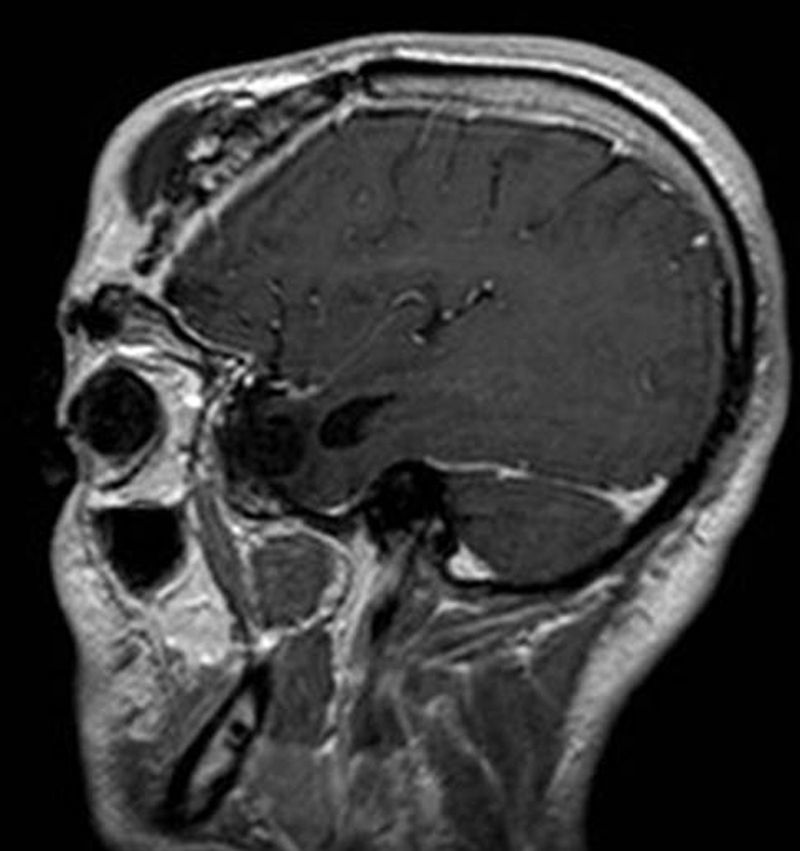
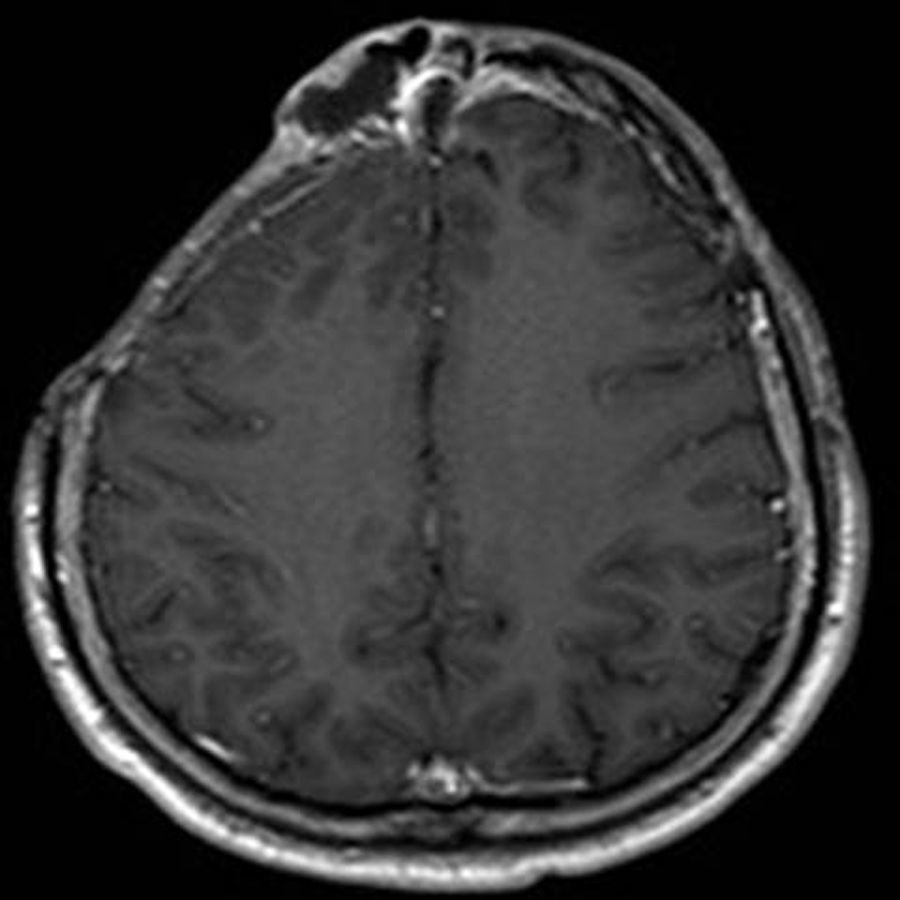
32-Year-old male, intranasal drug user, who was involved in a road traffic accident when he was 18 years of age, with comminuted right frontal and supraorbital bone fractures and subsequent recurrent CSF leak (fistula), associated with recurrent meningitis caused by H. influenzae and S. pneumoniae, which required up to 3 prior surgeries. He was admitted in April 2011 due to pneumococcal (S. pneumoniae) meningitis associated with fluctuating swelling of the forehead and right frontal epidural abscess (Figs. 1 and 2).
