Intravitreal therapy is very frequent in ophthalmological practice. Every time the patients receiving intravitreal treatment is being increased which means the rise of its inherent complications. There is few information about local infections at the injection site.
A case report is presented telling a Mycobacterium chelonae scleritis infection after anti VEGF intravitreal treatment. There is only one previous case reported and its knowledge is essential to establish an adequate and early specific treatment to prevent subsequent complications.
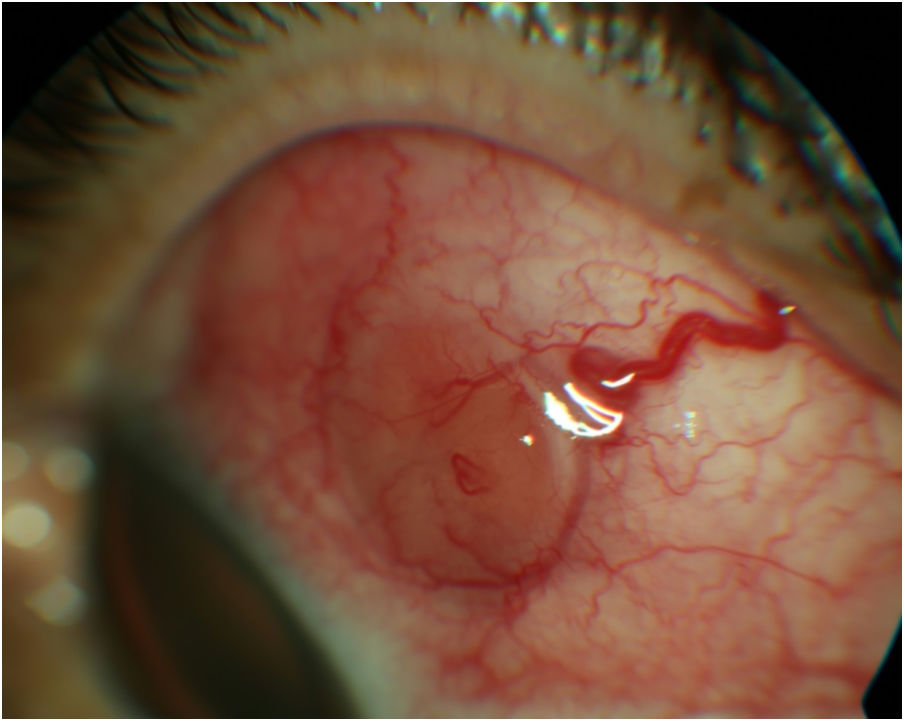
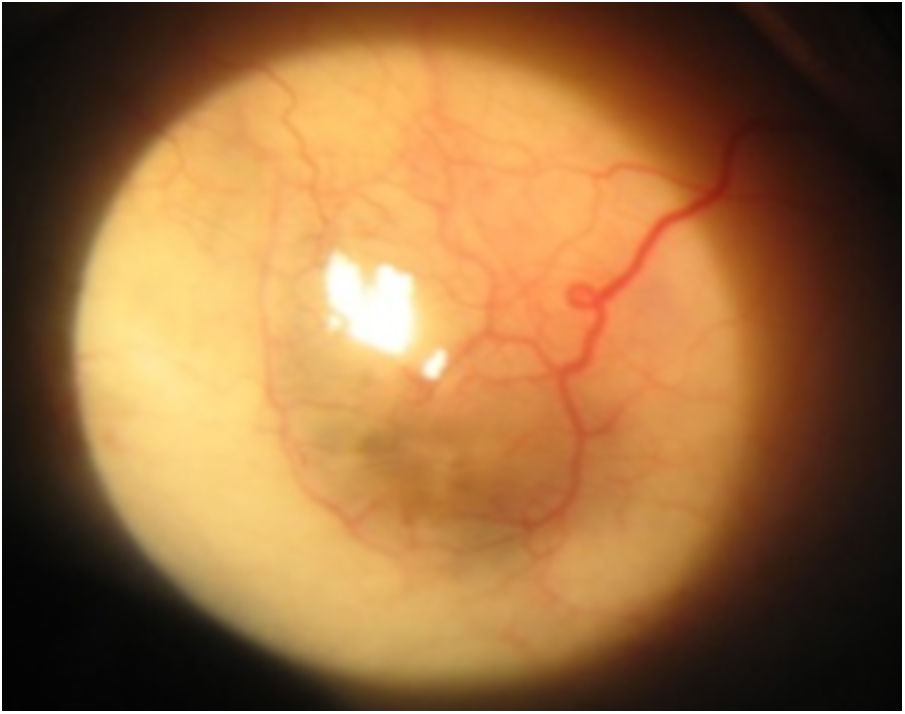
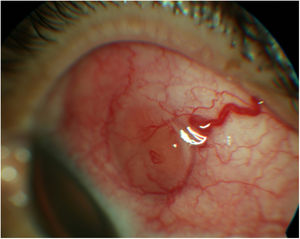
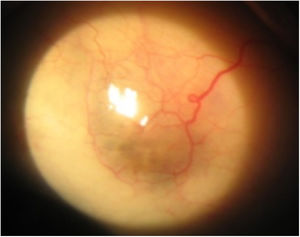
Case reportA 57-year-old female with monthly intravitreal therapy due to an AMD in the left eye presented with severe pain 1 week after the last visit. Visual Acuity was 20/25 (Snellen) in the right eye and 20/32 in the left eye. Slit-lamp examination revealed a scleral abscess at upper temporal quadrant in the left eye corresponding to the last injection site (Fig. 1). Fundoscopy revealed a retinal protrusion through the vitreous cavity beneath the abscess. A microbiological culture was performed with M. chelonae growth. Topical treatment with tobramycin and amikacin, and oral moxifloxacine was initiated and continued during 6 months. After, the inflamation and infection disappeared remaining a loss of scleral thickness (Fig. 2).
Intravitreal therapy is a common minimally invasive procedure to treat a wide spectrum of pathologies in Ophthalmology. The most common complications related to the procedure are corneal abrasions, retinal detachments, conjunctival hemorrhages, endophthalmitis and damage the lens.1 Scleritis and scleral abscesses associated with intravitreal injections are infrequent.2
