In order to study the evolution of the outbreak that occurred between 2009 and 2010 in 3 hospitals in Zaragoza, all vancomycin-resistant clinical Enterococcus faecalis isolates identified between 2011 and 2013 at these hospitals were characterised.
MethodsMolecular characterisation of the isolates and analysis of their clonal relationships was performed using pulsed field electrophoresis, along with a retrospective review of the patient records.
ResultsA total of 79 vancomycin-resistant E. faecalis isolates with genotype vanB2 of 73 patients were recovered in 2 of the 3 hospitals, most of them from urine specimens. About 46% of the cases were nosocomial. Distribution of the isolates among hospital services demonstrated high variability, making it difficult to predict a common source of infection. All the strains were multiresistant (vancomycin, erythromycin, tetracycline, ciprofloxacin, streptomycin, gentamicin, kanamycin) and belonged to lineage ST6. Seventy-four isolates (93.7%) were identical or closely related to the dominant one in the origin of the outbreak.
ConclusionThe outbreak remains constant over three years after being initially described, indicating the need to implement an active control in order to limit the emergence and spread of vancomycin-resistant clones.
Con el objetivo de estudiar la evolución del brote por Enterococcus faecalis ST6 genotipo vanB2 descrito en 2009–2010 en 3 hospitales de Zaragoza, se caracterizaron todos los aislados clínicos E. faecalis resistentes a vancomicina obtenidos entre 2011 y 2013 en dichos hospitales.
MétodosCaracterización molecular de los aislados y estudio de su relación clonal por electroforesis en campos pulsados. Revisión de las historias clínicas de los pacientes.
ResultadosSe detectaron 79 aislados E. faecalis genotipo vanB2 de 73 pacientes de 2 de los 3 hospitales analizados, la mayoría de origen urinario. El 46,5% de los casos fueron nosocomiales. La distribución según servicios hospitalarios mostró gran variabilidad, no pudiéndose identificar una fuente de infección común. Todas las cepas fueron multirresistentes (vancomicina, eritromicina, tetraciclina, ciprofloxacino, estreptomicina, gentamicina, kanamicina) y pertenecieron al clon ST6. El 93,7% eran indistinguibles al clon del inicio del brote o subtipos estrechamente relacionados.
ConclusiónEl brote se mantiene constante en los 3 años posteriores a su descripción, lo que señala la necesidad de mantener un control activo que limite la emergencia y diseminación de clones resistentes a vancomicina.
Enterococcus faecalis and Enterococcus faecium are the third and fourth most common aetiology of nosocomial infections.1 The first strains of vancomycin-resistant Enterococcus (VRE) were reported in Europe in the eighties and, since then, hospital outbreaks mainly associated with E. faecium have been on the rise. Isolation of vancomycin-resistant E. faecalis (VREF) remains infrequent. Acquired glycopeptide resistance is mediated by various mechanisms, of which vanA and vanB are the most common. The acquisition of these resistances complicates treatment of VRE infections since the therapeutic alternatives are approved for specific clinical indications and resistances to them have also been reported.2
Spain is one of the European countries with the lowest rates of VRE, although sporadic nosocomial outbreaks have been reported,3–5 the majority associated with E. faecium ST17. The only outbreak due to E. faecalis vanB2 published to date in Spain was detected between 2009 and 2010 in 3 hospitals in Zaragoza.6 Later, between 2011 and 2013, 79 isolates with similar characteristics were identified in 2 of these hospitals. Our objective was to characterise these isolates to determine whether they belonged to the same outbreak and analyse the characteristics and evolution thereof.
MethodsDescription of the outbreak and bacterial isolatesAfter the start of the outbreak due to VREF with genotype vanB2 in November 2009 and its exhaustive study until 2010,6 subsequent follow-up was carried out by selecting and characterising all the vancomycin-resistant VREF isolates, collected in Hospital Universitario Miguel Servet (HUMS), Hospital Clínico Universitario Lozano Blesa (HCULB) and Hospital Royo Villanova (HRV) between January 2011 and December 2013. The isolates came from clinical samples received in the Microbiology Laboratory to diagnose the infection.
