To compare closed and open endotracheal suction system in relation to ventilator-associated pneumonia in adult intensive care unit patients
MethodSystematic review.
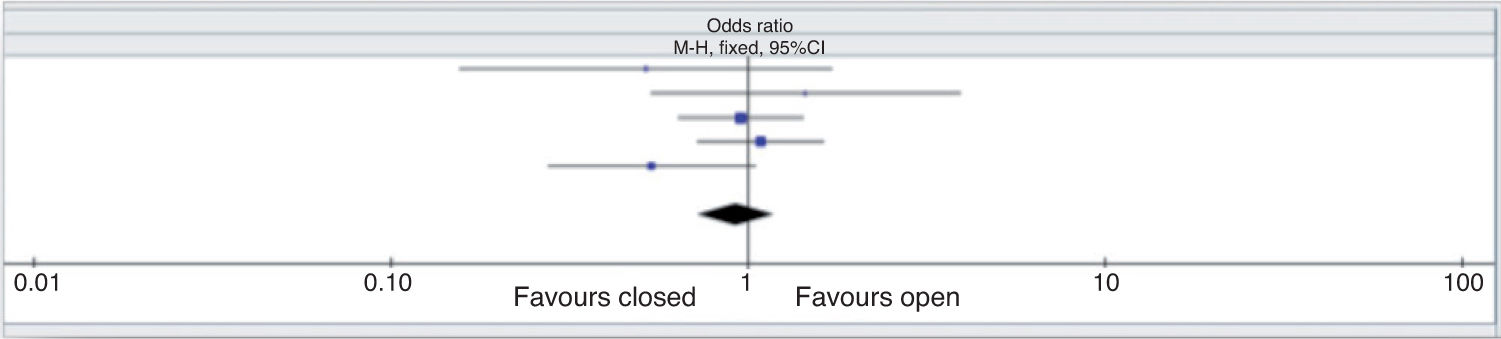
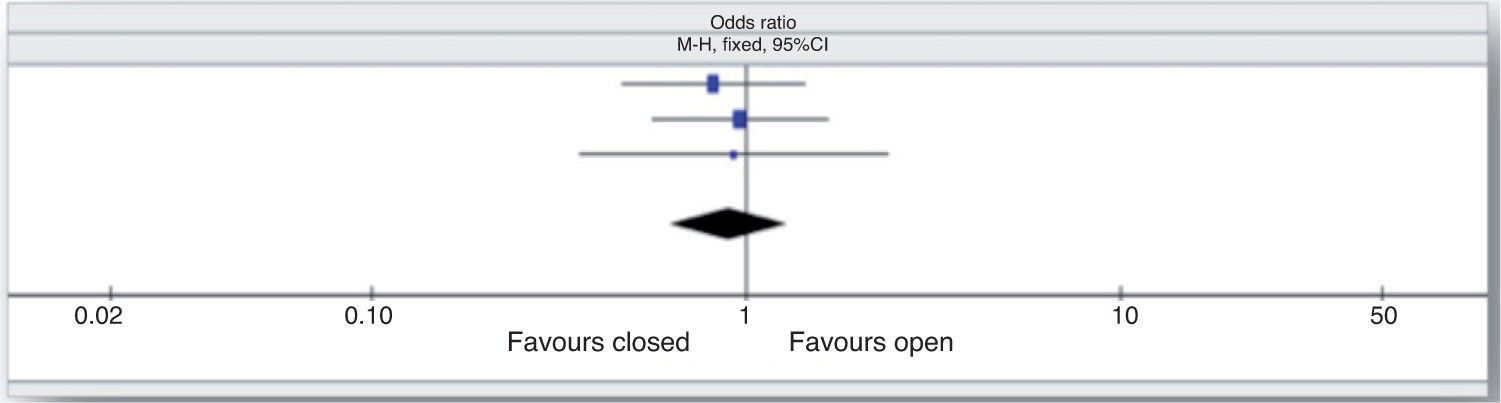
ResultsOf the 18 eligible studies identified through the search strategy, only 5 studies were included in the review. The two endotracheal suction systems show no differences in the incidence of ventilator-associated pneumonia (5 trials: odds ratio [OR], 0.92; Mantel-Haenszel [M-H], fixed; 95% confidence interval [95%CI], 0.72-1.18) or mortality rates (3 trials: OR, 0.89; M-H, fixed; 95%CI, 0.62-1.28).
