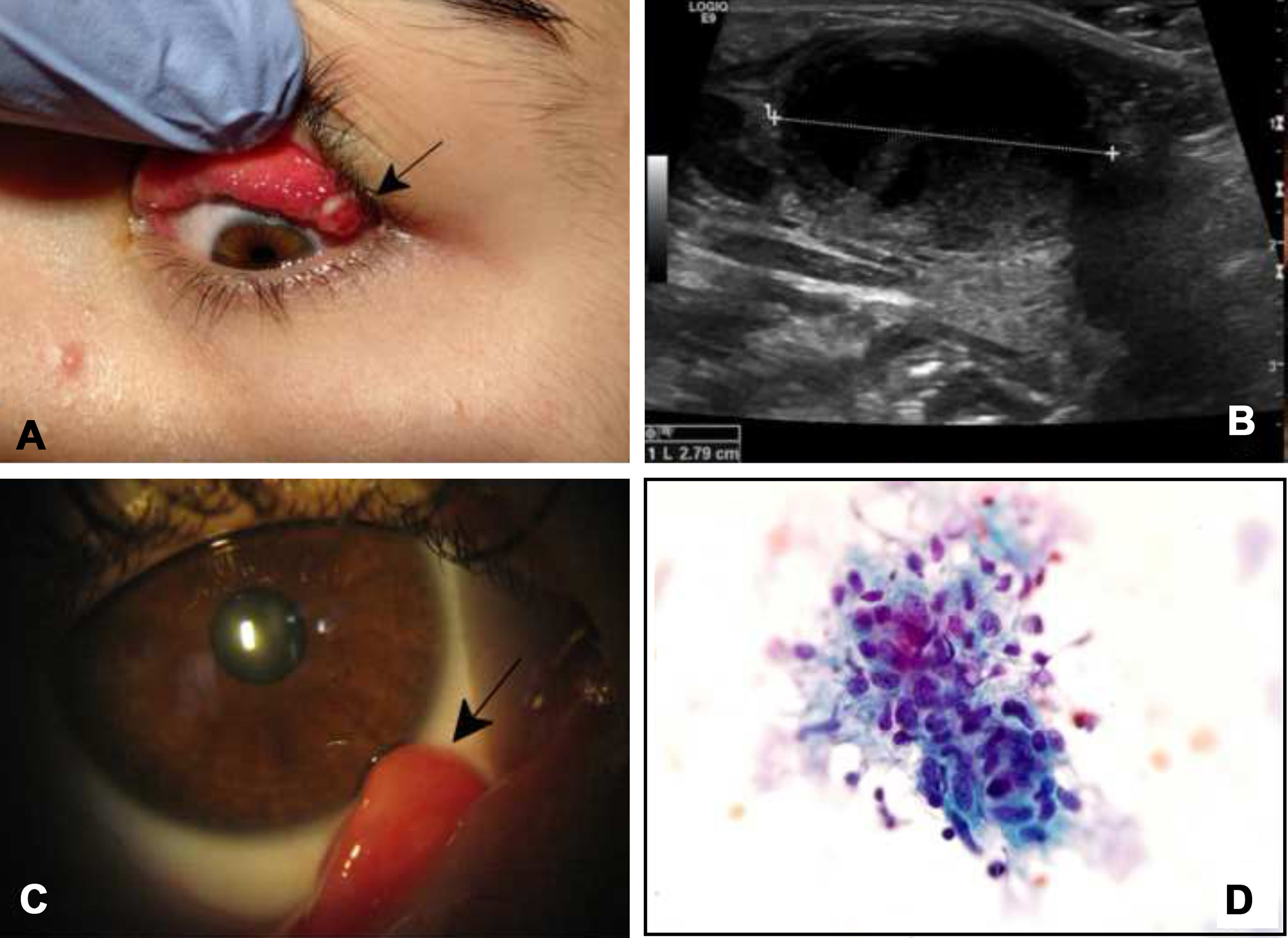
A 20-year-old patient who referred with a two-week evolution of pink eye, tearing and a foreign body sensation. This was also accompanied by the appearance of an ipsilateral painful preauricular mass. On examination, follicular conjunctivitis was identified, accompanied by an upper tarsal granulomatous lesion (Fig. 1A), with a mobile and painful preauricular adenopathy also present. Given the clinical suspicion, the patient was asked about any history consistent with the condition and according to what they told us, they sleep with a small cat. General analytical testing and indirect immunofluorescence (IIF) for Bartonella were requested.
