A 5-year-old child with agenesis of the external ear canal and deformity of the left ossicular chain, was brought to the emergency department due to fever, left jaw stiffness, preauricular pain and trismus starting 24h prior. Left preauricular and left parotid inflammation were found on examination, with no otorrhoea observed in the external ear canal, which ended in a cul-de-sac. Blood tests showed leukocytosis at 15,900/mm3 with 53% neutrophils, C-reactive protein (CRP) at 175mg/L and normal amylase. The ultrasound showed parotid gland inflammation with no collections. Given the suspicion of acute parotitis, it was decided to admit the patient with intravenous amoxicillin–clavulanic acid. After 4 days of treatment, the patient improved clinically, remained afebrile and the blood tests normalised. The patient was discharged with oral amoxicillin–clavulanic acid for 10 days.
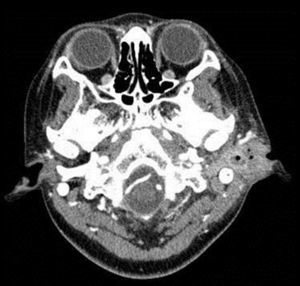
Five days after being discharged, while still under treatment with antibiotics, the patient was seen due to a recurrence of the inflammatory signs in the left parotid region and abundant purulent otorrhoea. A new left retroauricular skin fistula was observed (Fig. 1). A CT scan was performed which showed an extensive left parotid abscess, middle and external ear occupation by purulent material and a fistula communicating between the parotid abscess and the retroauricular skin (Fig. 2). A blood culture and a sample of the ear discharge were taken, and it was decided to admit the patient.
Clinical courseTreatment with intravenous amoxicillin-clavulanic acid was restarted with little response; therefore it was replaced with meropenem and the abscess was surgically drained.
Actinomyces odontolyticus was isolated in the blood culture, ear exudate and drainage material; therefore meropenem was replaced with intravenous penicillin. After one week of treatment, pain and fluctuation in the preauricular region appeared, and new parotid abscesses were observed on the imaging tests and radiological signs of left mastoiditis. The patient underwent another surgery for cleaning and debridement, fistula closure and middle and external ear reconstruction. Treatment with intravenous penicillin was maintained until 21 days were completed, and afterwards, the patient received outpatient treatment with oral penicillin for 6 months, with favourable progress and with no recurrences.
CommentsActinomyces sp. is an anaerobic gram-positive bacillus that usually colonises the oropharynx, intestines and the genital and urinary tracts. Cervicofacial actinomycosis is the most common clinical form, accounting for 50–60% of cases.1,2 It usually occurs in adults with prior lesions to the oral mucosa, infections of the gums, cavities, dental extractions, injuries or a history of recent surgery.1,2 It typically presents as cellulitis, abscesses or masses around the jaw and neck, often associated with osteomyelitis of the jaw2,3 and fistula formation. It very rarely affects the parotid glands4 or the middle ear.5 In our case, the infection was associated with a congenital deformity of the middle and external ear. The presence of nearby deformities has been described by some authors as a possible origin of infection, and it should be suspected in recurrent cases that do not present apparent oral lesions.3,6
The definitive diagnosis of actinomycosis is made via microbiological culture or viewing the bacteria in histological samples.1,2 It is difficult to isolate, as antibiotics are frequently administered beforehand, or due to coinfection with other bacteria, its slow growth, or by taking unsuitable samples for culture.1,2 The most common disease-causing species is Actinomyces israelii.1,2A. odontolyticus is rare,2,7 affecting the adult population in the reported cases.7 It is rarely isolated in blood cultures7 since only 12% of A. odontolyticus infections reported in the literature are associated with bacteraemia.7
To cure the infection and prevent recurrences, prolonged antibiotic treatment is required with high doses of penicillin for 6 to 12 months.1,2 However, in many cases, despite establishing the correct treatment, the infection tends to form a fistula and spread locally in a fast and aggressive manner,1,2 requiring an additional surgical approach.1,2 Moreover, in cases such as ours with mastoid involvement (a clinical form with higher mortality),2,5 there is a risk of spreading to the CNS.5
Thus, it is essential to establish a suspected diagnosis early. Nevertheless, it is unusual to consider actinomycosis in the differential diagnosis of cervicofacial infections in children,8 and actinomycosis was only suspected in 10% of paediatric cases when establishing the initial diagnosis.8
Our case is exceptional since it is an infection by A. odontolyticus in a paediatric patient,1,6 with associated bacteraemia, over a congenital deformity, and affecting the parotid gland and middle ear. However, the clinical progression is typical for this bacteria, therefore it is important to consider actinomycosis in recurrent, chronic, suppurative, cervicofacial processes in children.
Conflict of interestsThe authors declare that there is no conflict of interest with regards to the published article.
Please cite this article as: Blanco-Sánchez AI, Méndez-Echevarría A, Alonso-Quintela P, García-Perea A, Baquero-Artigao F. Escolar con fiebre, inflamación parotídea, otorrea y fístula retroauricular. Enferm Infecc Microbiol Clin. 2017;35:54–55.