This study examined the relationship of nurses’ caring behavior with the implementation of bedside handover between shifts.
MethodsA descriptive cross-sectional design was used in this study. A total of 153 nurses in three hospitals in Kepulauan Bangka Belitung Province, Indonesia took part in the study and filled out the Handover Evaluation Scale (HES) and Measuring of Nurses’ Caring Behavior (MNCB) questionnaires. Data were analyzed by performing Pearson correlation test.
ResultsThere was a statistically significant relationship between the nurses’ caring behavior and bedside handover implementation (p=0.000, r=0.537).
ConclusionNurses’ caring behavior is linked with the implementation of the bedside handover. Nurse managers are expected to improve the caring behavior of nurses and the implementation of bedside handovers by designing a supportive environment, providing periodic supervision, and conducting the evaluation.
Caring is a central attribute in the nursing profession. A caring nurse takes care of the patients with full commitment, responsibility, and respect to patients value.1 Nurses provide nursing care to patients 24h a day. Thus nurses have the longest opportunity of having interaction with patients compared to other health care professionals. One of the points of care in which nurses can have interaction with patients and their families is during clinical handover. A previous study showed that handover between shifts constitutes as much as 38% of nurses’ total working hours.2
Handover is a process of transferring responsibilities and accountability from one health care provider to another related to some or all aspects of patient care.3,4 Handover normally occurs between shifts or during transfer of the patients from a ward to a diagnostic room, between wards in hospitals, and between hospitals.5,6 Handover is carried out at least two to three times a day.7,8 Handover is of high importance for the continuous treatment process, and poor handover can lead to patient safety problems such as medication errors, delayed examination, sentinel events and even death.4,7
Studies have been suggesting bedside handover method to address many common handover issues and to improve patient involvement.9–13 Bedside handover can reduce misunderstandings and improve the accuracy of transferred information and communication.9,10 The interaction between nurses and patients can also increase through bedside handovers, while patients and families can have the opportunity to be involved in the patient care process.8,11–13 Bedside handover has shown many benefits, even though its implementation is often inconsistent both in quantity or quality. Such implementation problems are plausibly due to lack of support and leadership, no demands on nursing accountability, unaddressed obstacles, and less effective implementation planning.14 Some obstacles of the bedside handover implementation can come from the individual nurse, patient, social, and legal political factors.15
Our preliminary study conducted at three hospitals in Province of Kepulauan Bangka Belitung, Indonesia, found that bedside handover is a less common practice compared to the handover conducted between nurses at the nurse station. Bedside handover is usually done only at the beginning of the morning shift, and it hardly involves patients. There is a gap in the literature that shows how the ideal bedside handover could be interrelated with nurses’ caring behavior. Therefore, the present study aimed to describe the relationship between nurses’ caring behavior and the implementation of bedside handover between shifts in the hospitals in Kepulauan Bangka Belitung Province, Indonesia.
MethodThis study used a descriptive cross-sectional design. A total of 153 nurses in three hospitals in the Province of Kepulauan Bangka Belitung, Indonesia agreed to take part in this study. The handover implementation was evaluated using Handover Evaluation Scale (HES), a Likert-scale questionnaire developed by O’Connell et al. (2008). To assess the caring behavior, we used the questionnaire of Measuring of Nurses’ Caring Behavior (MNCB).16 Data were analyzed using descriptive statistics and Pearson correlation test. The ethical approval was issued by the Ethics Committee of the Faculty of Nursing Universitas Indonesia. We adhered to the basic principles of ethics to respect human dignity, privacy and confidentiality, justice, and beneficence principles throughout the study conduct.
