Moraxella spp accounts for approximately 5% of all corneal ulcers1 and can lead to severe complications. Several investigations have focused on the characteristics of Moraxella keratitis2,3 but until recently, no cases of corneal infections due to Moraxella nonliquefaciens have been published in the medical literature. We have reported a case of corneal abscess due to M. nonliquefaciens,4 and after this, we have seen two additional cases of corneal infection due to this pathogen. In this article we describe the main characteristics of these very rare infections.
Case 1. An 85-year-old man refers red eye and intense pain. A corneal ulcer located in the inferior hemicornea with a minor epithelial defect was detected. Treatment with tobramycin plus ciprofloxacin plus cycloplegic eyedrops was started. Several corneal scrapings were taken, and they were processed for bacterial and fungal culture. No study for viruses was performed. Gram staining exhibited no microorganisms. On the second day of incubation the growth of abundant colonies of a non-hemolytic and both positive catalase and oxidase microorganism was reported in pure culture. A mass spectrometry method (Bruker Biotyper, Billerica, MA) identified the strain as M. nonliquefaciens (log score 2.024). The culture in Sabouraud agar was negative after 21 days of incubation. Susceptibility to amoxicillin-clavulanate, cefotaxime, levofloxacin, azithromycin, thrimetroprim-sulphametoxazole was demonstrated. At 3 months of follow-up neither recurrence nor complications were observed.
Case 2. A 73-year-old woman was seen due to red eye and pain. Physical examination revealed conjunctival hiperemia and a central corneal ulcer with a minor infiltrate. Treatment with vancomycin plus ceftazidime plus cycloplegic eyedrops was started. Corneal scrapings were processed in the same way that in the case 1. On the first day of incubation, the growth of abundant colonies of a microorganism of the same characteristics that in the case 1 was reported in pure culture. The mass spectrometry method also identified the strain as M. nonliquefaciens (log score 2.144). The culture in Sabouraud agar was negative after 21 days of incubation. Susceptibility was the same that in case 1. Treatment was then modified and moxifloxacin eyedrops plus ciprofloxacin in ointment was started. After 6 months, a corneal re-epithelization was demonstrated and no recurrence was observed.
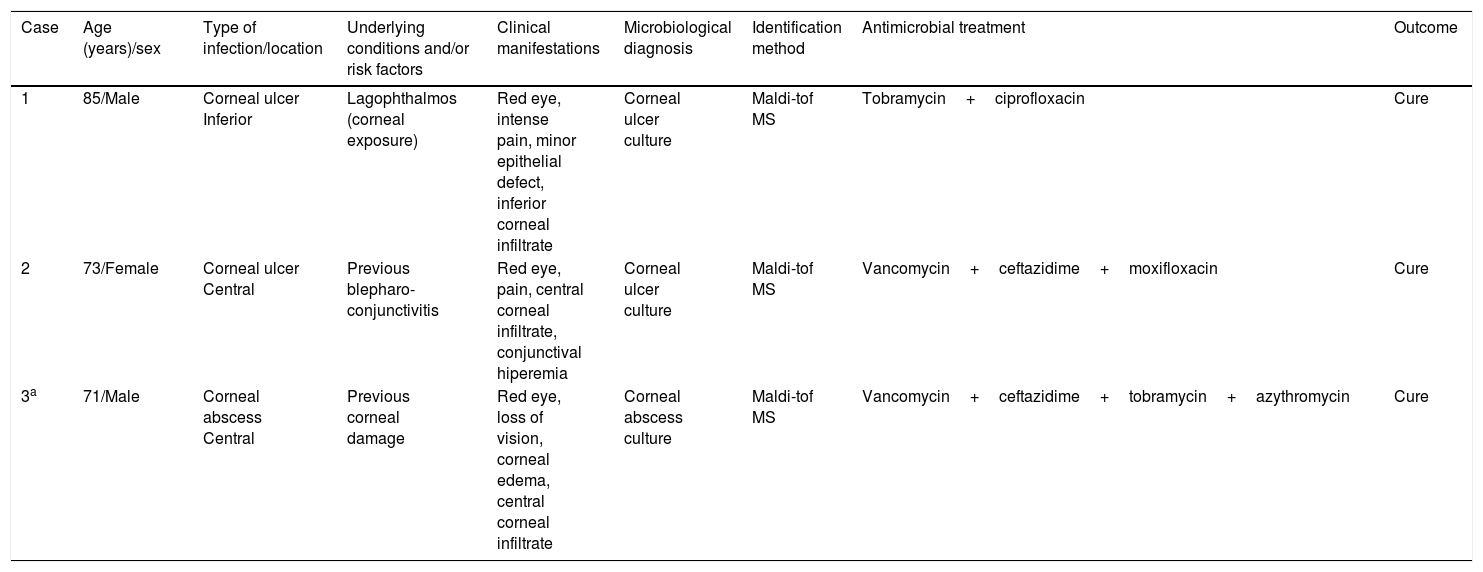
Ocular infections due to M. nonliquefaciens have been rarely described. These, have been classically associated with some predisposing factors such as chronic alcoholism, malnutrition, diabetes mellitus, and poor sanitary habits.5,6 However, our patients did not have any of these systemic factors, but they had local predisposing diseases such as corneal damage or previous corneal infection (Table 1), like recent investigations found.3,7,8 The recent scientific evidence has demonstrated that local predisposing factors may be more important that systemic factors for Moraxella keratitis.