The patients’ medical records were reviewed, analysing microbiological, demographic and clinical variables: age, sex, origin of the infection, underlying pathology, prior antibiotic treatment, process treatment and patient evolution. In the case of strains from the same patient, only those coming from samples of different origins or different pulsed-field gel electrophoresis (PFGE) patterns were included.
Identification and antibiogramThe resistance phenotype was determined via disc diffusion and broth microdilution methods (MicroScan, Siemens). The susceptibility to ampicillin, clindamycin, erythromycin, chloramphenicol, ciprofloxacin, teicoplanin, vancomycin, tetracycline, quinupristin-dalfopristin, trimethoprim-sulfamethoxazole, gentamicin, streptomycin, kanamycin, linezolid and daptomycin was studied following EUCAST criteria.7 The production of beta-lactamase was not evaluated. The minimum inhibitory concentration of vancomycin, teicoplanin and daptomycin was determined via the Etest method (Biomérieux). The vancomycin resistance genes (vanA, vanB, vanC-1, vanC-2/3 and vanD) were analysed via PCR in all isolates and the vanB2 gene was sequenced in a strain selected for each PFGE profile.6,8
Molecular typificationThe clonal relationship of VREF vanB2 was analysed via chromosomal DNA digestion (SmaI) and subsequent separation of the fragments using PFGE. The genetic profiles were compared following the Tenover criteria.9
