This was a 42-year-old patient with no relevant medical history who came to the hospital with a skin lesion on the left leg and feeling shivery. He reported the appearance, two months earlier, of a non-pruritic, scaly erythematous plaque on his left knee. On examination, an infected rounded plaque with desquamating borders was found on the lateral aspect of the left knee with several abscessed points, as well as signs of cellulitis and lymphangitis in the thigh (Fig. 1). Several hard, mobile and painful enlarged lymph nodes were found in the left inguinal region. The patient lived in the country in contact with cows, goats and horses, and reported falling off a horse onto brambles. After prescribing IV treatment with amoxicillin-clavulanic acid, the patient was admitted to the infectious diseases unit with a differential diagnosis of mycobacterial infection vs nocardiosis. A biopsy of the lesion was taken for histological and microbiological study. A small desquamative erythematous lesion was also found in the right pretibial area, but without signs of infection. The patient was discharged 48h after admission with amoxicillin-clavulanic acid and cotrimoxazole.
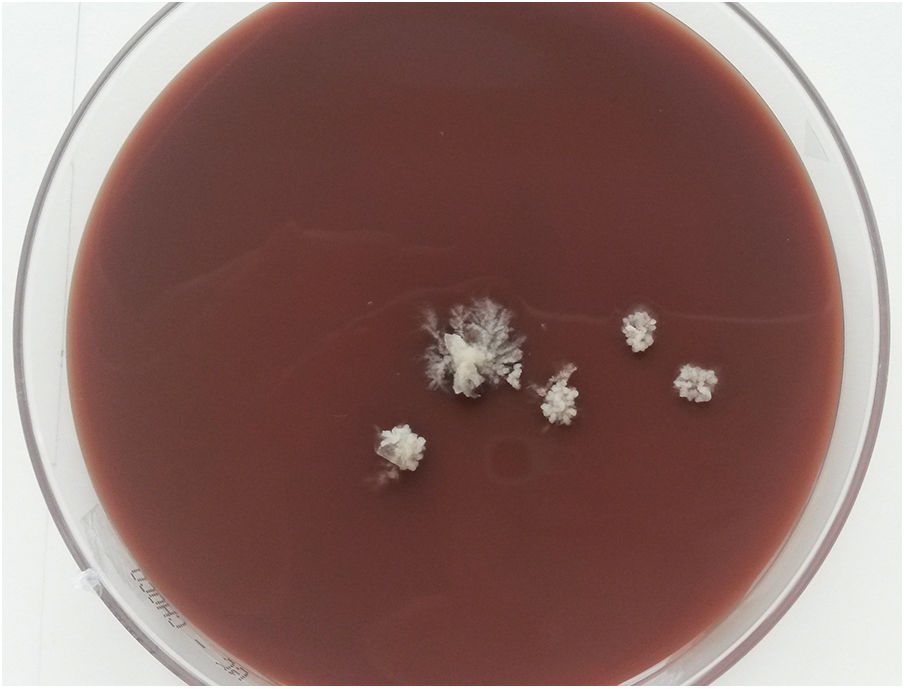
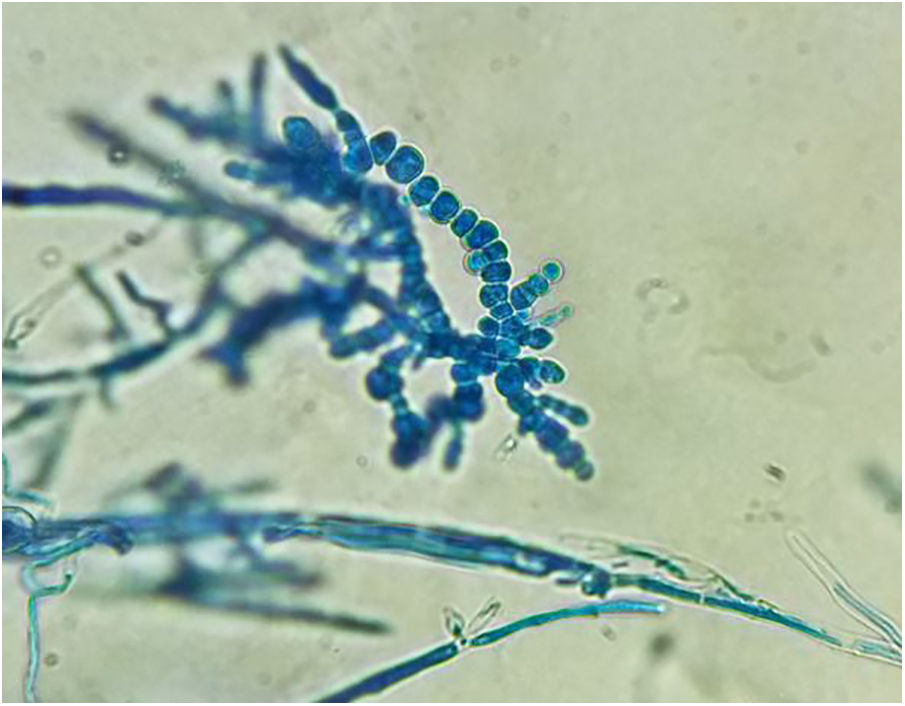
OutcomeAfter 7–10 days of incubation, the pure growth of a filamentous fungus forming creamy cerebriform colonies was observed in the cultures of exudate, abscess and biopsy from the patient's knee lesion in chocolate agar medium and blood agar at 37°C (Fig. 2). The antibiotic treatment was therefore discontinued and treatment with oral terbinafine was prescribed. Days later, growth was observed in Sabouraud medium with chloramphenicol and gentamicin at 30°C. Microscopic examination showed hyphae with chandelier appearance, absence of macroconidia and microconidia, and the presence of long chains of compacted chlamydoconidia suggestive of Trichophyton verrucosum (Fig. 3). The histological study showed an inflammatory process in the dermis with follicular destruction and presence of PAS-positive rounded structures, compatible with Majocchi granuloma. After six weeks of treatment, the lesion on the right tibia progressed to cellulitis with small pustular lesions and signs of lymphangitis. In the culture of one of the lesions, T. verrucosum was isolated again, with identification confirmed by the sequencing of the ITS region of the rRNA. Finally, after 12 weeks of treatment with terbinafine 250mg/d, the lesions had completely disappeared and the patient was discharged with no abnormal laboratory test results.
