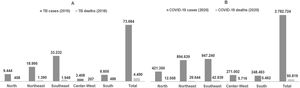
A higher rate of TB is observed in Southeast and North regions, where there is an incidence above 51 cases per 100,000 inhabitants, while the highest mortality rates are seen in Southeast, North, Northeast and South regions, with a mortality rate between 2,1 and 4,3 deaths per 100,000 habitants.5 The TB persistence in Brazil is highly linked to poverty conditions, social and economic inequalities, the lack of diagnostic in some regions and the adhesion difficulties to the treatment. Moreover, in Brazil, until August 4th, 2020, almost 3 million cases and 100,000 deaths were registered, and the highest incidence of COVID-19 was mainly observed in the Southeast, Northeast and North regions, where local health systems declared collapse, although South and Center-West regions are reporting a rampant increase in cases,1,6 with possible impact and dissemination of COVID-19 in Brazilian regions and with the highest rates of contamination by TB (Fig. 1). Furthermore, it was reported that cases of TB patients with COVID-19 coinfections progress to the severe type of COVID-19 and showed more extended recovery period,7 as well as TB-HIV coinfection or chronic lung disease, which are will more likely to succumb to COVID-19.8,9
Due to the high transmissibility of the Mycobacterium tuberculosis as well as SARS-CoV-2 thriving with crowding, close contact, and aerosol,1,4 some important focuses have been observed in Brazil, not only in regions with high population density but also in the high incidence of TB in carceral system (8154 new cases of TB in Brazil in 2019), with also a high number of cases of COVID-19.5 In parallel, COVID-19 cases have risen in indigenous populations, which are historically known for the devastating epidemic cases in Latin-America. These problems require extreme attention since the impact of COVID-19, plus the pre-existent TB conditions, represent a major concern in more vulnerable populations, where access to basic sanitation, recurrent infections and chronic diseases are not unusual. Of note, the possibility of a coinfection caused by COVID-19 and TB would be an aggravating situation, beyond the clinical manifestations, the diagnostic would be more complicated since the suspicion of having TB does not exclude the possibility of having COVID-19.
In view of this scenario, not only social inequalities must be highlighted, but also the possibility of coinfections between SARS-CoV-2 and other respiratory pathogens. Clinical features and treatment of patients with TB and COVID-19 remain poorly understood, which can further impact the Brazilian health system, since this type of coinfection is more likely to develop sequelae and complicate the clinical evolution. Moreover, barriers to rapid and complete diagnosis and management for both TB and COVID-19 may be an aggravating in long-term consequences in economic, social and health sectors in all Brazilian society and public health,10 which requires urgent actions and the need of more research for the prevalence of coinfections in the Brazilian scenario.
FundingThis work was supported with a grant (CP 10/2019) of the Fundação Araucária and APC.
Conflict of interestFFT is a CNPq researcher. The other authors declared no competing interests.