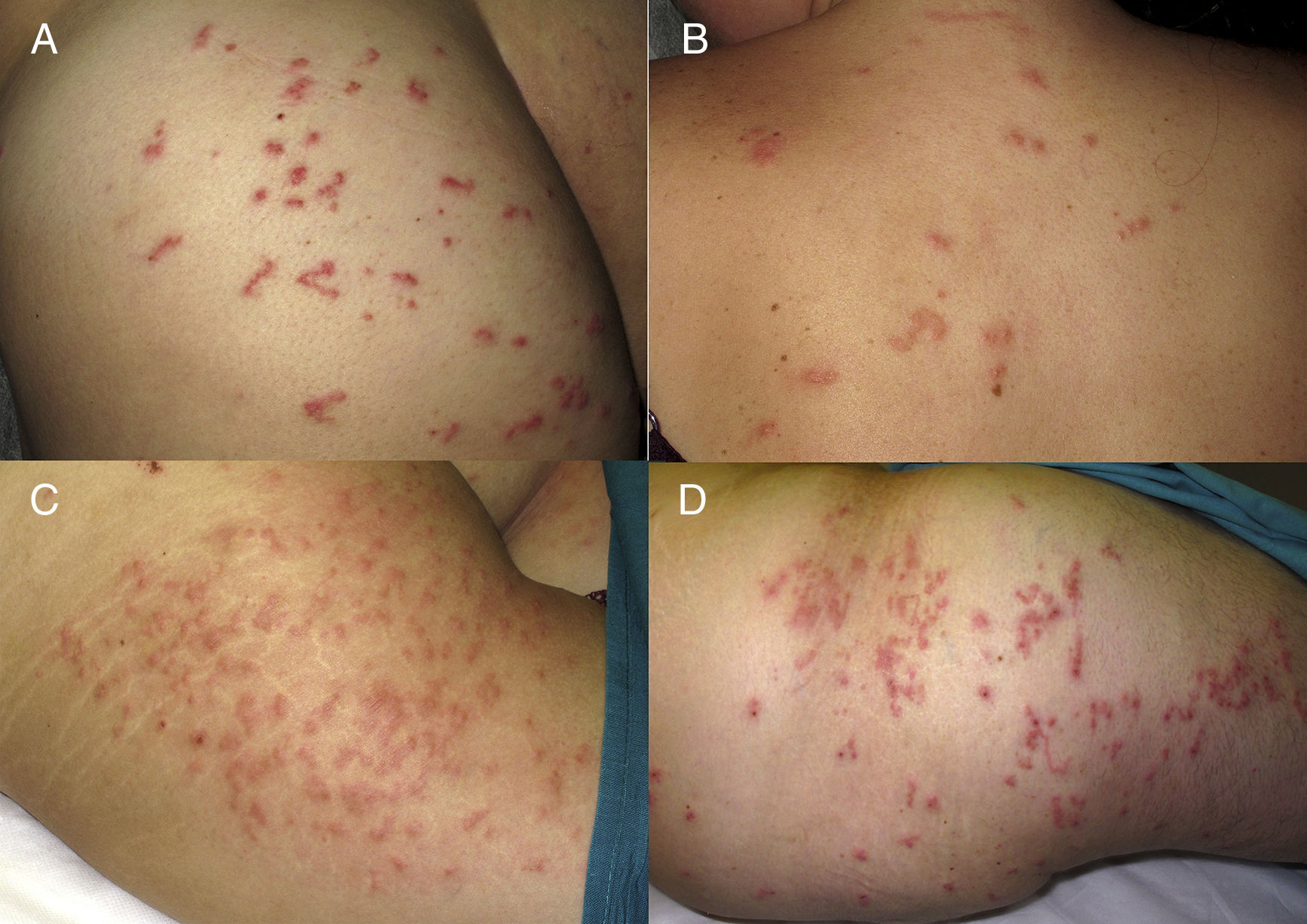
Cutaneous larva migrans (CLM) is one of the principal dermatological diagnoses in travellers returning from the tropics. It is easily recognisable by its characteristic serpiginous path. Most cases are identified and treated in primary care or traveller's consultations, without requiring a specific dermatological assessment to establish their diagnosis. However, there are cases with an atypical clinical presentation1 in which a papular component centred on the follicles predominates, known as CLM folliculitis or follicular cutaneous larva migrans (FCLM). The following are 3 cases of CLM with extensive affectation and folliculitis in travellers from Thailand. Three tourists had been in direct contact with wet sand on the coast of Phuket for several days on a trip made in the month of August (rainy season). Afterwards, they developed pruritus and some early stage pruritic papules (Fig. 1). Their clinical characteristics are summarised in Table 1. The response to oral ivermectin was satisfactory in all 3 cases, with rapid disappearance of the pruritus (first 48–72h) and progressive improvement of the lesions until their complete resolution in 2 weeks.
