Pyomyositis is a bacterial infection of the striated muscle, which usually develops into a muscle abscess. It mainly affects the large muscles of the lower limbs,1,2 and its location in the obturator internus muscle (OIM) is exceptional, little documented and a real diagnostic challenge.
We present the case of a 15-year-old adolescent boy, who came to the Emergency Department with a one-week history of fever, pain in the right gluteal region and a limp. He did not report any trauma, recent intense physical exercise or any previous infectious process. On examination, an antalgic position was observed with the right hip in flexion, external rotation and abduction. Blood tests showed 70.6% of neutrophils without leukocytosis (7.6·10^9/l) and CRP of 8.9mg/dl. X-rays of the pelvis and hips were performed without relevant findings and an ultrasound of the hip revealed joint effusion. The patient was admitted with clinical suspicion of septic arthritis.
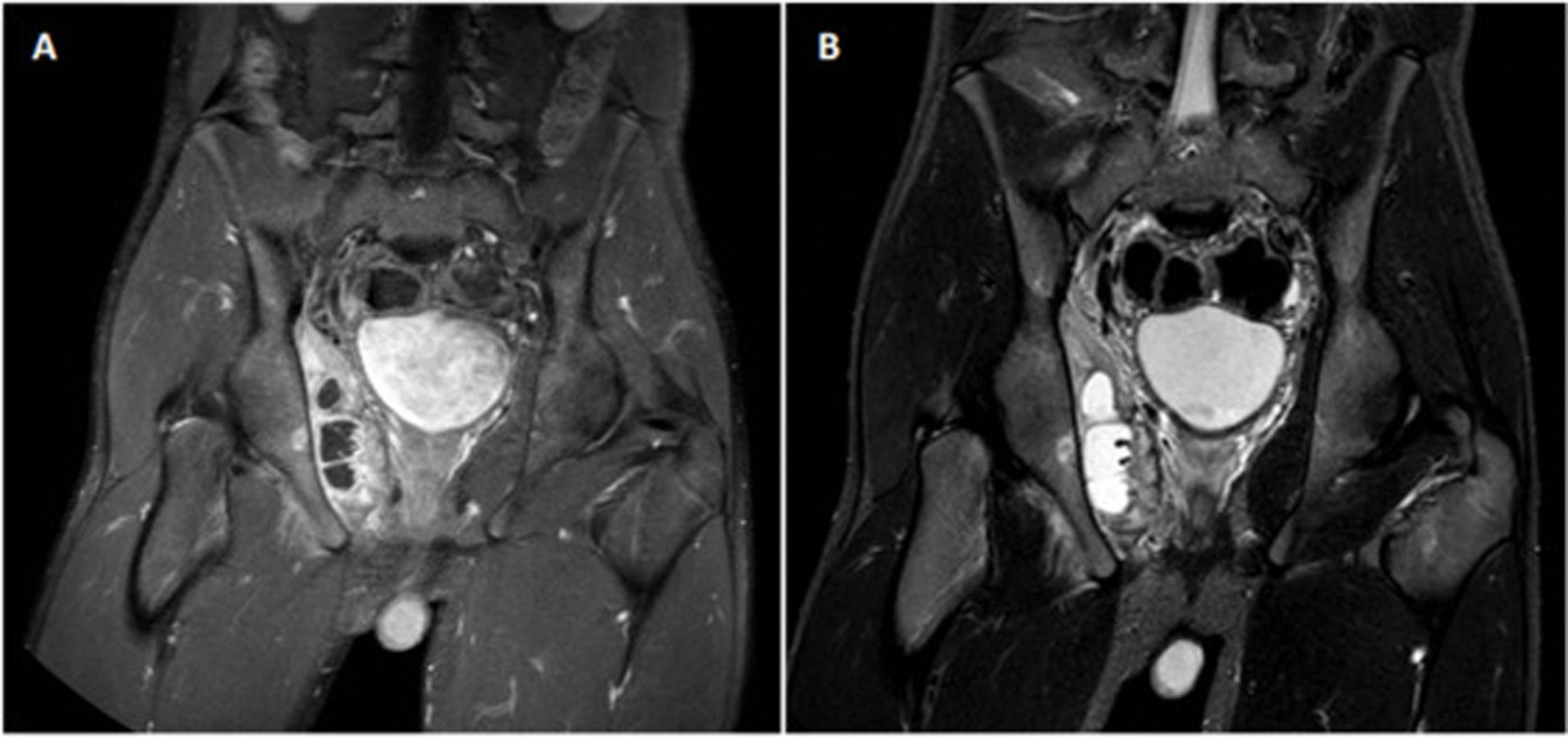
Arthrocentesis was performed, with negative gram stain and culture results. Blood cultures were positive for methicillin-sensitive Staphylococcus aureus (MSSA), and treatment with intravenous cloxacillin was started. An abdominal ultrasound study was completed, which ruled out appendicitis, and an MRI of the hip showed oedema of the peritrochanteric soft tissues without signs of septic arthritis. A follow-up MRI repeated five days later revealed an abscess measuring 6×1.5×5.5cm in the OIM with probable associated pelvic osteomyelitis (Fig. 1). Ultrasound-guided drainage of the collection was performed, obtaining 12 cm3 of purulent fluid and culture isolation of MSSA (identical sensitivity to blood cultures). In turn, antibiotic treatment was extended with vancomycin and clindamycin, after withdrawing cloxacillin.
The clinical response and test results were favourable, but without complete resolution in successive follow-up MRIs, so it was decided to prolong parenteral treatment for six weeks, the first four weeks in hospital, and at discharge, two more weeks with weekly dalbavancin combined with oral clindamycin.
Primary pyomyositis is an infrequent condition, which is observed mainly in tropical climates, although in recent decades it has notably increased in our setting, associated above all with situations of immunosuppression.2–4
Its pathogenesis is not completely known, but it has traditionally been associated with local trauma (15-50%) or strenuous physical exercise.1–5 It usually originates from haematogenous dissemination, with gram-positive bacteria being responsible for practically all cases, and Staphylococcus aureus being the most frequent microorganism.2,4