One isolate was selected for each PFGE pattern, and these were studied via multilocus sequence typing (MLST), amplifying and sequencing the fragments of genes gdh, gyd, pstS, gki, aroE, xpt e and qiL (http://efaecalis.mlst.net).
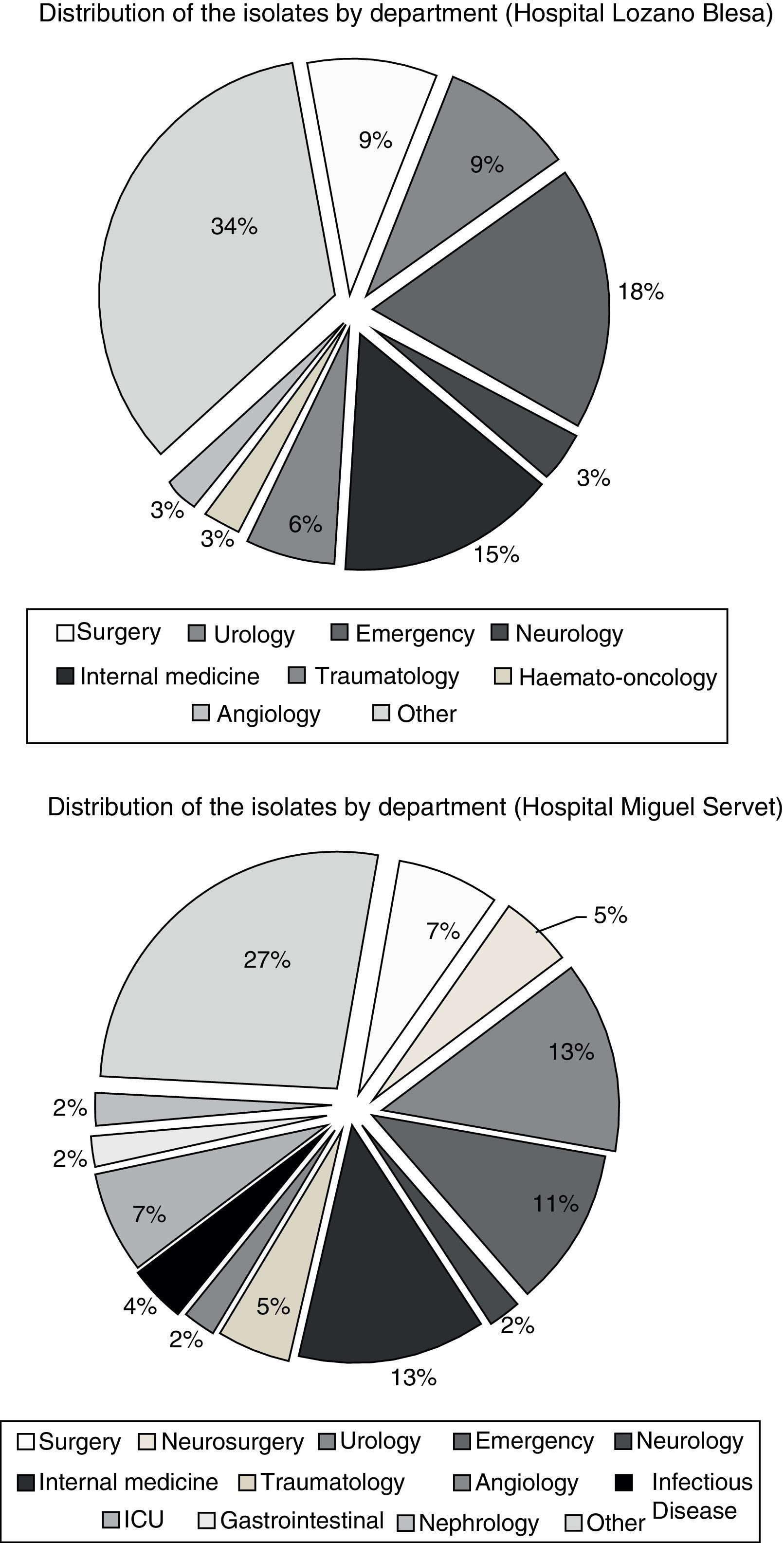
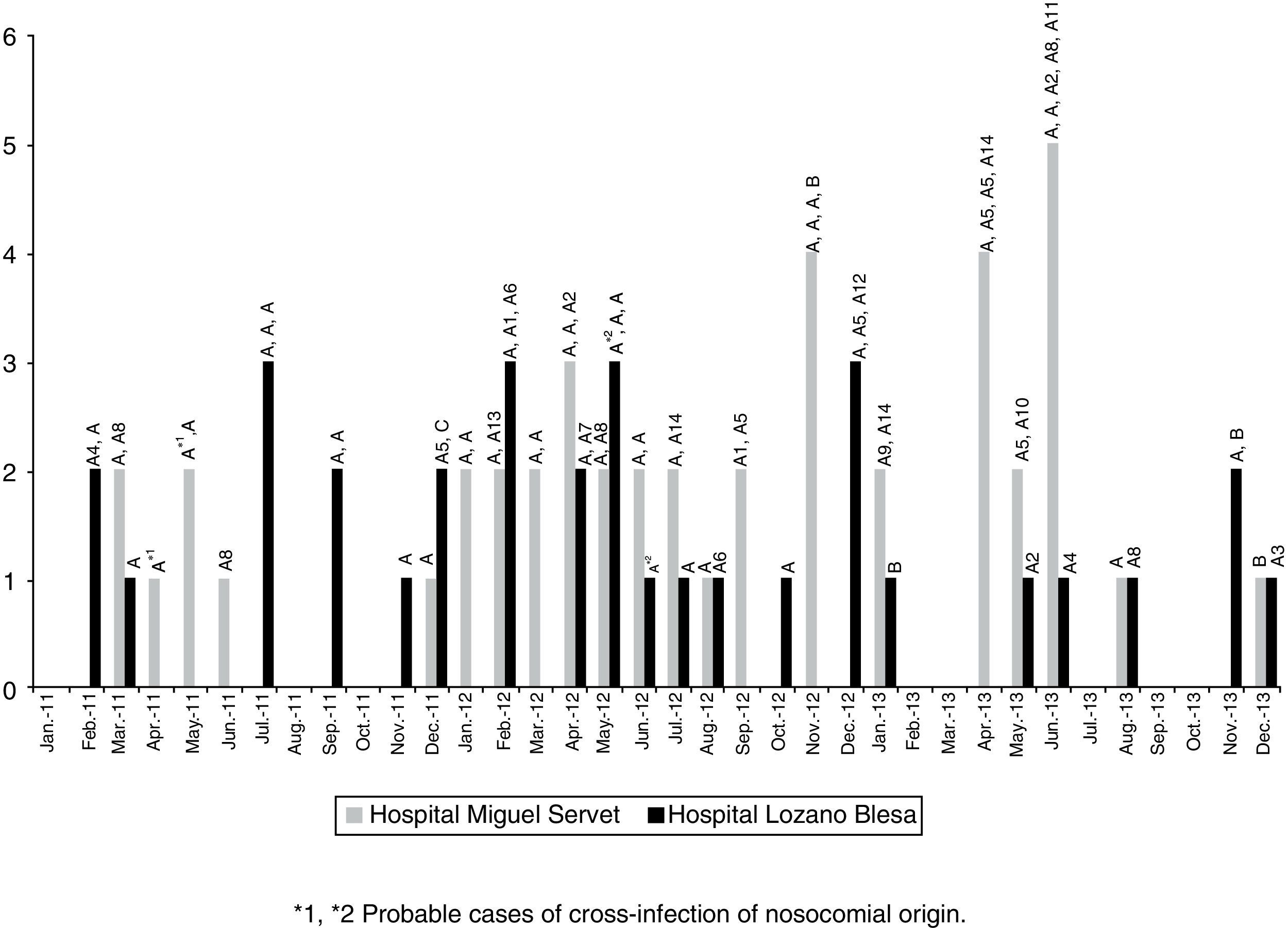
ResultsIn the study period (2011–2013), 79 vancomycin-resistant E. faecalis isolates were detected with genotype vanB2 (46 in HUMS, 33 in HCULB), from 73 patients (45.5% men; average age: 73 years). No VREF was detected in the study period in HRV. The majority of isolates (62; 78.5%) were obtained in urine samples. None of the patients with available data on prior antibiotic therapy had received vancomycin, but they had received beta-lactams (14/32) and/or fluoroquinolones (20/32). In 54 patients, E. faecalis vanB2 was confirmed as the causative agent of the infectious symptoms. Of the 71 cases in which it was possible to study the origin of the infection, 32 (45.1%) were community-acquired, 33 (46.5%) were nosocomial and 6 (8.4%) were associated with health care. The distribution of the isolates by hospital department showed it was widespread (Fig. 1), which suggests the existence of different sources of infection or transmission of these clones via healthcare staff or patient transfer. Cross-infection of nosocomial origin seems especially likely in 2 cases: one in the HUMS neurosurgery department in April–May 2011 and another in the HCULB traumatology department in May–June 2012. In both cases, VREF vanB2 was isolated with equal pulsotypes from different patients who coincided in the same department and period of time during their hospital stay.
Regarding the genotype study, all strains carried the vanB2 gene, and in all of them a specific mutation (G34T) was detected that involved an amino acid change (Met11Ile) in said allele. The isolates presented a multidrug-resistant phenotype that included, in addition to vancomycin resistance, resistance to erythromycin, tetracycline, ciprofloxacin and high levels of resistance to streptomycin, gentamicin and kanamycin.
The PFGE revealed the existence of 3 genetic profiles (pattern A and its subtypes, pattern B and pattern C). The majority of the strains (n=74; 93.7%) belonged to a clone identical to the one from the start of the outbreak (A, n=43) or a closely-related subtype (A1–A14, n=31, 1–3 band differences). Four strains, isolated in both hospitals and belonging to different patients, were identified as clone B and one as clone C (>6 band differences). MLST typing conducted on 16 isolates representing the different types and subtypes of PFGE showed that all of them belonged to the sequence type ST6. Fig. 2 shows that the frequency in detection of VREF vanB2-ST6 isolates remained stable during the 3 years of outbreak follow-up.
