Gordonia species are known to be opportunistic human pathogens causing secondary infections. We present the second case in the world of endocarditis caused by Gordonia bronchialis and a review of all the cases of endocarditis caused by Gordonia spp.
MethodsThe identification was performed by matrix-assisted desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS) and 16S rRNA gene sequencing were performed to confirm the identification. Antimicrobial susceptibility was performed by MIC test Strip on Mueller-Hinton agar supplemented with 5% defibrinated sheep blood according to Clinical and Laboratory Standards Institute.
ResultsPacemaker-induced endocarditis due to Gordonia bronchialis infection was determined in an 88-year old woman. The patient was treated with ceftriaxone and ciprofloxacin until completing 6 weeks from the pacemaker explant with a good evolution.
ConclusionThe case presented supports the pathogenic role of Gordonia bronchialis as an opportunistic pathogen and highlights the high risk of suffering infections caused by environmental bacteria.
Las especies de Gordonia son patógenos humanos oportunistas que causan infecciones secundarias. Presentamos el segundo caso en el mundo de endocarditis causada por Gordonia bronchialis, así como una revisión de todos los casos de endocarditis causados por Gordonia spp.
MétodosLa identificación fue realizada mediante espectrometría de masas MALDI-TOF MS, y se confirmó mediante secuenciación del gen 16S rRNA. La susceptibilidad antimicrobiana se realizó mediante tiras reactivas MIC en agar Müller-Hinton suplementado con un 5% de sangre ovina desfibrinada, conforme al Clinical and Laboratory Standards Institute (CLSI).
ResultadosLa endocarditis del marcapasos debido a infección por Gordonia bronchialis se encontró en una mujer de 88 años. La paciente fue tratada con ceftriaxona y ciprofloxacina hasta completar el periodo de 6 semanas desde el explante del marcapasos, con buena evolución.
ConclusiónEste caso respalda el rol patogénico de Gordonia bronchialis como patógeno oportunista, subrayando el alto riesgo de padecer infecciones causadas por bacterias ambientales.
Infective endocarditis is a serious disease with a high mortality in the short and long terms. A special situation of endocarditis that has grown in parallel with the more frequent use of implantable defibrillator, cardiac resynchronization therapy and pacemaker implantation is infection developed on these devices 1.
Members of the genus Gordonia are aerobic, catalase-positive, Gram-positive, nonmotile, nocardioform actinomycetes that are weakly acid-fast. The name for this genus, initially called Gordona, was chosen by Tsukamura in 1971 to pay tribute to the American bacteriologist Ruth E. Gordon 2.
Gordonia genus comprises 39 different species that are recognized for symbiotic associations with multiple hosts allowing its use in bioremediation. Some Gordonia species (including Gordonia bronchialis) isolated from clinical specimens are known to be opportunistic human pathogens causing secondary infections in immunocompetent and immunosuppressive individuals 3.
Here, we present the second case in the world of endocarditis caused by Gordonia bronchialis in a patient with implanted pacemaker. Our main purpose is to show our experience and describe all the cases published to date of endocarditis caused by Gordonia spp.
Material and methodsThe identification was performed by matrix-assisted desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS) (Maldi Biotyper® Bruker Daltonics) and 16S rRNA gene sequencing were performed to confirm the identification. The DNA was extracted using the PrepMan DNA Kit method (Applied Biosystems,) following the manufacturer's recommendations. Bacterial universal PCR was performed systematically on sample with primers 16S-F (5′-AGA GTT TGA TCC TGG CTC AG-3′) and 16S-R (5′-ACG GCT ACC TTG TTA CGA CTT-3′), producing an amplicon of approximately 1500 base pairs. The sequences obtained were compared with those stored in GenBank using BLAST software (http://www.ncbi.nlm.nih.gov/blast).
Antimicrobial susceptibility was performed by MIC test Strip (Liofilchem®) on Mueller-Hinton agar supplemented with 5% defibrinated sheep blood according to Clinical and Laboratory Standards Institute (CLSI) criteria for aerobic actinomycetes 4
Case reportAn 88-year old woman with chronic atrial fibrillation developed an atrioventricular block 20 years ago, with the implantation of a pacemaker. Generator was replaced in 2005 and 2018. One month after the second exchange, the patient began with erythema and itching on the generator wound and spontaneous drainage of hemopurulent material, exudate from the surgical wound was cultivated, growing a Gram-positive bacilli identified as Gordonia bronchialis beginning treatment with ciprofloxacin. The patient undergoes a transthoracic echocardiogram without signs of infective endocarditis.