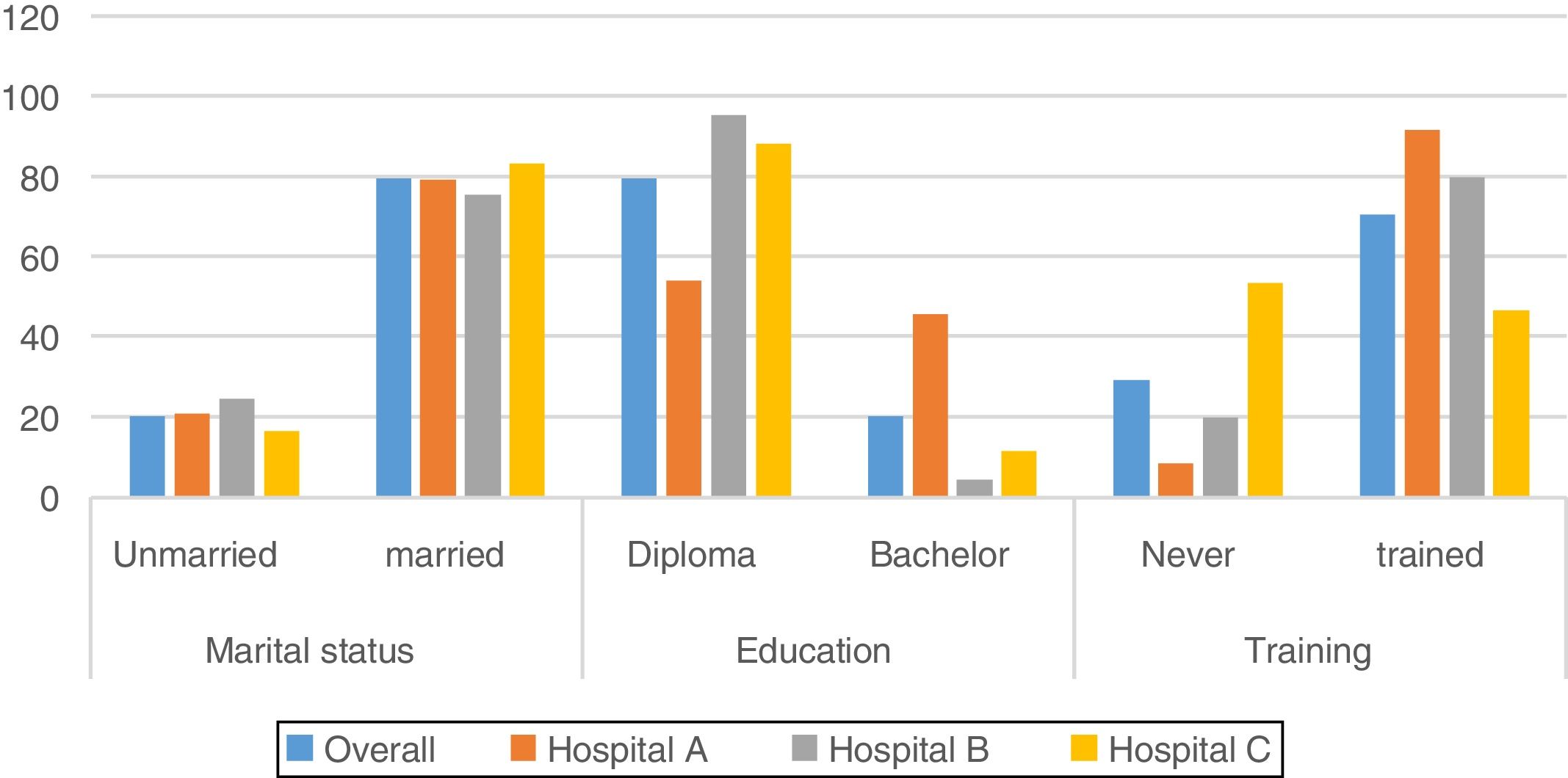
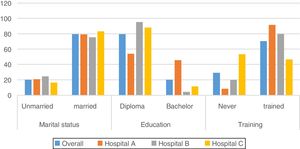
ResultsParticipant characteristicsMean age of all participants was 31.29 years (SD=4.97 years), while the mean work experience was 7.84 years (SD=4.95) (Table 1). Most participants were married (79.7%), had a diploma in nursing (79.9%), and had attended training (70.6%) (Fig. 1).