ConclusionsResults from 5 studies showed that suctioning with either closed or open endotra-cheal suction did not have an effect on the incidence of ventilator-associated-pneumonia or mortality rates. Therefore, more rigorous and large-scale research is needed for further evaluation.
Ventilator-associated pneumonia (VAP) is a common nosoco-mial infection in the hospital, particularly in the intensive care unit (ICU). This infection is increasing among patients with mechanical ventilation (MV) because of the invasive endotracheal tube (ETT) (Ruffell, 2004; Tablan et al, 2004).
VAP is a complication condition caused by the multidrug-resistant microorganism Acinetobacter baumannii, a frequent nosocomial pathogen among patients who undergo MV (Garnacho-Montero et al, 2003). Generally, mechanically ventilated patients have salivary secretion impairment, which stimulates the number of bacteria excessively, and which can easily cause VAP (Mori et al, 2006). However, several other factors are correlated with the presence of VAP, including routine invasive procedures.
VAP is diagnosed if patients have all the following clinical criteria: body temperature lower than 35.5 °C or higher than 38 °C, chest radiograph showing new or progressive infiltrates, white blood cell counts of >10,000 mm3 or < 4000/mm3, culture of significant respiratory secretions (tracheal aspirate of >106 CFU/mL, bronchoalveolar lavage of >104 CFU/mL, or protected brush catheter of >103 CFU/mL) or blood culture coinciding with the culture of the respiratory secretion (Lorente et al, 2006). However, another study mentioned that VAP diagnosis could be establish if patients present with at least 2 of the criteria (Topeli et al, 2004; David et al, 2011).
The incidence of VAP ranges from 6.8% to 44% among ventilated patients in the adult ICU. Chastre and Fagon (2002) cited by SARI Working Group (2011) revealed that crude mortality rates in patients with VAP significantly increased from 24-50% to 76% if the infection was caused by multi-resistant organism (SARI Working Group, 2011). One study also stated that VAP is a major contributor to high morbidity and mortality in ICU patients (Munro and Ruggiero, 2014). The risk of VAP is ten times higher in mechanically ventilated patients compared to non-ventilated in-patients (Combes et al, 2000). Moreover, VAP causes several secondary disadvantages to ICU patients, including being two times more likely to die, prolonged length of hospitalization and higher medical costs (Peter et al, 2007; SARI Working Group, 2011).
Suctioning is the intervention that is most frequently performed on mechanically ventilated patients. There are two types of suctioning systems, which are closed suction and open suction. The open suction system is performed by disconnecting the breathing circuit and inserting suction catheter into an ETT (Blackwood and Webb, 1998). Furthermore, this disconnection could be the opportunity for cross infection and hypoventilation (Johnson et al, 1994; Maggiore et al, 2002). To address these possible complications, closed suction was introduced. Closed suctioning is performed without disconnecting the respiratory circuit and using multi-use catheters, which is safer for patients on MV (Peter et al, 2007; Subirana et al, 2007; Peter et al, 2007).
Over the last two decades, most of the research on hospital-associated pneumonia has been focused on VAP. Because VAP is a consequential condition, many strategies have been employed to reduce the risk of its development of VAP (Vonberg et al, 2006; Siempos et al, 2008). One current strategy to reduce VAP is by the modification of suction-ing; several studies found that closed suction is more advantageous in preventing the spread of VAP than open suction (Niel-Weise et al, 2007; Subirana et al, 2007).
There are opposing views regarding endotracheal suction. Although this procedure is beneficial, therefore, it increases the risk of developing VAP. A few studies have shown different results about the beneficial effects of each endotracheal system (open and closed suction) on the development of VAP (Topeli et al, 2004). Furthermore, several studies hypothesised that closed suction could reduce VAP proliferation by decreasing environmental contamination. In contrast, open suction has been reported to be linked with arterial desaturation, inability to maintain PEEP (positive end expiratory pressure) and cardiac arrhythmia, especially in patients with cardiorespiratory instability (Peter et al, 2007). Although preliminary studies reported that closed suction somehow reduced the risk of developing respiratory infection, the relationship between VAP and types of suction remains questionable (Vonberg et al, 2006; Siempos et al, 2008). The aim of this systematic review is to evaluate if there is a difference between open endotracheal suction and closed endotracheal suction on the incidence of ventilator-associated pneumonia in mechanically ventilated ICU patients.