Given the persistence of signs of local infection and fever, the patient undergone a pace-maker and electrodes (located in right ventricle) exchange surgery. The explanted pacemaker (generator, pacemaker pocket and pacemaker leads) was sent to the Microbiology Department. Next day, the patient has fever so blood cultures and a new transesophageal echocardiogram was performed, showing vegetations in the tricuspid septal veil and pacemaker electrode, so pace-maker explant was performed by cardiac surgeon, requesting cultures of the pacemaker.
Aerobic, anaerobic and fungal culture was performed and there was growth of Gordonia bronchialis (except in the generator) after 48h of incubation at 37°C in blood and chocolate agar. Given the isolation of Gordonia in the first explanted system, it was decided to extend the incubation time of blood cultures from 5 days to 14 days being positive at 11 days and 18h for Gordonia bronchialis. So it was a pacemaker-associated endocarditis, ceftriaxone 2g and ciprofloxacin 400mg/12h were combined. The second pacemaker explanted culture was negative.
Control blood cultures were performed at 72h, being negative. Intravenous treatment with ceftriaxone and ciprofloxacin was maintained until completing 6 weeks from the pacemaker explant.
Upon discharge, a new transthoracic echocardiogram was performed in which no endocarditis signs were observed. Since the patient was aged, dependent for basic activities and no atrial-block or bradiarrythmia was observed in subsequent medical visits so no pace-maker implant took place. The patient remained stable, presenting progressive normalization of acute phase reactants, asymptomatic and without presenting recurrences until the present. No control blood culture was performed after the resolution of clinical presentation.
The identification of the microorganism by MALDI-TOF resulting in Gordonia bronchialis with a score of 1.68. Identification was repeated with previous extraction with ethanol-formic recommended by the manufacturer, improving to 2.08 score. The sequence was 99% identical to Gordonia bronchialis type strain DMS 43247 using the NCBI 16SrRNA gene database.
The strain was sensitive to all the antibiotics tested (amoxicillin-clavulanate, ceftriaxone, ciprofloxacin, imipenem, tobramycin, amicacin, linezolid and trimethoprim-sulfamethoxazole).
DiscussionGordonia bronchialis is an emerging opportunistic pathogen widely distributed in the environment. The genus Gordonia is able to form biofilm by producing gordonan, and acidic cell aggregation-inducing polysaccharide and consequently is responsible for persistent infections and need for prolonged treatments5.
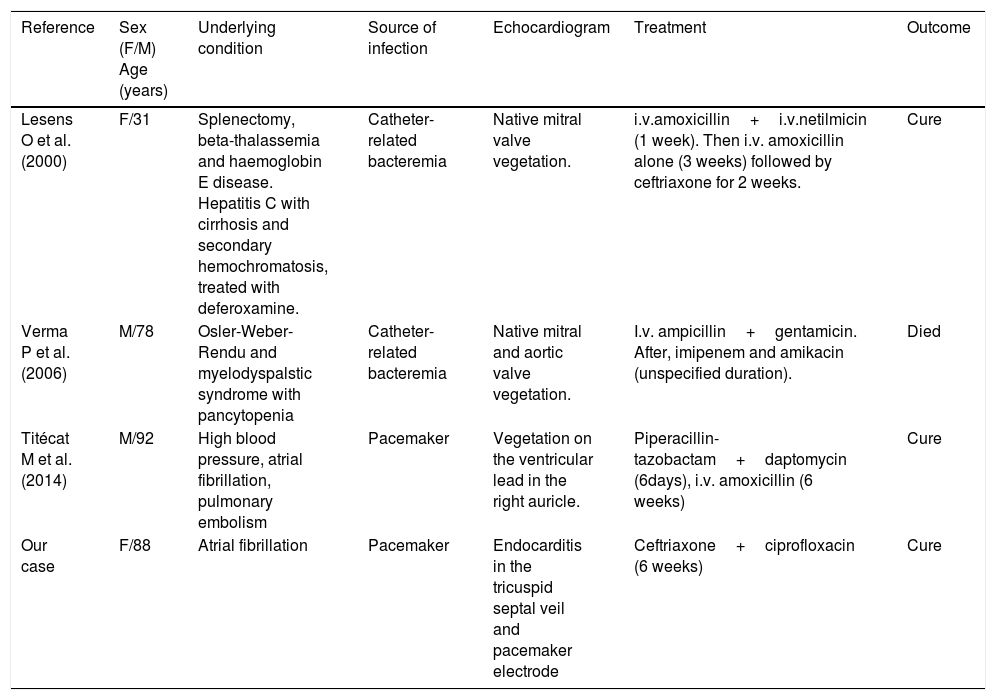
Gordonia bronchialis is involved in bacteraemia and sequestrated lung6, recurrent breast abscess7, pleural infection8, osteomyelitis9, sternal infection10–14, pacemaker-induced endocarditis 15,cutaneous abscess16, peritoneal dialysis associated peritonitis17 and endophthalmitis 18. To our knowledge, we describe the second case in the world of endocarditis caused by Gordonia bronchialis and the fourth case of endocarditis caused by Gordonia spp since two other cases produced by Gordoniapolyisoprenivorans19 and Gordonia sp. most closely resembling Gordonia sputi20 have been described. In these last two cases, endocarditis was caused by bacteremia associated with long-standing central catheter, in our case as well as in the case of Titécat M et al., endocarditis was caused by infection of the pacemaker system. The main characteristics of these 4 cases are described in Table 1.
