The objective of antimicrobial stewardship programmes (ASP or programa pediátrico de optimización de antimicrobianos [PROA] in Spanish) is to improve patients’ clinical outcome, the use of antimicrobials, and to reduce resistance to these antimicrobials.1 After more than a decade of work with the various departments involved in the rational use of antimicrobials in children, in 2015 a paediatric ASP, called PROA-NEN, which includes neonatology, and which follows a non-imposing methodology, was officially implemented. One of the fundamental activities of persuasive ASP programmes are the prospective audits and feedback given to prescribers. At our centre, weekly on-site audits are conducted by the paediatric infectious disease specialists and microbiologists at the hospital's main clinical units (5046 in 2016; 5114 in 2017). The advisory group is made up of four members from paediatric infectious diseases, two microbiologists and one pharmacist, with each of them specialised in a specific disease. Prior to the meeting, each of the patients is reviewed through the information extracted from medical records, and an intervention strategy is agreed regarding the diagnostic and treatment procedures (whether to continue, adjust, change or suspend the treatment). During the session with the prescribers (specialists from the various units and resident doctors-in-training) this strategy was discussed and the clinic was advised on the action to be taken, receiving immediate feedback, thereby allowing for greater consensus and thus greater acceptance and adherence.
Although it is known that persuasive strategies are more accepted by clinics, there are few publications that extensively analyse the different ASP interventions, and they are particularly scarce in paediatrics.2–7
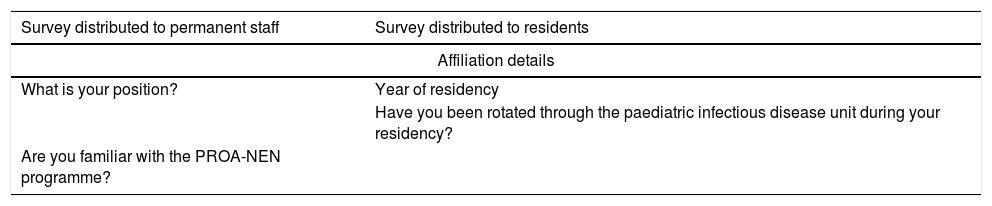
The PROA-NEN team designed a study to evaluate how the prescribers perceive the audits in order to detect possible areas for improvement and/or intervention. An anonymous survey was conducted, comprised of 18 questions, divided into four sections (Table 1): (1) affiliation; (2) evaluation of the consultation methodology: with directed responses (yes/no) and with levels of evaluation (from very unsatisfied to very satisfied: from 0 to 10); (3) evaluation of the impact of the audits on clinical decisions; and (4) evaluation of the training actions and free-response questions about suggestions for improvement.
Questionnaire to evaluate the quality of audits and training actions within the PROA-NEN framework.
| Survey distributed to permanent staff | Survey distributed to residents |
|---|---|
| Affiliation details | |
| What is your position? | Year of residency |
| Have you been rotated through the paediatric infectious disease unit during your residency? | |
| Are you familiar with the PROA-NEN programme? | |
| Evaluation of the audit methodology | |
|---|---|
| Are PROA-NEN audit sessions conducted in your department/unit? | In what % of units/departments where you have been rotated are PROA-NEN audits conducted? |
| From 0 (very poor) to 10 (very good), how would you rate the duration of the audits and the frequency with which they are conducted in your department/unit? | |
| From 0 (very poor) to 10 (very good), how would you rate the professionals that perform them? | |
| From 0 (not very) to 10 (very), how necessary do you think the presence of a microbiologist and/or a pharmacist is in the audits? | |
| Do you think that the format of the audits is appropriate? | |
| Do you think it would be better if they were conducted in digital format through the medical records? | |
| How satisfied are you overall with these audits? | |
| Evaluation of the impact of the audits on clinical decisions | |
| Do the audits affect how you issue prescriptions? | |
| From 0 (never) to 10 (always), to what extent is your prescription adjusted to that recommended by the infectious disease specialists during the audits? | |
| Do you see the conduct of audits in your daily practice as a positive thing? | |
| Did your attendance at the audits reduce your number of inter-consultations with the infectious diseases unit last year? | |
| Evaluation of the training actions and needs | |
| Did you attend any of the training actions that were conducted within the context of PROA-NEN in 2017? | |
| From 0 (not very) to 10 (very), how useful did you find them? | |
| Would you like to receive more training on antimicrobials? | |
| On which specific topics; pick a maximum of 4 | |
| Do you have any suggestions for improving the PROA-NEN audits? | |
The questionnaires were given to resident doctors (68) and specialists (87) from the centre's various paediatric sub-specialties and paediatric surgery, as well as to specialists in pharmacy and microbiology. One hundred and three professionals out of 155 took part (with a similar representation in both groups). 81.5% of specialists and 77.1% of resident doctors were familiar with PROA-NEN. 94% confirmed that audits were conducted in their department and the overall evaluation in terms of the audit methodology was 8.7 out of 10. 92% said that the on-site format of the audits was better than digital, and they all stated that the conduct of the audits was a positive thing in their daily practice. Likewise, those surveyed viewed the participation of a pharmacist and/or microbiologist in the audits positively (with scores of 7 and 9 out of 10, respectively). Regarding decision making, 92% of those surveyed stated that the audits affected their prescription of antimicrobials, and in 80% of cases the prescription was individually adjusted to that recommended.