Obturator internus pyomyositis (OIP) is an extremely rare condition of which few cases have been described in the literature. However, its incidence has been increasing in recent years.3,5 It is more common in children,1,5 and usually manifests with fever, pain in the hip or thigh, limp and antalgic position with the hip in flexion, external rotation and abduction.1,5 In half of the cases, it is complicated by infection of adjacent muscles or pelvic osteomyelitis,1,5 as occurred in our case.
Diagnosis is usually late due to clinical and analytical non-specificity,3 or as a result of being confused with other osteoarticular or intra-abdominal pathologies, especially septic coxarthritis.1,3,6 Ultrasound is useful as a diagnostic approach but the gold standard is MRI, which has great sensitivity and specificity, especially in early stages.3,6,7 It is also important to perform blood cultures and cultures of material drained from the abscess.
The duration of treatment is not well defined and will vary depending on the severity and response. Patients should be covered empirically for Staphylococcus aureus (and if immunocompromised also for gram-negative bacteria),2,7 initially intravenously, with subsequent oral sequencing. In addition, if an abscess appears it should be drained, with percutaneous drainage being preferable to surgery.2 The usefulness of the new antistaphylococcal antibiotics, specifically dalbavancin, should be highlighted due to its convenient weekly intravenous dosage, which allows it to be administered on an outpatient basis. Although there is little experience in paediatric patients, it appears to be safe and effective,8 and given the higher incidence of this pathology at an early age, it has been interesting to see the excellent results obtained with our patient.
Therefore, we are facing an underdiagnosed disease, in which clinical suspicion will be fundamental, so when faced with a patient, especially a paediatric patient, who presents with fever, limp and a hip ultrasound that is normal or suggestive of septic arthritis, we should always suspect OIP and expand the study with MRI. In this way, we will avoid therapeutic delays and devastating complications, since the only prognostic factor for complete functional recovery is early diagnosis and treatment.3
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Martínez-Fernández S, Vázquez-Temprano N, Diz J. Piomiositis del músculo obturador interno: no todo es artritis séptica. Enferm Infecc Microbiol Clin. 2022;40:400–401.