A right frontal craniotomy and sinus drainage was performed, obtaining cultures positive for S pneumoniae; after 6 weeks of treatment with intravenous ceftriaxone and an asymptomatic period with no recurrences, a right frontal cranioplasty (CustomBone®) was implanted in September 2012.
After one year symptom-free, the patient was readmitted in November 2013 with recurrent pneumococcal meningitis and with an underlying previous epidural abscess to the cranioplasty that had to be removed, debridement of the right frontal sinus and intravenous treatment with ceftriaxone followed by oral levofloxacin. Due to intolerance, the patient switched to clindamycin, which he received until he completed 6 months of treatment (June 2014).
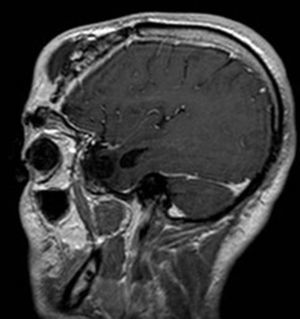
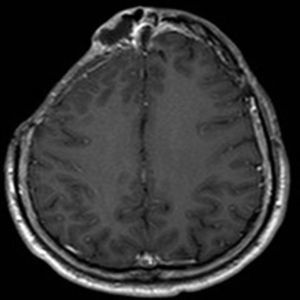
Clinical courseThe patient was readmitted in October 2014 due to recurrence of fluctuating swelling with spontaneous supranasal suppuration and cultures positive for coagulase-negative Staphylococci. After administering vancomycin+ceftriaxone, and despite the brain MRI not showing obvious intracranial collections (Fig. 3), another frontal craniotomy, drainage and debridement of the left frontal sinus, supranasal sinus and residual right supraorbital sinus sealed with wax were performed, and vancomycin and gentamycin were administered. The intraoperative cultures were negative and the universal 16S PCR undetectable, so intravenous treatment was completed for 6 weeks with IV teicoplanin 600mg/24h and ceftriaxone 2g/12h.
Final commentSuppurative osteomyelitis of the frontal bone, also known as Pott's Puffy Tumour, is a rare and little-known condition that is seldom reported in the medical literature. It is characterised by fluctuating swelling of the forehead secondary to a subperiosteal abscess caused by frontal bone osteomyelitis. It is most commonly seen in children and adolescents in whom the most widespread predisposing factor is acute or chronic frontal sinusitis.1 It is much less common in adults, however, and the main risk factors include frontal bone trauma, prior craniotomy or cranioplasty, mastoiditis, nasal drug abuse, tooth infection and ethmoid sinusitis.2,3
The pathogenesis of this condition is closely related to the unique anatomy of the sinuses and the ease of propagation through the mucosal venous drainage of the frontal sinus towards the diploë. The solutions of continuity in the sinus wall secondary to the risk factors described above facilitate progression of the infection. The clinical picture varies depending on the spread of the infection, and it may manifest as swelling of the frontal region without intracranial spread if it progresses towards the external table of the frontal bone, as an epidural abscess if it progresses towards the internal table or as orbital cellulitis if it spreads towards the supraorbital region.4,5
It is diagnosed on the basis of clinical and radiological findings. Typical symptoms in adults include fever, purulent rhinorrhoea, frontal or orbital cellulitis, fluctuating swelling or frontal fistula, as well as neurological symptoms such as meningitis or frontal focal symptoms.3
The CT scan is the gold standard for frontal bone osteomyelitis diagnosis, while MRI is effective at identifying intracranial complications. Labelled leucocyte scintigraphy may be useful in monitoring treatment response.6
The bacteria involved in the pathogenesis of the condition are mostly found in the saprophytic flora of the sinuses and lead to infection by anaerobic S. aureus and Streptococcus sp., Gram-negative bacteria and fungi.2
Treatment involves a combined medical-surgical approach: early broad-spectrum antibiotic treatment and the surgical drainage of intracranial collections (external or endoscopic) depending on the location and extent of the complications.7
Prognosis is variable and is determined by potential neurological sequelae and the high probability of recurrence, associated with significant morbidity owing to the need for multiple surgical procedures as shown in the case presented above.3,8
FundingThe authors declare that they have not received funding of any kind to complete this study.
Conflicts of interestThe authors declare that they have no conflicts of interest.
We would like to thank the clinicians involved in the case listed as co-authors, as well as all the other clinicians who helped to treat this patient during his multiple readmissions.
Please cite this article as: Corcóstegui Cortina T, Guío Carrión L, Aurrekoetxea Obieta J, Montejo Baranda JM. Tumoración frontal recidivante en paciente con craneotomías de repetición. Enferm Infecc Microbiol Clin. 2017;35:262–263.