An 18-year-old spanish female patient was admitted to our hospital in December 2017 after 2 days of fever, caugh and dyspnea. The patient had no clinical relevant history, no history of recent travel and a completed vaccination calendar. The patient accomplished sepsis clinical criteria, and examination revealed no neurologic findings or skins lesions. Laboratory findings were leucopenia, coagulopathy and elevation of acute phase reagents. Torax X-ray showed a bilateral infiltrate. The patient evolved to acute respiratory failure, which required admission to our Intensive Care Unit for respiratory support with Optiflow. Empirical antimicrobial treatment with meropenem, levofloxacin and oseltamivir was started after collection of blood and urine cultures and nasopharyngeal exudate for PCR testing for Influenza viruses.
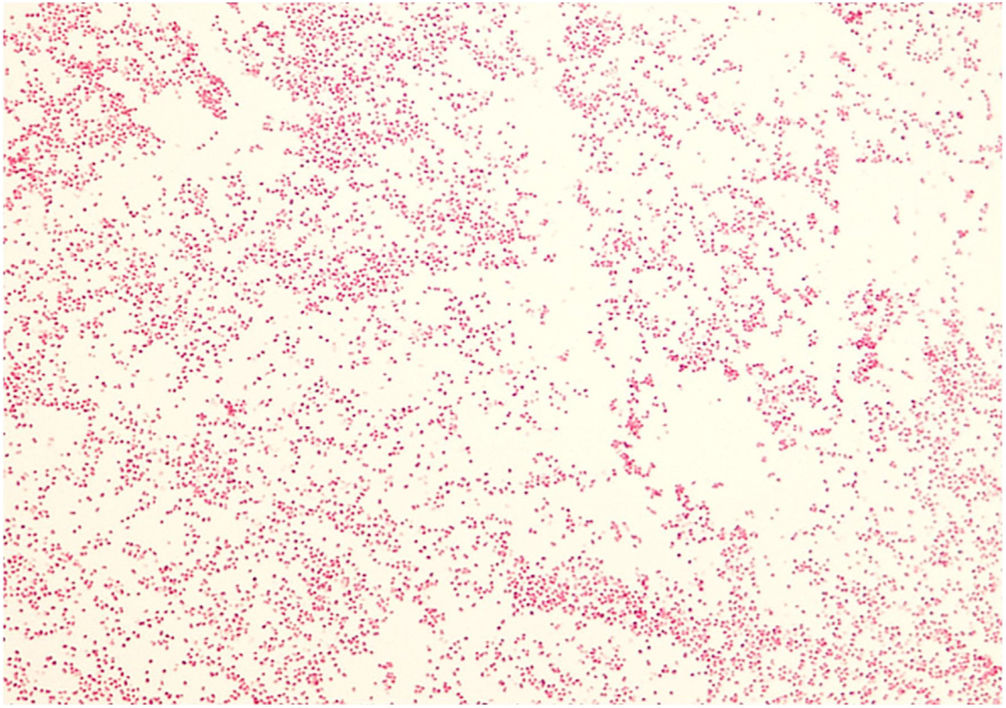
Urine and nasopharyngeal samples were negative. After 15h of incubation, blood cultures were positive and the Gram stain showed Gram-negative cocci in pairs (Fig. 1). The bottles were subcultured onto Columbia sheep blood and chocolate agar plates and incubated at 35°C in 5% CO2. With the suspicion of meningococcemia, subculture was also made onto Martin Lewis agar and incubated at 35°C in CO2. After 24h of incubation, all agar plates were grown, showing small, non-hemolytic, brilliant, grayish colonies. The oxidase test was positive and the biochemical identification panel (Api NH, Biomérieux) revealed that the isolate fermented glucose and maltose and was proline arylamidase and gamma-glutamyl transferase positive. Agglutination for capsular antigens was made (Directigen Meningitis Combo Test, Biomérieux), confirming that the isolate was Neisseria meningitidis serogroup C/W. The strain was susceptible to Cefotaxime (MIC≤0.016μg/mL). Clinicians were informed and the patient underwent targeted therapy with Cefotaxime at a dose of 2g/8h for 7 days, with favorable outcome. After 12 days of hospitalization, the patient was discharged from our hospital without any clinical consequence of the infection.
The strain was sent to the Reference Laboratory for Meningococci (National Centre of Microbiology, Institute of Health Carlos III, Majadahonda, Spain) for confirmation and characterization. The isolate was identified by using slide agglutination with specific polyclonal antibodies as N. meningitidis serogroup W, and molecularly characterized by sequencing variable regions of the PorA protein gene1 as genosubtype P1.5,2 (PorA VR1:5, VR2:2).
Invasive meningococcal disease (IMD) is a severe and life-threating illness, associated with different serogroups of N. meningitidis. In Spain, all IMD cases must be notified through the National Network of Epidemiological Surveillance, due to its high morbidity and mortality, as well as the clinical consequences of the infection. The disease is seasonal, being more frequent in the winter months. The epidemiological patterns are different depending on the involved serogroup.2 Regarding the incidence of IMD, 3121 cases were reported in 2015 in EU/EEA countries (0.6 cases per 100000 population), being the most frequent the serogroup B (61%), followed by serogroup C (14%). There is a continuous decreasing trend in the incidence of the mentioned serogroups. However, IMD by other serogroups that were rare years ago in Europe such as W and Y, are now increasing, achieving a rate of 11% for W and 10% for Y of the total number of cases in 2015.3–7 Thus, the implementation of the quadrivalent conjugate vaccination (A, C, Y and W) has been proposed in countries with increasing rates of IMD by serogroup W such as United Kingdom, Greece, Austria and Czech Republic.8
In Spain we have attended a similar scenario: on the one hand a decrease on the incidence of IMD by serogroup C and B. On the other hand, the number of IMD due to non-frequent serogroups (W and Y) has also increased (8.2% of W and 5.2% of Y in 2015–2016 season).9
These serogroups are nowadays considered as emerging and they should be considered in patients with clinical suspicion of meningococcal infection. The possibility of quadrivalent conjugate vaccine implementation in Spain should be evaluated in response to the increasing risk of IMD cases by serogroup W.10
This case report illustrates the emerging importance of these local-acquired non-B/C meningococcal infections which have to be considered as a differential diagnosis in patients with either sepsis of respiratory origin with or without neurological or skin findings. In addition, it could serve to point out the potential benefit of implementing the quadrivalent vaccine in Spain. However, prospective multicentric studies are needed to establish the incidence of these emerging serogroups and also to assess the convenience of the quadrivalent vaccine implementation in Spain, as it has already been implemented in other EU/EEA countries.
We thank Rebeca Bailén for her help with the preparation of the manuscript.