Reported infective endocarditis due to Gordonia spp.
| Reference | Sex (F/M) Age (years) | Underlying condition | Source of infection | Echocardiogram | Treatment | Outcome |
|---|---|---|---|---|---|---|
| Lesens O et al. (2000) | F/31 | Splenectomy, beta-thalassemia and haemoglobin E disease. Hepatitis C with cirrhosis and secondary hemochromatosis, treated with deferoxamine. | Catheter-related bacteremia | Native mitral valve vegetation. | i.v.amoxicillin+i.v.netilmicin (1 week). Then i.v. amoxicillin alone (3 weeks) followed by ceftriaxone for 2 weeks. | Cure |
| Verma P et al. (2006) | M/78 | Osler-Weber-Rendu and myelodyspalstic syndrome with pancytopenia | Catheter-related bacteremia | Native mitral and aortic valve vegetation. | I.v. ampicillin+gentamicin. After, imipenem and amikacin (unspecified duration). | Died |
| Titécat M et al. (2014) | M/92 | High blood pressure, atrial fibrillation, pulmonary embolism | Pacemaker | Vegetation on the ventricular lead in the right auricle. | Piperacillin-tazobactam+daptomycin (6days), i.v. amoxicillin (6 weeks) | Cure |
| Our case | F/88 | Atrial fibrillation | Pacemaker | Endocarditis in the tricuspid septal veil and pacemaker electrode | Ceftriaxone+ciprofloxacin (6 weeks) | Cure |
With the advancement of molecular techniques, the number of recognized species of aerobic actinomycetes is increasing, and differentiation between related species is allowed. In our case, the identification by MALDI-TOF achieved a high score after extraction with ethanol-formic acid. However, correct identification is not always possible as it is not in the database of some automated systems and for its morphological similarity of the colonies with other species. In fact, in the other three published articles 15,19,20in which endocarditis occurred, the definitive identification required the 16S rRNA.
Regarding antibiotic treatment, there are currently no standardized guidelines, there are numerous combinations of antibiotics described in the literature. The combination of vancomycin and ceftazidime, trimethoprim-sulfamethoxazole and imipenem, piperacilia-tazobactam and daptomycin among others have been described. Later, according to evolution, the treatment has been sequenced to ciprofloxacin, linezolid and amoxicillin. A case has been described in which ceftaroline monotherapy has been used 21.
The case presented supports the pathogenic role of Gordonia bronchialis as an opportunistic pathogen and highlights the high risk of suffering infections caused by environmental bacteria and the importance of molecular analyses in the definitive identification of these and other related species.
Conflict of interestsThe authors declare that they have no conflict of interest.