A 68-year-old woman visited her primary care physician due to a lesion in her right index fingernail for the past three months. The lesion was painful and affected the proximal nail bed. It showed no change in colour and was unrelated to prior trauma (Fig. 1). In addition, it was accompanied by neither regional lymphadenopathy nor systemic symptoms. Her personal history included poorly controlled diabetes mellitus type 2 in the context of morbid obesity having led to gastroparesis, as well as retinopathy and polyneuropathy. She had not recently travelled abroad, and she did not have any pets.
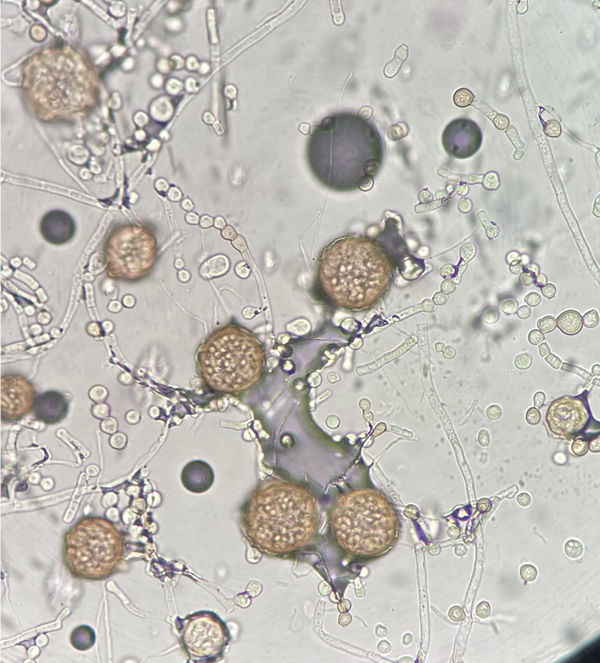
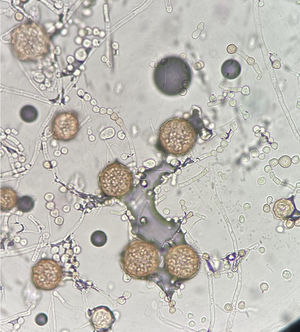
As onychomycosis was suspected, following cleansing with 70% ethanol, a sample was collected from the deep zone, close to the nail matrix, for mycological examination and seeded in Sabouraud chloramphenicol agar (Becton Dickinson [BD], Heidelberg, Germany) and in Mycosel agar (BD). The patient was prescribed treatment with itraconazole 200 mg every 12 h the first week of the month for three months1. After a week of incubation of the culture media at 30 °C, the growth of several colonies of a filamentous fungus was seen in the Sabouraud chloramphenicol agar. The colonies had a velvety texture; from the top, they were greyish-violet at the centre and whitish on the periphery, and from the bottom, they were reddish-brown (Fig. 2). Microscopic examination of the colonies revealed hyaline hyphae featuring conidiophores with chains of smooth, pyriform conidia with a truncate base and round cleistothecia with an intense honey colour (Fig. 3). Based on these characteristics, the fungus was identified as Monascus ruber2. Morphological identification was confirmed by means of DNA extraction, amplification and subsequent sequencing of the conserved internal transcribed spacer (ITS) regions using ITS4 and ITS5 primers3. The sequence obtained was analysed by means of comparison with those deposited in two public databases, GenBank (United States National Center for Biotechnology Information [NCBI], http://www.ncbi.nlm.nih.gov) and MycoBank (http://www.mycobank.org), yielding similarities to the Monascus ruber sequence of 99.61% and 100%, respectively.
The patient returned for a follow-up visit two months later, wherein less dystrophy and nail plate growth with a healthy appearance were observed. Given the patient's favourable clinical course and poor drug tolerance due to gastrointestinal discomfort, a decision was made to stop her antifungal treatment.
Closing remarksOnychomycosis is a nail infection caused by dermatophytes, non-dermatophytic filamentous fungi and yeasts. Among these causal agents, dermatophytes are the most common. There are several risk factors such as diabetes mellitus, immunosuppression and ageing; in the latter, abnormalities in peripheral circulation, difficulties with personal hygiene, sedentary lifestyle and slower nail growth facilitating fungal invasion are common4. Onychomycosis caused by non-dermatophytic fungi is uncommon, yet medically significant given its challenging diagnosis and treatment. These fungi are found in nature as soil saprophytes and plant pathogens. They exhibit rapid growth and a universal distribution. Notable examples of non-dermatophytic fungi that cause onychomycosis are Scopulariopsis spp. and Fusarium spp., followed by species from the genus Aspergillus5,6. Monascus ruber is an ascomycete belonging to the family Monascaceae that was recently identified as a causal agent of onychomycosis in two patients, one from India and one from Morocco7,8. Our case is the first one reported in Spain and we believe it must be taken into account as a possible emerging cause of onychomycosis in this country; therefore, we feel it is useful to recognise its macroscopic and microscopic characteristics. While the importance of this condition is often underestimated, infected nails act as a reservoir for infection, which in immunosuppressed patients can cause serious systemic infections. Antifungal treatment of onychomycosis is not simple, as long treatment periods are needed, especially in cases of extensive involvement. A lack of immediate satisfactory effects and the side effects associated with the drugs used result in low rates of compliance. Furthermore, said side effects sometimes require treatment suspension, as in our patient9,10. In both our case and the two cases reported in the literature, infection with Monascus ruber successfully resolved.
FundingNo funding was received for this study.
Conflicts of interestThe authors declare that they have no conflicts of interest.
The authors would like to thank Dr. Javier Pemán for his help in reviewing the draft article.
Please cite this article as: Valentín-Martín A, Hernández-Pérez N, Romero-Noreña A, Molina-Moreno JM. Onicomicosis de rara etiología. Enferm Infecc Microbiol Clin. 2022;40:330–331.