A 49-year-old woman admitted to the infectious disease department with a fever of one week's onset and general state of deterioration. Her history included a 22-year history of HIV infection with poor adherence to treatment, resulting in poor control of her disease. On admission she had a viral load of 135,000 copies of RNA/ml and a CD4 count of 30cells/mel. She presented complications of repeated oropharyngeal and oesophageal candidiasis. She also had generalised psoriatic plaques of 8 years’ onset, with poor adherence to treatment (acitretin and topical corticosteroids), and exacerbated by the advanced stage of HIV infection.
Physical examination revealed generalised large erythematous desquamative plaques affecting the chest and limbs bilaterally and symmetrically (PASI score 25, BSA 50%, PGA 5).
Diagnosis and outcomeThe patient was admitted to investigate her fever with no apparent focal point of infection and antiretroviral treatment was restarted with topical corticosteroids for the psoriasis. The initial test results showed neutropenia and chest X-ray was normal.
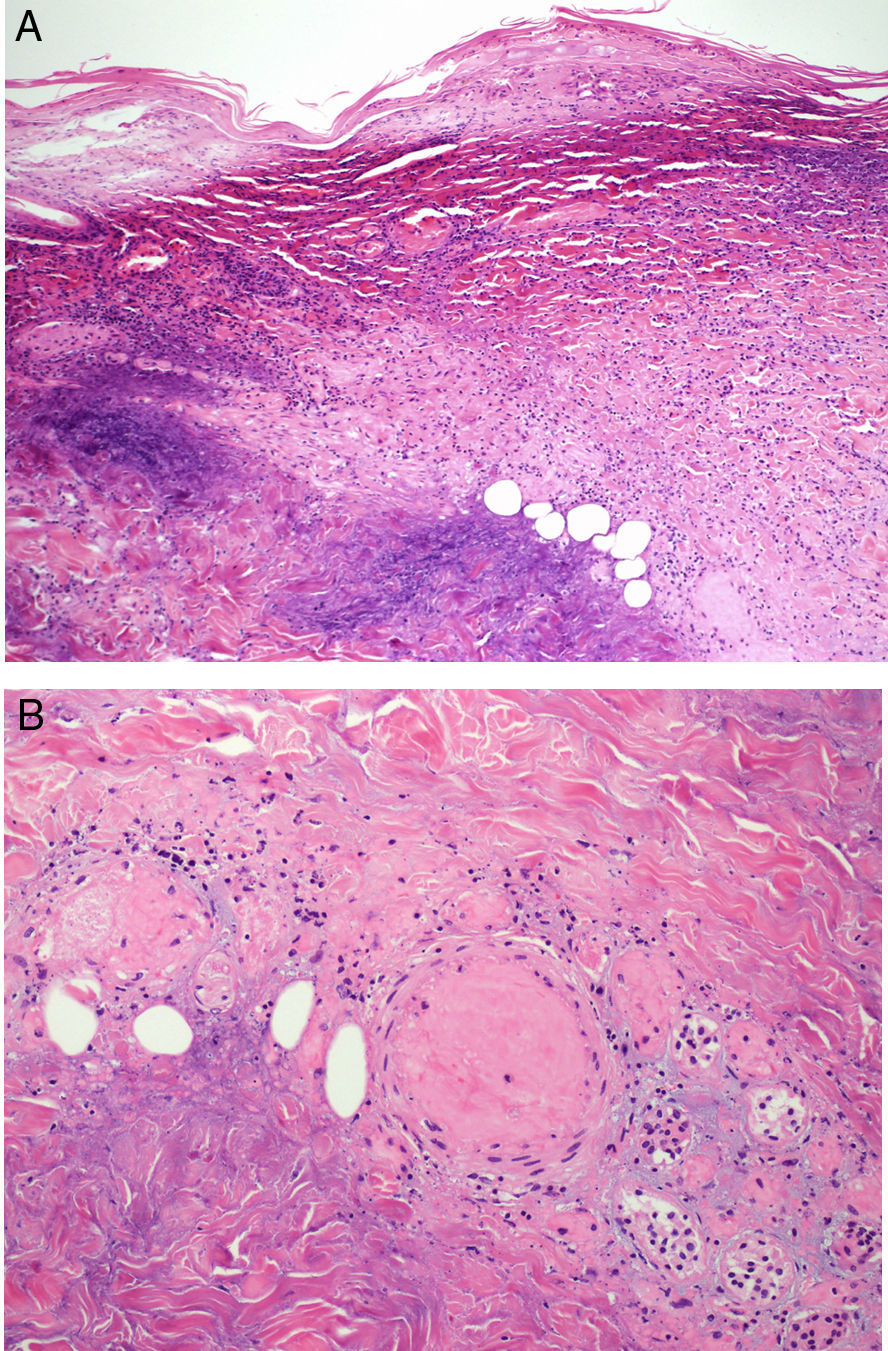
The patient's general state of health deteriorated 72h after admission with the onset of confluent, violaceous macules/papules on the psoriasis plaques gradually progressing to necrotic ulcers (Fig. 1). The patient made poor progress, with reduced level of consciousness, hypotension, oliguria and signs of poor peripheral perfusion, in addition to the progression of the skin lesions (Fig. 2). Despite starting intravenous cloxacillin and meropenem, intensive saline therapy and vasoactive drug perfusion, the patient died. Skin biopsy revealed superficial and deep necrosis with pronounced acute inflammatory infiltration of the dermis and subcutaneous tissue, with vascular thrombosis (Fig. 3). It was not possible to observe bacteria by Gram staining around the vessels. Staphylococcus aureus sensitive to cloxacillin and Pseudomonas aeruginosa were isolated in blood cultures and the biopsy culture with no relevant resistance. The PCR of the exudate from the lesions was negative for herpes simplex virus 1 and 2 and the varicella zoster virus.
(A) Skin biopsy of one of the necrotic ulcers showing necrosis of the superficial and deep dermis, with a large inflammatory dermal component. (B) On enlargement of the image, in addition to the necrosis and the polymorphonuclear inflammatory infiltration, we can observe dermal blood vessels with vascular thrombosis, associated with the inflammatory process.