DiscussionUnlike in the United States, where outbreaks of VRE (mainly E. faecium) have been reported with relative frequency, in Europe the prevalence has been lower, although in recent years, an increase has been shown in some countries.1 For years, detection of E. faecium genotype vanA has been common in farm animals and food, probably in relation to the widespread use of avoparcin as a growth promoter in animals until 1997, the year that this use was prohibited in the European Union. Although E. faecalis is mainly responsible for enterococcal infections, E. faecium presents higher rates of acquired antimicrobial resistance. VREF infections continue to be infrequent. Thus, due to the special characteristics of the first outbreak of E. faecalis vanB2 reported in Spain, in this project we conducted follow-up and characterisation of the clinical isolates of the following years. It should be noted that the clonal relationship of the isolates was established via PFGE, indicated preferentially for strains isolated in hospitals during periods shorter than 6 months.10 Nevertheless, the lack of alternative methodologies in terms of cost, reproducibility and discriminatory power has fostered the extension of its use in studies evaluating outbreaks. Furthermore, acquisition of horizontal transfer elements could give rise to changes in more than 6 bands, which could lead to sub-estimation of the total number of related clones.
Regarding the origin of the strains, the majority came from urine samples, as is also described in earlier studies.11 None of the patients from whom information could be collected about prior antibiotic treatment had received vancomycin. Therefore, unlike other studies,3 no association was observed between prior consumption of vancomycin and emergence of VREF vanB2. However, the selection of these clones as a result of the prior antibiotic administration of other families commonly related to VRE acquisition3,12 (such as fluoroquinolones, against which the studied clones showed resistance, or cephalosporins), cannot be ruled out.
Sequence type ST6, to which E. faecalis isolates belong, is, along with ST17 (in E. faecium), one of the genetic lines which is best adapted to the hospital environment in Spain.13 In 2004, the spread of an E. faecalis clone belonging to this line, but carrying the gene vanA, in 3 Portuguese hospitals was reported.14 These facts support the studies suggesting that ST6 is particularly suitable for picking up exogenous genes (such as vanA or vanB) via recombination.15E. faecalis strains belonging to this line have also been detected in pigs16 and in a wild rat,17 showing characteristics very similar to the clinical strains from Portugal and Spain. It should be highlighted that the mutation detected in allele vanB2 (G34T), which entails an amino acid change (Met11Ile), was also observed in the isolate from the rat. Future studies that determine the possible biological implication of this mutation present in the allele vanB2 of enterococcal strains spread in such varied environments will be needed.
Molecular typification allowed us to observe the circulation of 3 clones present in both hospitals and with a distribution over time without a definite trend. Unlike what is observed in outbreaks caused by E. faecium, usually polyclonal and in which the predominant clone at the beginning gives way to other variants,6,7,11 in this outbreak, both the predominant clone (A) and other clones (B, C) and even its subtypes (A1–A14) were detected throughout the 3 years, without one variant being clearly associated with a particular hospital. This, along with the high rate of community cases and the high variability in distribution of the isolates by hospital department, suggesting the possibility that it is a clone that is widely distributed in this area. It is therefore necessary to implement control strategies to reduce the persistence of these VREFs, avoid spread and emergence of new clones, and the possible horizontal transfer of vanB genes to other strains to preserve the clinical usefulness of vancomycin.
FundingThis project has been partly funded by the SAF2012-35474 project of the Ministerio de Economía y Competitividad (MINECO) [Ministry of Economy, Industry and Competitiveness] and the European Regional Development Fund (ERDF). C.A. Alonso has a FPI (research personnel training) pre-doctoral grant from MINECO attached to the SAF2012-35474 project.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Alonso CA, Rezusta A, Seral C, Ferrer I, Castillo FJ, Torres C. Persistencia de un clon ST6 de Enterococcus faecalis con genotipo vanB2 en dos hospitales de Aragón. Enferm Infecc Microbiol Clin. 2017;35:578–581.