In relation to the training actions, it was observed that only 40% of the resident doctors and 50% of the specialists had attended the PROA-NEN continuous training sessions, with those who had attended evaluating it positively (8 out of 10).
This questionnaire has allowed us to learn about the positive overall evaluation of prescribing professionals. Furthermore, we noted the significant impact of the audits on their clinical practice and the high level of adaptation of the methodology used (on-site and non-restrictive) to the specialists’ needs. Finally, points for improvement were detected in terms of the training, and it is for this reason that a transmedia and gamification-type training project is being developed for this purpose.
To conclude, we want to emphasise that, for proper implementation of a paediatric ASP with the merited level of excellence and quality, regular analysis and evaluation of the programme's interventions is essential. The unimposing, on-site audit model is adapted to the needs of the specialists in a tertiary paediatric centre in our environment.
Pere Soler Palacín: Unidad de Patología Infecciosa e Inmunodeficiencias de Pediatría, Servicio de Pediatría, Hospital Universitari Vall d’Hebron, Barcelona, Spain.
Susana Melendo Pérez: Unidad de Patología Infecciosa e Inmunodeficiencias de Pediatría, Servicio de Pediatría, Hospital Universitari Vall d’Hebron, Barcelona, Spain.
Natalia Mendoza Palomar: Unidad de Patología Infecciosa e Inmunodeficiencias de Pediatría, Servicio de Pediatría, Hospital Universitari Vall d’Hebron, Barcelona, Spain.
Aurora Fernández Polo: Servicio de Farmacia, Hospital Universitari Vall d’Hebron, Barcelona, Spain.
M. Nieves Larrosa Escartín: Servicio de Microbiología, Hospital Universitari Vall d’Hebron, Barcelona, Spain.
Carlos Rodrigo Gonzalo de Liria: Servicio de Pediatría, Hospital Universitari Vall d’Hebron, Barcelona, Spain.
Montse Pujol Jover: Unidad de Curas Intensivas Pediátricas, Hospital Universitari Vall d’Hebron, Barcelona, Spain.
Yolanda Castilla Fernández: Servicio de Neonatología, Hospital Universitari Vall d’Hebron, Barcelona, Spain.
Laura Alonso García: Servicio de Oncología y Hematología Pediátricas, Hospital Universitari Vall d’Hebron, Barcelona, Spain.
Sergio López Fernández: Servicio de Cirugía Pediátrica, Hospital Universitari Vall d’Hebron, Barcelona, Spain.
Jesús Quintero Bernabeu: Unidad Funcional de Hepatología y Trasplante Hepático Pediátrico, Servicio de Pediatría, Hospital Universitari Vall d’Hebron, Barcelona, Spain.
Núria Wörner Tomasa: Unidad de Urgencias Pediátricas, Servicio de Pediatría, Hospital Universitari Vall d’Hebron, Barcelona, Spain.
Ignacio Iglesias Serrano: Unidad de Alergia, Neumología y Fibrosis Quística Pediátrica, Servicio de Pediatría, Hospital Universitari Vall d’Hebron, Barcelona, Spain.
José Àngel Rodrigo Pendas: Servicio de Medicina Preventiva-Control de la infección, Hospital Universitari Vall d’Hebron, Barcelona, Spain.
Elisa Navarro Royo: Servicio de Medicina Preventiva-Control de la infección, Hospital Universitari Vall d’Hebron, Barcelona, Spain.
Diego van Esso Arbolave: Pediatría Territorial, Servicio de Atención Primaria Muntanya, Gerencia Territorial de Barcelona, Spain.
Maria Estrella Barceló: Área del Medicamento, SAP Muntanya, Barcelona, Spain.
Please cite this article as: Melendo-Pérez S, Fenoy-Alejandre M, Morey-Olivé M, Soler-Palacín P, grupo PROA-NEN. Evaluación de la calidad percibida en las intervenciones no restrictivas dentro de un programa pediátrico de optimización de antimicrobianos (PROA-NEN). Enferm Infecc Microbiol Clin. 2019;37:215–217.