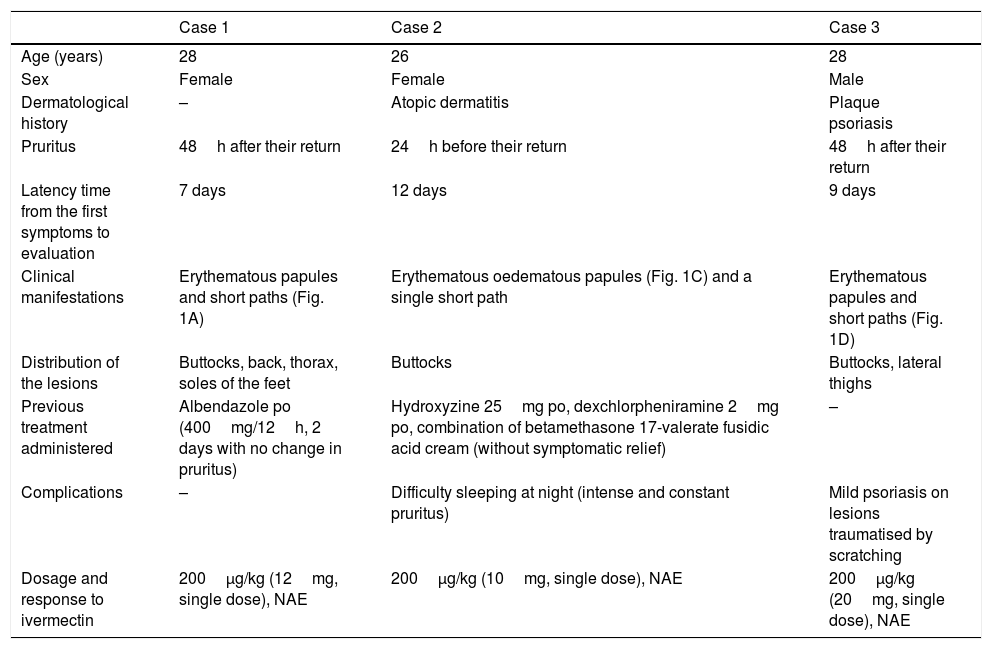
Clinical characteristics of the 3 patients diagnosed with FCLM.
| Case 1 | Case 2 | Case 3 | |
|---|---|---|---|
| Age (years) | 28 | 26 | 28 |
| Sex | Female | Female | Male |
| Dermatological history | – | Atopic dermatitis | Plaque psoriasis |
| Pruritus | 48h after their return | 24h before their return | 48h after their return |
| Latency time from the first symptoms to evaluation | 7 days | 12 days | 9 days |
| Clinical manifestations | Erythematous papules and short paths (Fig. 1A) | Erythematous oedematous papules (Fig. 1C) and a single short path | Erythematous papules and short paths (Fig. 1D) |
| Distribution of the lesions | Buttocks, back, thorax, soles of the feet | Buttocks | Buttocks, lateral thighs |
| Previous treatment administered | Albendazole po (400mg/12h, 2 days with no change in pruritus) | Hydroxyzine 25mg po, dexchlorpheniramine 2mg po, combination of betamethasone 17-valerate fusidic acid cream (without symptomatic relief) | – |
| Complications | – | Difficulty sleeping at night (intense and constant pruritus) | Mild psoriasis on lesions traumatised by scratching |
| Dosage and response to ivermectin | 200μg/kg (12mg, single dose), NAE | 200μg/kg (10mg, single dose), NAE | 200μg/kg (20mg, single dose), NAE |
FCLM: follicular cutaneous larva migrans; NAE: no adverse effects.
FCLM is a clinical picture that is scarcely described in the literature, characterised by the absence or scarcity of typical serpiginous paths in its initial phases. Its pathogenesis entails penetration of larvae through the follicular orifices, without the need for a continuous epidermal route. Subsequently, the larvae move through the follicular epithelium, a movement that generates a local hypersensitivity reaction to the parasite, expressed in the form of papules and/or pruritic pustules. The typical serpiginous paths appear later, in the most evolved phases of the clinical picture. They tend to be shorter than in conventional cases and originate from a papule centred around the follicle. The presence of a greater number of paths in cases of parasitic folliculitis seems to be related to the massive penetration of multiple larvae through the follicles from highly parasitised soils. The diagnosis is clinical and skin biopsy usually does not provide additional relevant information, given the difficulty in detecting the parasites. Notable complications include eczematisation or bacterial superinfection, especially when the diagnosis is delayed.2–4 Atypically, tissue invasion from Ancylostoma larvae with the ability to produce hyaluronidase, a virulence factor that allows them to reach the dermal vessels and from there the lung and the digestive tract (Löffler's syndrome), has been described.5 Treatment is based on the administration of albendazole (400mg/day for 3 days) or oral ivermectin (200μg/kg of body weight in a single dose).6,7 For some authors, cases of FCLM pose a greater resistance to antiparasitic treatment than the classic forms of CLM. In a study conducted by Caumes et al. in 2002, follicular forms of CLM imply a greater probability of therapeutic failure than classic forms with the usual doses of oral ivermectin.8 However, in the published cases a uniform dose of ivermectin (12mg) is administered, without specifying a calculation of the dose based on the weight of each patient. Subsequently, this group retrospectively evaluated the response to ivermectin with an adjusted dose of 200μg/kg in cases treated from 2008 to 2012, concluding that the efficacy of ivermectin in a single dose is higher in classic CLM than in FCLM.9 In any case, what does seem clear is the lack of response to topical treatment with thiabendazole, as a consequence of the location of the larvae in the epithelium or follicular canal and the presence of a higher parasitic load in FCLM forms.
In conclusion, despite the fact that the main cause of follicular lesions in patients returning from the tropics is bacterial folliculitis, CLM should be considered in the differential diagnosis of those patients who present with papular, pruritic lesions and/or who do not respond to conventional antibacterial treatment. Likewise, a complete physical examination should be carried out in search of the characteristic serpiginous paths, visible in the most evolved phases of the clinical picture, that define this parasitosis. Antiparasitic treatment with ivermectin adjusted to weight (200μg/kg in a single dose) in adult patients would be effective in most patients with FCLM. However, given the controversy over the greater resistance of follicular forms to single dose treatment, we recommend a close follow-up of these patients in the first week after treatment.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Pulido-Pérez A, Nieto-Benito LM, Sánchez-Herrero A, Suárez-Fernández R. Respuesta a ivermectina oral en 3 casos de larva migrans folicular. Enferm Infecc Microbiol Clin. 2019;37:415–416.