(A) Image showing papillary follicular conjunctivitis next to a granuloma with an ulcerated surface in the upper tarsal conjunctiva of the left eye. (B) Ultrasound of case 2 wherein a 2.79cm adenopathy is identified with small foci of necrosis. (C) Slit-lamp photograph showing a conjunctival granuloma protruding from the bottom of the lower conjunctival sac of the right eye. (D) Biopsy of a submandibular adenopathy wherein clustered epithelioid histiocytes suggestive of granulomatous lymphadenitis are identified.
A 3-year-old girl, evaluated for a conjunctival lesion in the right eye and foreign body sensation. According to the patient, she is being studied for painful submandibular adenopathy (Fig. 1B) for which surgical debridement and biopsy have been performed. She presented a right lower tarsal granuloma, with no other findings (Fig. 1C), and a biopsy of the adenopathy revealed the presence of granulomatous lymphadenitis (Fig. 1D). We did not find anything, despite a detailed epidemiological history of contact with animals.
EvolutionIn case 1, the IIF was positive for anti-Bartonella henselae IgM (titre 1/256) and IgG (1/320), indicative of recent infection. Empirical treatment with macrolides was started (azithromycin 500mg/24h/for 5 days) since follow-up was not possible.
Case number 2 presented serology positive for B. henselae (IIF IgM 1/512 and IgG 1/40). Therefore, treatment with azithromycin and amoxicillin/clavulanic acid, adjusted for weight, was started.
In both cases the evolution was favourable.
Final commentsParinaud's oculoglandular syndrome is one of the ocular manifestations of what is known as cat-scratch disease (CSD) caused by B. henselae, though it is not the only cause.1 It is estimated that it represents around 6% of cases of CSD and presents a seasonal pattern, predominating in autumn and winter.2,3 It occurs as a unilateral follicular conjunctivitis frequently associating a tarsal focal granulomatous lesion with necrosis or ulceration and regional adenopathies that may be accompanied by mild general symptoms.4–7 It is typically referred to as a unilateral ocular redness with non-purulent epiphora, eyelid oedema and conjunctival lesion along with painful regional adenopathy.3
B. henselae is a gram negative bacillus whose culture is complex, but can be done in enriched media with times of up to four weeks. Likewise, Warthin–Starry staining can be used to demonstrate the presence of the pathogen in blood vessel or lymph node samples.8,9 In immunocompetent patients B. henselae produces necrotizing granulomas and microabscesses, while in immunosuppressed patients the response tends to be vasoproliferative in nature.8
Infection in humans can go unnoticed, and in some symptomatic cases the epidemiological history of contact with animals may be absent. Clinical suspicion in the presence of positive IgG and IgM antibody titres by IFI is the most common method to establish the diagnosis, although molecular biology techniques have been developed that have a higher specificity.9 As for serology, cross-reactions that occur with other species of Bartonella, especially Bartonella quintana, and which limit its accuracy when identifying the species involved must be taken into account.8
Antibiotic treatment in immunocompetent patients is controversial and should be individualized based on the degree of involvement and the characteristics of the patient, although it is always worthwhile in immunosuppressed patients or cases with associated intraocular involvement.9 Both erythromycin and doxycycline have shown very favourable responses, and the duration of treatment usually ranges from two to six weeks in immunocompetent patients, and up to four months in immunosuppressed patients.1 Azithromycin at a rate of 500mg/24h/for 5 days has been shown to be a safe and effective alternative.10
We believe that an adequate knowledge of the disease allows treatments and diagnostic tests that generate iatrogenesis and unnecessary concern in patients and their families to be avoided. Observation in mild cases with ophthalmologic examinations may be more than sufficient in most cases, although the treatment should be individualized based on the characteristics of the patient. In cases where treatment with azithromycin 500mg/24h/for 5 days is considered to be indicated, it has proven to be a valid regimen.
FundingThis study has received no specific funding from public, private or non-profit organizations.
Please cite this article as: Cuadrado MM, del Barrio LT, Pedreiro SM, Guevara KG. Conjuntivitis granulomatosa en 2 pacientes jóvenes. Enferm Infecc Microbiol Clin. 2020;38:238–239.