Age and work experience of the participants.
| Hospital | n | Mean | SD | CI 95% |
|---|---|---|---|---|
| Age | ||||
| Overall | 153 | 31.29 | 4.97 | 30.49–32.08 |
| Hospital A | 48 | 30.92 | 4.32 | 29.66–32.17 |
| Hospital B | 45 | 30.22 | 5.46 | 28.58–31.86 |
| Hospital C | 60 | 32.38 | 4.93 | 31.11–33.66 |
| Work experience | ||||
| Overall | 153 | 7.84 | 4.95 | 7.05–8.63 |
| Hospital A | 48 | 6.75 | 4.32 | 5.57–7.93 |
| Hospital B | 45 | 7.15 | 4.96 | 5.66–8.64 |
| Hospital C | 60 | 9.22 | 5.34 | 7.84–10.60 |
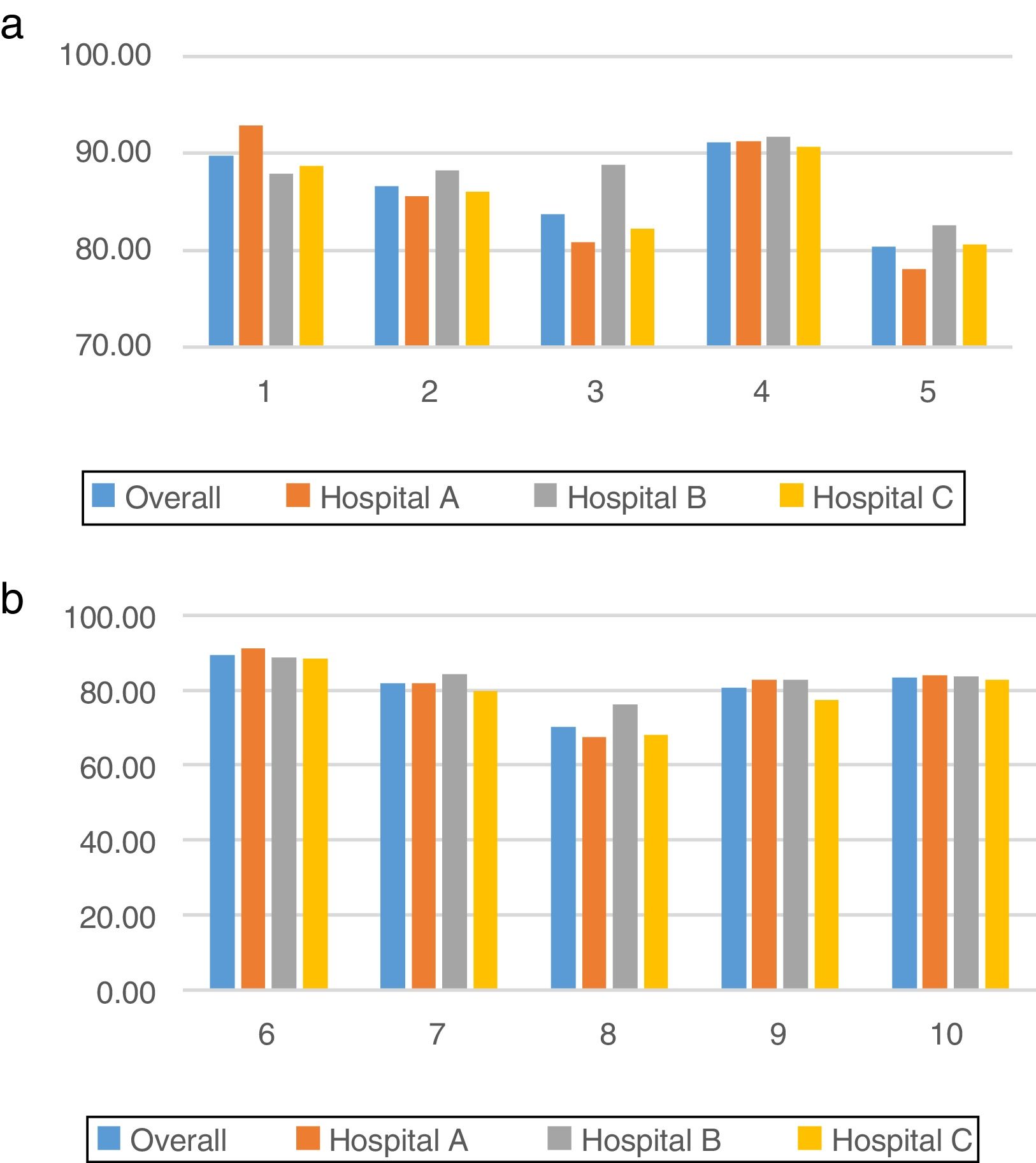
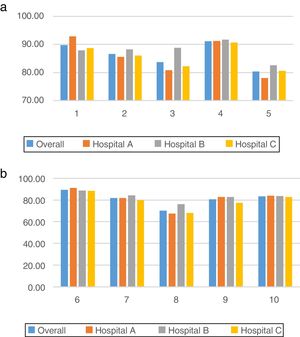
We measured the nurses’ caring behavior based on Watson's ten carative factors. Overall, the mean score of the nurses’ caring behavior at three hospitals was 85.1%. The highest mean score was gained by nurses of the hospital B (86.5%), while the lowest was scored at hospital C (83.91%). Of all carative factors, the dimension of development of a helping–trust relationship was the highest mean score (91.2%) at two hospitals (B=91.8% and C=90.7%). The highest mean score of the nurses’ caring behavior at hospital A was in the carative factor of humanistic and altruistic values (92.9%). On the other hand, the lowest caring behavior score at three hospitals (overall mean=70.4%) was of the provision a supportive environment factor (Fig. 2a).