MethodsA systematic review was carried out in the Cochrane Central Register of Controlled Clinical Trials (CENTRAL), Ovid Medline 1948 to June 2015 (MEDLINE), CINAHL Plus Text 1982 to June 2015 (CINAHL) and EMBASE 1950 to June 2015. The author performed searches of CENTRAL, MEDLINE, CINAHL and EMBASE using a similar search strategy
Only English-language randomized controlled trials (RCTs) were included in this systematic review and could not include non-English studies due to the translation that this would entail. All mechanical ventilated patients who were intubated for more than 48 h were included in this review. Adult ICUs were included. All adult patients (aged 18 years old and above) were included.
All citations were screened based on title, keywords and abstract. Duplicates were deleted by using EndNote X7. Secondary searches based on the reference list of articles from the primary search were conducted and appropriate papers were identified. One researcher did the above primary and secondary collection of literature. All articles were reviewed by one author and verified by one of the other authors who were a supervisor. Disagreements regarding inclusion were resolved by consensus discussion.
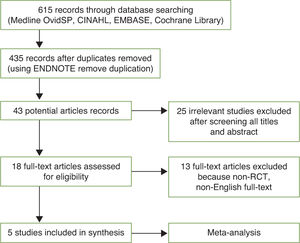
Only quantitative studies were included in the review, which relevant to the research question. Several studies were excluded from the review because of not meeting the inclusion criteria, e.g. non-RCT studies, non-English studies, non-ICU settings, comparing specific diagnoses, patients were intubated before admission to ICU, and comparing specific brands of catheter suction. During the systematic review process, the authors independently assessed the included studies in order to minimize the risk of selection bias. The authors followed PRISMA flow chart as the search strategy framework. Critical appraisal was focus on selection, performance, attrition and detection. Furthermore, the author used the CASP (Critical Appraisal Skills Programme) tool for appraising RCT studies.
This tool was used because it involves the following criteria: patient selection (eligibility criteria, baseline comparability), patient allocation (randomization, allocation concealment), blinding (patient, care giver, observer, clinician, and statistician), intervention (co-interventions, compliance), outcome measurement (adverse events) and statistics (intention-to-treat analysis). The findings from all quantitative studies were extracted from the research form and compiled into a table identifying the characteristics of each study.
The author conducted independent data extraction using JBI Trial tool (MAStArI Critical appraisal tool Randomized Control), which resulted in scoring from 6 to 10. This tool consists of 10 questions that represent the weight of articles' quality. These characteristics included randomization, blinding (to treatment allocation), concealment, blinded outcome, and follow-up of participants, treatment comparable or equal to groups, reliable measurement and statistical analysis. After scoring, the author documented a brief description on another form including: the author, date and location of study, participants and numbers, intervention, setting and treatment, outcome measures and results.
The results were relevant to the research question being analyzed and Meta-analyses are performed to summarize studies that address the same hypothesis and results in the same way. The first researcher did the analysis whereas the second researcher was reviewed and advised with no disagreement.
ResultsPrior to searching on any specific databases, the author registered herself to each database. The first search was conducted on 9th January 2015 until 23rd June 2015. In consequence of a comprehensive literature, there were initially 615 prospective studies recorded from all databases.
