Lung infections in highly immunocompromised individuals, including patients living with HIV not undergoing antiretroviral treatment (ART), have a diverse aetiology and overlapping clinical characteristics.1 This may hamper the diagnosis of coinfections.
We present a case of a 42-year-old Bolivian woman living with HIV, without antiretroviral therapy (ART), a 50 CD4+ cells/μL count, and a viral load of 6.6 log10 copies/mL. She was admitted at the Emergency Room complaining of fever, diarrhoea, vomits, and a 10kg loss of weight over the last 6 months after a 2 year-stage in her native country. Laboratory examinations showed hepatic alteration.
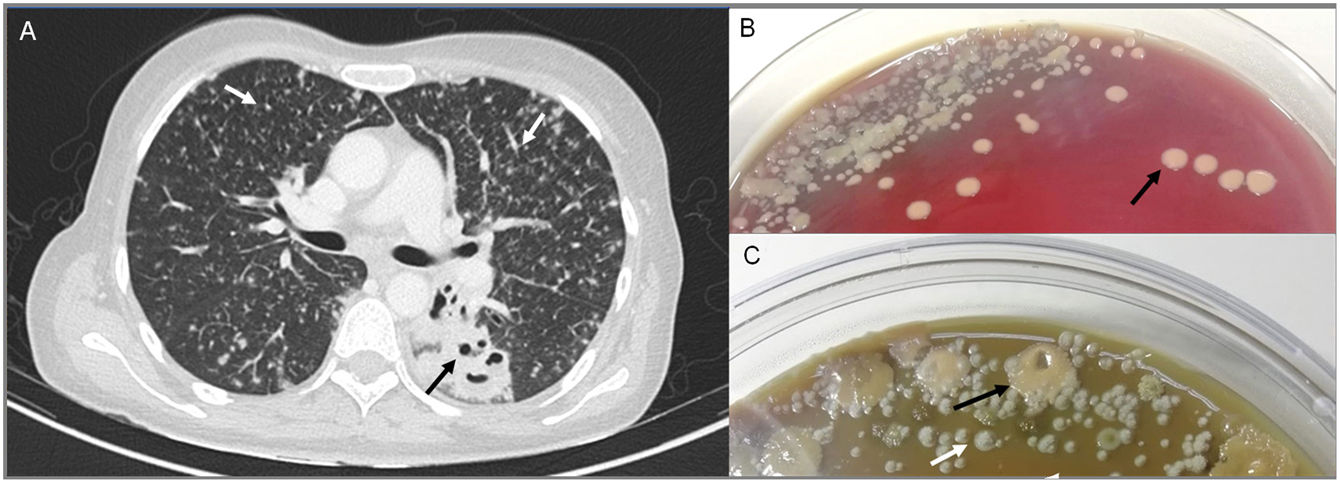
Thoracoabdominal CT scan revealed diffuse bilateral micronodular pattern suggestive of miliary tuberculosis, pulmonary cavities in the lower left lobe, and diffuse lymphadenopathies (Fig. 1A). Microbiological workup included conventional, fungal, and mycobacterial cultures from bronchoscopy specimens, Mycobacterium tuberculosis PCR, Pneumocystis spp. PCR, cryptococcal antigen test, serum β-d-glucan and detection of antibodies against dimorphic fungi and imported parasitic diseases. Serological, cryptococcal antigen and PCR tests were negative, whereas (1,3)-β-d-glucan was positive (28.50pg/mL).
Thoracoabdominal computed tomography scan showing diffuse bilateral micronodular pattern indicated by white arrows and pulmonary cavities in the upper segment of lower left lobe pointed by a black arrow (A). Conventional culture plates of bronchoscopy specimen after 4 days of incubation (B). Conventional culture plates of bronchoscopy specimen after 17 days of incubation (C). Black arrows point Rhodoccoccus hoagii colonies and white arrow points Histoplasma capsulatum colonies.