Nurses’ caring behavior based on 10 carative factors. Note: 1. Formation of a Humanistic–Altruistic System of value; 2. Installation of Faith–Hope; 3. Cultivation of Sensitivity to ones's self and to others; 4. Development of a helping–trust relationship; 5. Promotion and acceptance of the expression of positive and negative feelings; 6. Systematic use of creative problem solving caring process; 7. Promotion of transpersonal teaching–learning; 8. Provision for a supportive, protective, and/or corrective mental, physical, societal, and spiritual environment; 9. Assistance with gratification of human needs; 10. Allowance for existential–phenomenological–spiritual forces.
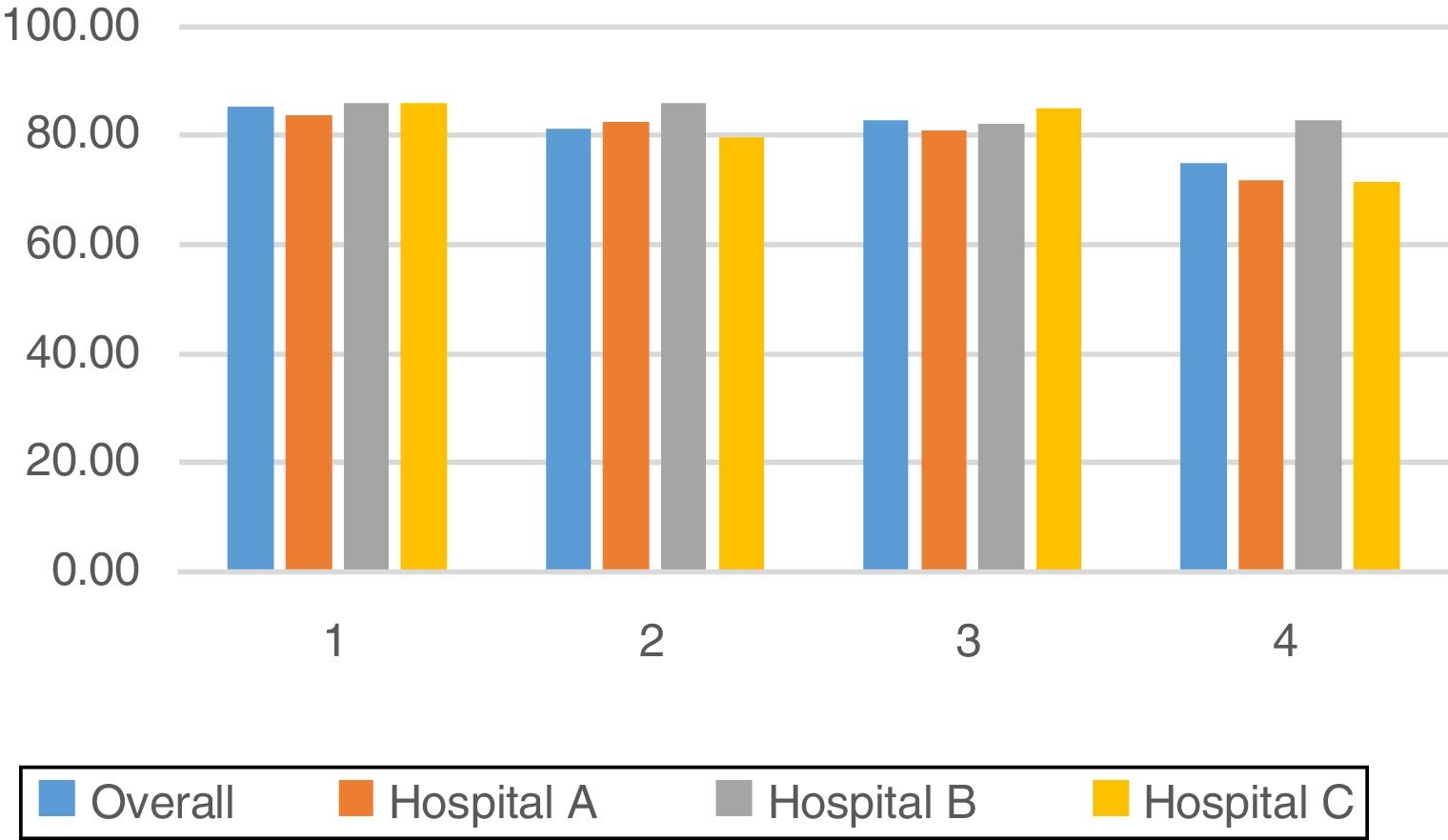
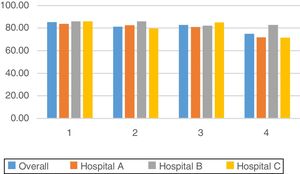
The handover evaluation measurement results yielded an average of 81.9% implementation in the three hospitals (Fig. 3). The mean scores of the four dimension of bedside handover implementation were comparable between all hospitals.
The mean score of quality of information dimension marked the highest (85.4%) in the implementation of bedside handover by the nurses in three hospitals (Fig. 3). Dimension number 4 (patient involvement) had the lowest overall mean score (75.0%) compared with the other three dimensions of bedside handover implementation. Nurses in hospital A and C scored the lowest in this particular dimension (71.9% and 71.5%, respectively).
The relationship between nurses’ caring behavior and implementation of bedside handovers between shiftsPearson correlation test results yielded a significant relationship between nurses’ caring behavior and implementation of bedside handover (p=0.000). The correlation value of 0.537 indicated that as much as 53.7% of bedside handover implementation was influenced by nurses’ caring behavior and the rest was influenced by other factors.