Main characteristics of patients with corneal infection due to Moraxella nonliquefaciens.
| Case | Age (years)/sex | Type of infection/location | Underlying conditions and/or risk factors | Clinical manifestations | Microbiological diagnosis | Identification method | Antimicrobial treatment | Outcome |
|---|---|---|---|---|---|---|---|---|
| 1 | 85/Male | Corneal ulcer Inferior | Lagophthalmos (corneal exposure) | Red eye, intense pain, minor epithelial defect, inferior corneal infiltrate | Corneal ulcer culture | Maldi-tof MS | Tobramycin+ciprofloxacin | Cure |
| 2 | 73/Female | Corneal ulcer Central | Previous blepharo-conjunctivitis | Red eye, pain, central corneal infiltrate, conjunctival hiperemia | Corneal ulcer culture | Maldi-tof MS | Vancomycin+ceftazidime+moxifloxacin | Cure |
| 3a | 71/Male | Corneal abscess Central | Previous corneal damage | Red eye, loss of vision, corneal edema, central corneal infiltrate | Corneal abscess culture | Maldi-tof MS | Vancomycin+ceftazidime+tobramycin+azythromycin | Cure |
Clinically, corneal infection due to Moraxella spp has been characterized as a central ulceration with deep stromal involvement, hypopyon, and perforation. None of our patients had hypopyon or deep stromal involvement. Some investigations have shown that location of ulcer is variable2,8 and hypopion is not always present.7
The treatment of choice for M. nonliquefaciens infections has not yet been established. Moreover, no specific breakpoints have been established for species of Moraxella other than M. catarrhalis, so we have used these breakpoints for interpretation. In our three patients, different successful treatment regimens were used (Table 1), as well as in other investigations involving Moraxella corneal infections.2,3,7,8 The best outcome seems to be obtained with a multi-drug approach in most cases.3,7,8
A study reported good outcome in all patients, except two of them who showed perforation despite aggressive medical and surgical therapy,8 and tends to recover within 2 weeks in the majority of patients.3 The patients that had undergone penetrating keratoplasty for corneal perforation had a poor visual outcome.7 Our patients had a good outcome and a complete re-epithelization was demonstrated.
In conclusion, keratitis caused by M. nonliquefaciens is rare and must be suspected in patients with local predisposing factors such as corneal damage or previous corneal infection. Treatment of corneal traumas is very important in order to avoid dissemination of infection into the eye, so prompt and appropriate treatment of these lesions may help to both avoid complications and recover total vision.