Empiric antitubercular therapy and anti-Pneumocystis prophylaxis were started but the patient progressively deteriorated suffering from asthenia, dyspnoea, night cough, and bilateral pleuritic pain.
After 4 days of incubation (5% blood agar, 5% CO2, 37°C), mucoid salmon-pink colonies identified as Rhodococcus hoagii (formerly Rhodococcus equi) by MALDI-TOF (bioMérieux),2 were isolated in culture plates of respiratory specimens (Fig. 1B). Levofloxacin and imipenem were added while rifampicine was kept.
As the hepatic alteration remained unexplained, a liver biopsy was performed. Two weeks later, the Pathology Department reported an acute granulomatous hepatitis, with abundant small yeast-like structures within the granulomas. Concurrently, brownish white yeast-like colonies became visible in the bronchoscopy specimens extended culture (Fig. 1C) corresponding to thin hyaline hyphae, small microconidia, and spiked spheric macroconidia. Histoplasma capsulatum identification was confirmed by MALDI-TOF. Histoplasma spp. PCR from deparaffinised hepatic tissue was positive.
The final diagnosis was disseminated histoplasmosis and R. hoagii pulmonary coinfection. She was started on amphotericin B, switching to oral itraconazole 18 days later, while she was kept on antimicrobial treatment against R. hoagii. Over the following year, clinical and radiological improvement was observed. Antitubercular treatment was withdrawn as presence of Mycobacteria spp. was not confirmed; anti-Pneumocystis prophylaxis, however, was kept until a CD4+ count >200cells/μL was reached and the viral load became undetectable.
Antitubercular therapy was promptly initiated as a 30% of AIDS without ART from Latin America and presenting miliary pattern have tuberculosis,3 a pattern similar to other granulomatous infections such as rhodococcosis, cryptococcosis, pneumocystosis and endemic fungal diseases.1 Upper lobe cavities may also be found in R. hoagii and fungal pneumonia.1 Multiple opportunistic infections have been described in 8% of Latin-American AIDS patients.4
In our country, patients living with HIV are rarely infected by intracellular pathogens like R. hoagii nowadays; besides, Histoplasmosis is infrequently seen in non-endemic countries, so physicians may not be familiar with their clinical presentation, increasing the risk of missing their diagnosis.5 Although R. hoagii explained the necrotizing pneumonia6 it did not fully explained the micronodular pattern and the clinical manifestation. A positive BD-glucan test, the risk of potential exposure in Bolivia along with a compatible chest imaging led us to search for endemic fungi.
H. capsulatum was reported by the laboratory 22 days after admission. In Europe, disseminated histoplasmosis, the most life-threatening form, is usually diagnosed in the setting of an advanced HIV infection.7
Microbiological confirmation in non-endemic regions is challenging. Combined detection of Histoplasma antigen in urine and serum, the most effective way to diagnose disseminated histoplasmosis, is not widely available out of endemic areas.8 Serology turns positive 4–8 weeks after infection9 but it may fail in immunocompromised patients, as was our case.8 The (1,3)-β-d-glucan serum antigen, although unspecific, is usually positive in disseminated forms.10 Cultures, remain the gold standard, but they lack quickness and sensitivity.8 Real-time PCR assays can reach a sensitivity around 90–95%. The Histoplasma PCR in respiratory specimens was negative in our patient; however, a positive result was obtained from liver biopsy. Extra-pulmonary specimens and combination of different tests may increase the diagnostic sensitivity.
Due to the wide range of opportunistic infections that may exist in AIDS, diagnostic tests should be used meticulously, as its yield may be suboptimal, multiple active infections may co-exist, and they may present with overlapping or atypical signs and symptoms. Imported infections should be taken into account in patients coming from endemic areas.
FundingThis work did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approvalThe research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. The patient provided written informed consent for publication of this case report and all the accompanying images.
Conflict of interestThe authors have no conflicts of interest to declare.