DiscussionCaring is a major element in nursing practice. Human relations are the basis of caring behavior, and this relationship will develop by the involvement of nurses in caring for their patients. This study found that the caring behavior scores of the nurses at three hospitals in Kepulauan Bangka Belitung province was good in general. However, caring behavior has not yet become a work culture for nurses in providing nursing care to patients. This disparity is likely to be linked with the low patient demands on nurses’ caring behavior. Many factors influence nurses caring behavior, including community culture in an area, the absence of system demands from an organization, nurses’ characteristics, and knowledge. Most patients in our study setting have a biomedical perspective of health care that they view the nurses as medical support. Their contacts with nurses are primarily related with the collaborative care done by nurses such as medication administration, intravenous catheter insertion, and alike. Patients are not aware that nurses are to provide comprehensive care that is revolved in caring behavior as the core. In Indonesian culture that has a strong family tie, the family would normally assist the patients in fulfilling their basic needs such as nutrition, elimination, personal hygiene, and other needs that do not require any specialized skills. Every patient normally has at least one family member accompanying, assisting, and chaperoning them. Therefore, the patients hardly feel the need of the nurses to address their daily basic needs while being hospitalized. They also tend to feel more comfortable to have their own family taking care of their fundamental needs, as they feel reluctant or rather inappropriate to ‘bother’ nurses for such personal necessities.