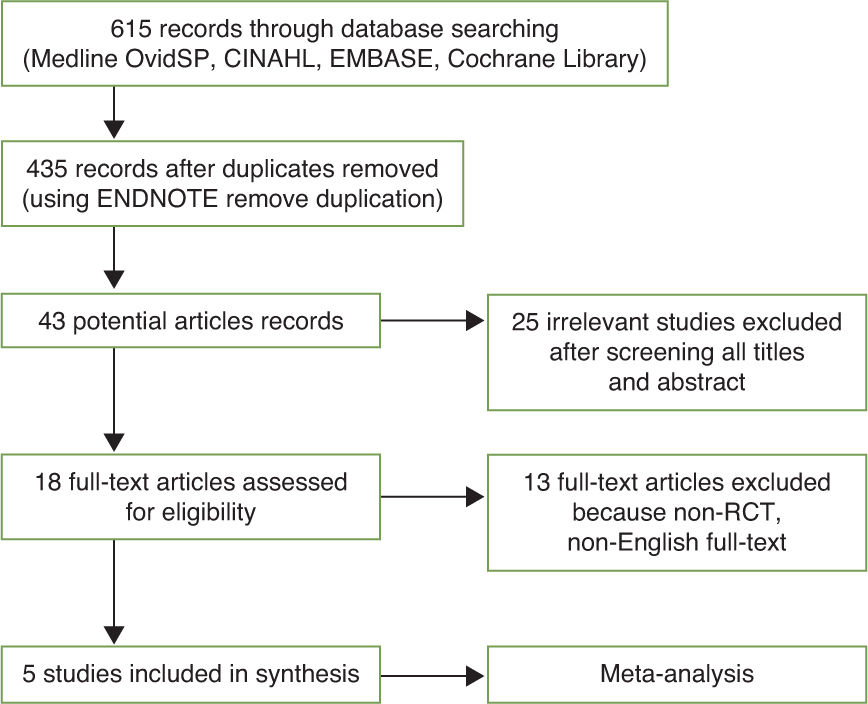
The author traced any duplication of the literatures by End-Note X7, which removed 180 duplicates, shortening the list to 435 studies. The assessment by screening the titles and abstracts resulted in 43 potential articles being maintained. The subsequent screening removed a further 25 irrelevant studies. In result, 18 full-text articles were assessed for eligibility in detail, of which 13 were excluded for not meeting inclusion criteria, such as not being RCTs (n = 8) and not being English full-text articles (n = 5, comprising 1 Chinese, 1 Korean, 1 Farsi, 1 Portuguese and 1 Spanish study). Thus, 5 studies were ultimately identified as fulfilling all inclusion criteria and were subsequently included in this review (Figure 1).
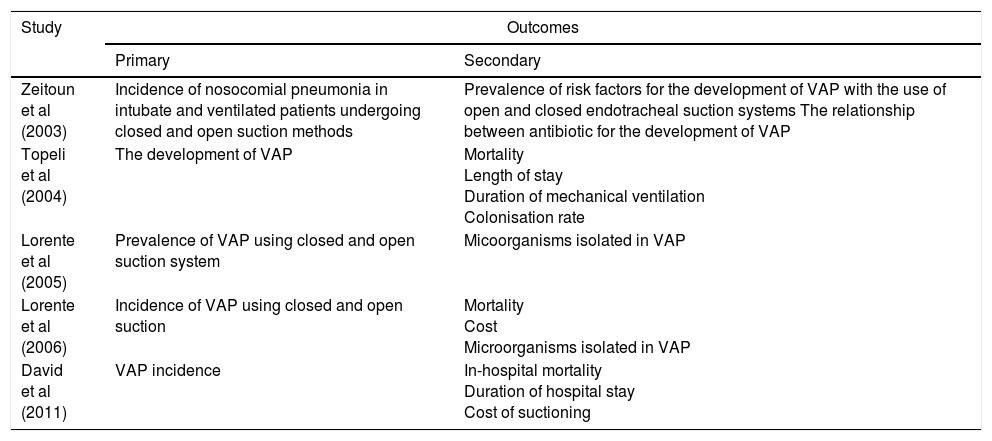
Five eligible trials (Zeitoun et al, 2003, Topeli et al, 2004; Lorente et al, 2005, Lorente et al, 2006; David et al, 2011) were identified and included in this review. Therefore, all trials were conducted in very diverse countries such as Turkey, Spain (2 studies), Brazil and India but in the similar setting; which adult ICU. Five trials reported VAP incidence as primary outcome and 3 trials (Topeli et al, 2004; Lorente et al, 2006; David et al, 2011) measured mortality as the secondary outcome (Table 1). There are no trials that compared other than closed and open endotracheal suction comparison.