In our literature revision we have found only 2 cases of M. chelonae scleral infection due to an intravitreal injection reported. One of them had culture negative and the M. chelonae infection was only suspected.3 On the other hand, Ilya et al. reported a case of a scleral abscess due to M. chelonae culture positive with similar clinical features to our case. It appears as an inflammatory node that may be complicated with an abscess at puncture area (Fig. 1).
M. chelonae is a nontuberculous mycobacterium (NTM) which may have a long incubation period. It commonly produces skin and soft tissues infections and the eye is the second most frequently organ involved. The organism is known to cause dacryocistitis, canaliculitis, conjuntivitis, scleritis, endophthalmitis and keratitis.4 Scleritis and scleral abscesses have been reported as complications after retinal surgery, but M. chelonae scleral abscesses associated with intravitreal injections are exceedingly rare.2 This bacterium survives in nonnutrient and high temperature solutions. Its biochemical characteristics are growth in MacConkey positive arylsulphatase medium in 3 days, negative iron uptake and negative nitrate reduction test.5 It resists surface disinfectants commonly used in hospital sterilization units and characteristically forms biofilms Water and aqueous solutions are the greatest vector for transmission to humans. Contamination of surgical material has also been described as one of the main sources of emergence of M. chelonae.6
Collecting microbiological culture is capital to determinate the antibiotic sensitivity which leads to an adequate therapeutic strategy. This is especially significant in immunodeficient people because the infection in these patients become more usually systemic and severe. In nonimmunodeficient people treatment between 4 weeks and 6 months is required, in our experience 6 months topical and oral therapy was necessary to eradicate the infection (Fig. 2).
FundingNone declared.
Conflict of interestNo conflicting relationship exists for any author.