Further analysis of the ten carative factors of caring showed that the highest mean scores obtained by nurses of hospital B and C were on the carative factor of fostering the development of a helping–trust relationship. This carative factor is particularly relevant to the bedside handover. A helping–trust relationship between nurses and patients can be nurtured through intense communication for example by introducing our names while on duty, providing honest information, showing empathy, maintaining patient privacy, and always being sincerely ready while needed.1,17
With regards to the implementation of the bedside handover between shifts, nurses at hospital B mentioned that the clinical handover is commonly conducted at bedside despite the heavy workload or patient overload that occur at times. Nurses realized that the bedside handover is very important and its poor conduct may potentially be harmful to patients. Nurses at Hospital B also said that even though the implementation of bedside handover often prolongs nurses’ shift hours, but they need to do it as a standard operating procedure. Hospital B nursing management has been applying bedside handover method for a long time. Therefore, its implementation has become not only a standard practice but also a culture. Nurses carry out bedside handover consistently without being supervised. Nurses’ awareness about patient safety is one of the factors that can affect the implementation of bedside handover. In addition, nurses’ commitment to providing services according to the applicable standards is also a supporting factor of bedside handover implementation. Other factors affecting implementation of bedside handover include knowledge, barriers among staff nurses, socialization and understanding about the effect of bedside handover on patient satisfaction, availability of guidelines/standards of implementation, and leader support.14
Nurses at Hospital C, on the other hand, gained the lowest score (81.4%) of bedside handover implementation compared to other hospitals in this study. Nurses at hospital C stated that bedside handover is more often carried out only at the beginning of morning shifts (transfer from the evening shifts), as the doctor also do medical visits in the morning. Nevertheless, in some wards, bedside handovers were conducted consistently because the head nurse strictly requires bedside handover. At some other wards of which the head nurse does not have a strict ward policy about nursing handover; bedside handover is only carried out in some exceptional cases (Fig. 3).
Hospital A had a fairly similar situation with hospital B for its bedside handover implementation. The nurses mentioned that handover is more often done at the nurse station than at the bedside. The implementation of bedside handover also still encounters various obstacles in terms of frequency and quality. Nurses at hospital A were not well aware of the standard operating procedure of bedside handover. They also had a lack of understanding of the advantages of bedside handover. At this hospital, the bedside handover standard operating procedure was primarily made to fulfill the hospital accreditation demands, and it is not fully implemented in the daily practice. Obstacles faced by nurses are lack of a comprehensive guide to stages of handover, information submitted at the bedside, and nursing care plan for subsequent patients.18,19 Some contributing factors to the inconsistency of frequency and quality of bedside handover are lack of supervision from the head nurse, lack of support from the higher nursing management/leadership, low or no demand of nurse accountability, failure to overcome nurse obstacles, and ineffective planning implementation.14 Nurse managers, therefore, should prepare a comprehensive local standard to improve the bedside handover implementation.
Meanwhile, the implementation of bedside handover at hospital B marked the lowest score in the efficiency dimension. It is likely because the handover at this hospital is carried out in two places, at the nurse station, and bedside. According to the nurses of hospital B, the length of handover would vary depending on the number of patients and the complexity of the patients’ diseases. Some nurses pointed out that bedside handover would usually take more time and keep the after duty nurses staying longer at the ward. In line with this, several prior studies also showed that the bedside handovers are perceived to be less efficient as it needs a longer time.20–22 Some other studies suggested a rather different conclusion that communication with the patients and families in the bedside handovers can shorten the time needed for handover instead.23–25
Our study findings show the lowest overall score of patient involvement in the implementation of the bedside handover (74.9%). Generally, more handovers were conducted at the nurse stations, hence little patient involvement. The bedside handover also did not emphasize patient involvement. Nurses may need a standard operating procedure and training to implement effective bedside handovers with more patient involvement.
On the other hand, the dimension of information quality was the highest overall score of the bedside handover implementation in three hospitals (85.4%) This is plausible as handovers at three hospitals are conducted with verbal handovers at the nurse station using the patients’ medical record before the nurses proceed with the bedside handover. Former studies also mentioned that verbal handover accompanied by notes on the structured sheet could render more information.26,27 One of the strengths of handover done at nurse station by verbal means and using patient records is that it can help nurse transfer complete and accurate information and to prevent lost of information.
