We present the case of a 72-year-old male with a history of cardiovascular surgery for myocardial revascularisation, with placement of a double coronary by-pass by grafting of the left internal mammary artery to the left anterior descending artery and of the saphenous vein to the right coronary artery. His previous medical history included resection of a malignant bladder tumour, type 2 diabetes mellitus treated with oral antidiabetic drugs and obesity.
One month after discharge from hospital, he came to the emergency department with fever and suppuration of the median sternotomy wound, with purulent discharge on pressure and a fluctuating abscess in the lower part of the wound. It was decided to admit the patient to hospital for treatment with vacuum-assisted closure (VAC). Samples of exudate were collected and vancomycin (15 mg/kg/12 h IV) and ceftazidime (2 g/8 h IV) were prescribed.
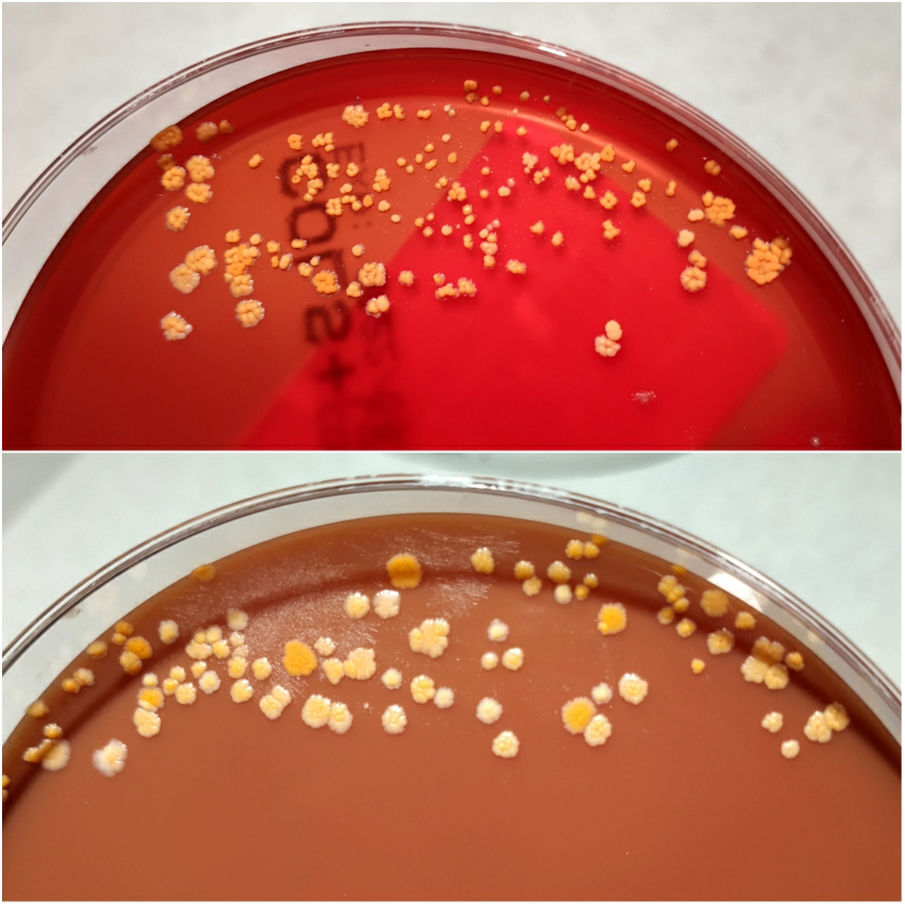
The surgical wound exudate samples were cultured on blood and chocolate agar (Thermofisher) incubated at 37°C in CO2 atmosphere. After incubation for 72 h dry, rough, polymorphous yellow colonies began to grow (Fig. 1).
Clinical course and diagnosisGram staining of these colonies revealed irregular Gram-positive bacilli. Identification was performed by MALDI-TOF mass spectrometry (Maldi-Biotyper, Bruker), which determined Gordonia bronchialis with score of 2090. With longer incubation, the colonies acquired a rougher and more raised appearance, as well as a more orange colour, typical of the carotenoid production of this micro-organism (Figs. 2 and 3).
Once the species was identified, it was decided to treat with linezolid (600 mg/12 h IV) and ceftriaxone (2 g/8 h IV). G. bronchialis grew in subsequent successive cultures of all the samples collected from both the wound and the sternal tissue biopsy.
Antibiotic sensitivity was determined by microdilution using the MICroSTREP plus 6 panel (MicroScan®, Beckman) incubated 72 h, and by E-test® (bioMérieux) on Mueller-Hinton plates with 5% defibrinated horse blood and 20 mg of ®-NAD/l (Thermofisher) incubated 48 h. For the interpretation of sensitivity, the Clinical and Laboratory Standards Institute (CLSI) criteria for mycobacteria, Nocardia spp. and other aerobic actinomycetes (2011) were followed, with the strain being sensitive to linezolid, amoxicillin/clavulanic acid, ceftriaxone, cefotaxime, cefepime, imipenem, trimethoprim/sulfamethoxazole, clarithromycin and minocycline. No interpretation is available for vancomycin and meropenem (MIC 0.38 and 0.008 mg/l respectively).
With these results, ceftriaxone was discontinued (4 days in total), maintaining linezolid and adding meropenem (2 g/8 h IV). Subsequently, linezolid was withdrawn after 29 days of treatment due to the patient developing thrombocytopenia, continuing on meropenem alone for a total of four weeks. During his admission, the patient developed febrile peaks and required removal of sternal wires, from which G. bronchialis was again isolated, and clinical improvement was subsequently achieved with the antibiotic treatment in conjunction with VAC therapy. Once negative cultures were obtained, the sternal wound was closed. At discharge, the patient received a course of oral ciprofloxacin (500 mg/12 h) for two weeks as home treatment.
Gordonia spp. are slow-growing, aerobic, catalase-positive, nocardioform actinomycetes. They are commonly found in soil. Biochemical tests can lead to confusion with other actinomycetes, especially Rhodococcus spp. Recently, molecular methods and mass spectrometry systems have helped to significantly improve the identification of Gordonia spp. 16S rRNA gene sequencing is an efficient but slow process, unlike MALDI-TOF.1
Infection with Gordonia spp. is rare, but has been found in patients after coronary surgery, such as sternotomy infection, bacteraemia, osteomyelitis, pleural infections and recurrent breast abscesses. It has mainly been found in intravascular catheter infections. It usually causes systemic infection in immunocompromised patients and local infection in immunocompetent patients, although invasive infections have been reported in the latter.2 There are currently no conclusive treatment guidelines for G. bronchialis infections.3
It is important to suspect this microorganism phenotypically, as it can cause invasive infections, and to differentiate it from other actinomycetes species, such as Rhodococcus spp.; as it is slow-growing, it is advisable to increase the incubation period. Mass spectrometry systems (MALDI-TOF) are a good, fast, reliable and cost-effective tool for effective identification.