Although the prevalence of psoriasis in HIV-infected patients is similar to that in the general population, in these patients the disease tends to be more severe and worsen as their immunosuppression progresses.1–3 Furthermore, in the generalised stages, it can form a portal of entry for microorganisms that can lead to sepsis.4
Sepsis is still one of the main causes of mortality in the world. The frequency of onset of skin lesions associated with sepsis is not well known, although it is essential to be able to identify them because they tend to express in early stages, which will enable prompt diagnosis and treatment. One of the pathophysiological mechanisms that would explain the onset of these skin lesions is direct invasion of the vascular wall by the microorganism responsible for the sepsis, as occurs in ecthyma gangrenosum.5 This disorder is essentially caused by P. aeruginosa, although cases caused by different microorganisms have been described including S. aureus. Necrosing vasculitis occurs with vascular thrombosis which triggers a cutaneous infarction that progresses to ulcerated lesions, which can be single or multiple and can appear on any part of the body. It is more common in immunosuppressed patients with intense and prolonged neutropenia.5–8
We present the case in this article of a patient infected by HIV in an advanced state of immunosuppression, neutropenia and with poorly controlled psoriasis. Her generalised psoriasis could have formed the portal of entry for S. aureus, the most common skin bacteria in HIV infection, and P. aeruginosa.9,10 The symptoms, histology, blood cultures and the biopsy culture led us to the conclusion that our patient's ulcerated lesions were probably an ecthyma gangrenosum due to a septic vascular disease caused by P. aeruginosa. However, we cannot discount the aetiological role played by S. aureus, less commonly involved in the pathogenesis of this disorder. This clinical case illustrates the need for strict therapeutic control of both the HIV infection and the psoriasis of patients in whom both diseases coexist, considering the serious systemic complications that can be triggered.
FundingThe authors declare that they have received no source of funding.
Conflict of interestThe authors have no conflicts of interest to declare.
Our thanks go to Berta Ferrer and Rosa Cristòfol for their collaboration.
Please cite this article as: González-Cruz C, Espinosa Pereiro J, Aparicio Español G, Falcó Ferrer V. Úlceras sobre placas psoriásicas en paciente con infección avanzada por el virus de la inmunodeficiencia humana. Enferm Infecc Microbiol Clin. 2017;35:605–606.