Bedside handover allows patients and families to engage more with nurses and nursing care. Studies also found that bedside handover can improve quality of care for patients, enhance patient safety, improve information accuracy, increase patient and nurse satisfaction, improve critical thinking skills and decision making, increase nurse accountability, improve documentation completeness, as well as facilitate assessment and evaluation process at same time.21,23–25 Moreover, bedside handover can also prevent miscommunication and improve coordination between nurses, and patients/families.28
Open communication between nurses, patients, and families can improve patient safety. Communication will help nurses, patients, and families to understand the goals, obstacles, and limitations of patient care. In the bedside handovers, the process of communication both verbally and nonverbally occurs. Listening to patients with empathy can build a helping–trust relationship between nurses and patients. Fostering a helping–trust relationship is Watson's fourth carative factor that forms the basis of bedside handovers. The helping–trust relationship can be promoted through keen communication of the nurses for example by providing honest yet understandable information and showing empathy and readiness to help the patients.1,17
Our statistical results show that the development of a helping–trust relationship has the highest score on the nurses’ caring behavior (91.2%). With such a high score, the nurse–patient interaction is supposedly excellent. According to the patients, nurses are friendly, caring, call patients with their names, respond to patient's call quickly, assess patient's complaint, but they find nurses rarely introduce themselves at the initial contact with the patients. Nurses may miss this essential part of handover because of lack of a comprehensive guide to conducting bedside handover or lack of reinforcement of the basic communication practice in nursing.18 A standard guide for implementation of bedside handover is therefore needed. Standardization is useful to regulate time, suitability, and structure of the handover, and to promote the involvement of the patients and families in the handover to support safe patient care. Standardized format assists nurses in documenting and transferring information as well as enhancing nurses’ ability to plan nursing care for patients.19
Furthermore, interpersonal communication of the nurse manager to the staff nurses e.g. giving attention, responding, clarifying, supporting, giving feedback, conveying information, appreciating experiences, and using humor are expected to increase the application of bedside handover standard operating procedure and to promote caring nurse behavior. A manager must be able to carry out his/her functions in supervising the implementation of bedside handover, assessing its implementation and improving if there are deficiencies and motivating the staff nurses to provide the best nursing care.29 Application of the standard bedside handover must be supported by a strong commitment of the nurses and nurse managers.11 Nurses’ interaction in handover should reflect the nurse's caring behavior toward patients. When nurses nurture an interpersonal teaching and learning environment, nurses empower patients to be more actively involved in the decision making process and implementation of their care.10,30
In three hospitals, the lowest dimension of nurses’ caring behavior is provision for a supportive environment (68.2% of the total score). Our interviews with the patients reveal that nurses rarely offer spiritual care such as facilitating patients to worship, but they usually motivate patients to pray for healing. Creating an environment that supports mental health and spirituality and respects human dignity is the eighth carative factor according to Jean Watson. The supportive environment encompasses the nursing concepts to maintain safety, privacy, and comfort by controlling the environment outside the patients. This is done so that the patients feel they are in a safe environment. Nurses must maintain the patient's privacy while doing bedside handover, for example by asking if the patient wants his/her family stay during bedside handover or not.28 Visitors apart from the immediate family are generally requested to wait outside during the bedside handover to maintain the patient's privacy.
Internal and external environment affects individual health. Internal environment includes mental and spiritual needs as well as individual socio-cultural beliefs. Patient comfort can be promoted by controlling physical environmental factors such as regulating room temperature, changing position, taking care of the eyes and mouth, and helping patients to meet their daily needs.17 While conducting bedside handover, nurses can check the surrounding environment of the patients including bell and things around the patient, and scrutinize patient's medication list. Caring nurses hold a higher commitment and responsibility for patient safety. As Nightingale noted, although a nurse does not care for the patients at any time, a nurse would still check the safety of patients ‘surrounding environment.28
Handover is a communication process whereby a nurse who has completed her duty provides information related to some or all aspects of the patient such as patient's identity, illness history, treatment history, nursing priorities, and subsequent nursing plans.21 It can be concluded from the findings of this study that nurses’ caring behavior is linked with the implementation of the bedside handover. Nurse managers are expected to improve the caring behavior of nurses and implementation of bedside handovers by designing a supportive environment, providing periodic supervision, and conducting the evaluation.
Conflict of interestsThe authors declare no conflict of interest.
This work is supported by HIBAH PITTA 2018 funded by DRPM Universitas Indonesia No. 1848/UN2.R3.1/HKP.05.00/2018.
Peer-review under responsibility of the scientific committee of the Second International Nursing Scholar Congress (INSC 2018) of Faculty of Nursing, Universitas Indonesia. Full-text and the content of it is under responsibility of authors of the article.