Outcome measures of 5 studies
| Study | Outcomes | |
|---|---|---|
| Primary | Secondary | |
| Zeitoun et al (2003) | Incidence of nosocomial pneumonia in intubate and ventilated patients undergoing closed and open suction methods | Prevalence of risk factors for the development of VAP with the use of open and closed endotracheal suction systems The relationship between antibiotic for the development of VAP |
| Topeli et al (2004) | The development of VAP | Mortality Length of stay Duration of mechanical ventilation Colonisation rate |
| Lorente et al (2005) | Prevalence of VAP using closed and open suction system | Micoorganisms isolated in VAP |
| Lorente et al (2006) | Incidence of VAP using closed and open suction | Mortality Cost Microorganisms isolated in VAP |
| David et al (2011) | VAP incidence | In-hospital mortality Duration of hospital stay Cost of suctioning |
Based on demographic data, there were 1225 patients in the 5 studies. A total of 615 patients were treated with open endotracheal suctioning system, 29% of which acquired VAP, and 610 patients were treated with open endotracheal suc-tioning system, of which similar 29% suffered VAP. Generally, the sample sizes used in all studies were very different, ranging from 47 to 457 participants, with a median of 200. The methods of randomization included computer-generated from Excel (or other) software to have closed or suction intervention and randomized at the time of intubation (depends on event or odds dates).
All participants were adult patients aged 18 years old and above; the average age was 57.73 years old in open suction and 55.01 years old in closed suction. However, only four studies mentioned the mean age (David et al, 2011; Lorente et al, 2005; Lorente et al, 2006; Topeli et al, 2004), and those studies only included males, whereas Zeitoun et al (2003) did not mention the sex of participants. The severity of patients' diagnoses were being assessed and recorded by Acute Physiology and Chronic Health Evaluation II (APACHE II) Score, CPIS (Clinical Pulmonary Infection Score), and Glasgow Coma Scale (GCS).
All trials randomized the patients to closed or open endo-tracheal suction. Only 3 studies specifically mentioned the type of closed suction or brand of multiple-catheter. There were Topeli et al (2004) used Steri-Cath endotracheal closed suction (Steri-Cath, Sims Portex, Unites States), Lorente et al (2005 and 2006) used Hi-care endotracheal suction (Mallinckrodt, Mirandola, Italy).
In the group that receiving closed endotracheal suctioning, suctioning was performed using multiple catheters that were not routinely changed every day. Topeli et al (2004) and Lorente et al (2005 and 2006) mentioned that closed suction was replaced when it was grossly soiled, presented mechanical failure, or if the patient needed re-intubation. David et al (2011) maintained the use of closed suction for one week, while Zeitoun et al (2003) did not mention the use of closed suction.
Even though the types of closed suction were different, the open suction control was definitely the same for all trials. All trials used the same method while performing open endotracheal suction. This means that before performing endotracheal suction, the patient should be hyper-oxygenated before the breathing circuit is disconnected from the ventilator, then single-use catheter will be inserted through the ETT to aspirate the secrets.
In order to measure the incidence of VAP, 3 studies did the measurement with tracheal swab. Topeli et al (2004) did the first culture of endotracheal swab 48 h after intubation then continued on alternate days until extubation or patient withdrawal (death). Similarly, Lorente et al (2005 and 2006) measured VAP by doing tracheal aspirates twice a week and lastly at the moment before extubation. Furthermore, they also measured micro bacteria causing VAP; however, at the first stage all studies preferred to check the presence of clinical criteria and used specific tools to diagnose VAP.
The 5 trials measured the incidence of VAP between closed and open endotracheal suction as the primary outcome. Additionally, 3 of the 5 studies measured mortality. Because of the similar outcome, meta-analysis was conducted in order to have precise and vigorous results. In spite of all studies measuring VAP incidence, several studies made different findings.
Zeitoun et al (2003), Topeli et al (2004), and Lorente et al (2005) found that types of endotracheal suction system had no effect on the development of VAP outcome in ICU. However, Lorente et al (2006) found that closed suction without daily change is the optimal option for patients needing suction longer than four days.