Trichophyton verrucosum is a zoophilic dermatophyte fungus of cosmopolitan distribution which causes inflammatory tinea infections through direct or indirect exposure with cattle and less commonly with other animals. The prevalence of the infection in humans varies greatly depending on the geographic area studied1,2 and has been related to different milking practices, humidity, hygiene conditions and animal vaccination programmes in the area. The most common forms of clinical presentation are tinea corporis, tinea capitis and tinea barbae (kerion).3,4 Majocchi granuloma is a form of dermatophytosis in which the fungus invades the dermis and destroys the hair follicle. It is very uncommon and is usually seen in patients with either trauma or immunosuppression factors, and in these cases it can spread via the lymphatic or vascular systems or by contact.5–8 The differential diagnosis of this clinical condition includes infection by Nocardia spp., atypical mycobacteria or other mycoses, especially in patients with lesions in the extremities and who spend time in rural areas. The definitive diagnosis is determined by the requirements of the fungus, as the optimum temperature for growth is 37°C, and it needs media enriched with thiamine or inositol. This means growth is slow and it is not uncommon to detect it in bacteriological media, such as blood, chocolate or BHI agar.9 The antifungals most often used for the treatment of these severe forms of dermatophytosis are terbinafine and triazoles, and the duration of treatment is determined by the clinical response and host factors.6,10
In conclusion, we present a rare case of invasive dermatophytosis caused by T. verrucosum in an immunocompetent patient, probably acquired through direct contact with a sick animal or spores in the soil or fomites. The inflammatory reaction in mycosis caused by T. verrucosum and the difficulty the fungus has in recovering in mycological culture media can lead to the delayed diagnosis of this infection.
Please cite this article as: López-Soria L, Aguirrebengoa Ibarguren K, Ratón Nieto JA, Barrios Andrés JL. Lesión cutánea y linfangitis en paciente inmunocompetente. Enferm Infecc Microbiol Clin. 2019;37:481–482.