David et al (2011) found that closed endotracheal suction might be advantageous in reducing the incidence of VAP, particularly late-onset VAP. Furthermore, 3 out of 5 trials also measured the secondary outcome of mortality rate. Topeli et al (2004), Lorente et al (2006) and David et al (2011) found that the average mortality rate in open endotracheal suction was 13.8%, while in closed endotracheal suction it was 13.6%. The statistical result based on meta-analysis (forest plot) is discussed in the following section.
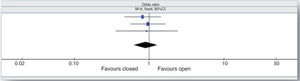
Meta-analysisAll included studies resulted in the same primary outcome that measuring the incidence of VAP on closed endotracheal suction versus open suction. This means that the outcome was both clinically and statistically homogenous and could be pooled for meta-analysis. These studies, which involved 1225 patients grouped into experimental (closed endotracheal suction) and control (open endotracheal suction) groups, comprising 615 patients in the control group and 610 patients treated by closed endotracheal suction.
The analysis of these studies found that there was no statistically significant difference between VAP incidence on closed endotracheal suction compared to open endotrache-al suction (odds ratio [OR], 0.92; Mantel-Haenszel [M-H], fixed; 95% confidence interval [95%CI], 0.72-1.18). This suggests that the use of closed endotracheal suction did not decrease or could not prevent the development of ventilator-associated pneumonia when compared with open endo-tracheal suction (Figure 2).
Meta-analysis of 3 studies (David et al, 2011; Lorente et al, 2006; Topeli et al, 2004) that looked at the mortality rate as the complication of VAP also demonstrated that there was no statistically significant difference between closed endotracheal suction and open endotracheal suction (OR, 0.89; M-H, fixed; 95%CI, 0.62-1.28). This implies that both patient groups had equal mortality complications (Figure 3).
DiscussionThe effect of closed and open endotracheal suction in the ventilator-associated pneumonia incidenceSeveral studies from 15 years ago, proposed closed endotra-cheal suction as a strategy to decrease VAP incidence on the mechanical ventilated patients that opposed with open en-dotracheal suction. In respect to Wagh (2009), there was a newer development to prevent VAP, include: the use of sub-glottic ETT, continuous suctioning of the subglottic secretions, specially designed cuff ETT, and specially designed closed tracheal suctioning system, such as closed system.
However, this was negatively correlated with the result of meta-analysis of our current 5 studies. Meta-analysis of 5 studies (David et al, 2011; Lorente et al 2006; Lorente et al, 2005; Topeli et al, 2004; Zeitoun et al, 2003) showed that, here is no significant difference between VAP incidence on the closed and open endotracheal suction group. Both studies reported a similar risk for ventilator-associated pneumonia in both closed and open endotracheal suction (heterogeneity: chi-squared = 5.35; df = 4; P = .25; I2 = 25%). In conclusion, closed endotracheal suction could not prevent the development of VAP.
Interestingly, even though the result of meta-analysis found that generally there is no difference in the incidence of VAP but David et al (2011) found that closed endotra-cheal suction was associated with a trend of reducing the incidence of VAP. This shown when the outcome tested for superiority (odds ratio, 1.86; 95% CI, 0.91-3.83; P = .067) found that closed endotracheal suction having a benefit (P = .067) in terms of VAP reduction, particularly for late-onset VAP (P =.03). This finding, therefore, matched with the previous study by Combes et al (2000) which found that the use of closed endotracheal (Stericath in particular) reduced the incidence rate of VAP without any side effect (Combes et al, 2000). Nonetheless, a study of David et al (2011) used only clinical criteria to diagnose VAP without any other diagnoses method. On the contrary, four other studies used another measurement besides clinical criteria, such as: throat swab cultures. This could be the possible factor that influencing the result of VAP incidence on both group. In addition, the result of all studies showed that types of endotracheal suction had no effect on the development of VAP incidence.
MortalityOne study presumed that the death case might be caused by VAP which occurred to the patients who admitted to the ICU (Chawla, 2008). According to Chawla (2008), VAP incidence in Asian countries is quite raising, which was ranging from 3.5 to 46 per 1000 ventilator days. Several studies in Asian countries revealed that VAP case significantly increasing in most countries, for example in India, Thailand, and Korea.
However, the implication meta-analysis of 3 studies may oppose to that previous study. Meta-analysis of 3 studies (David et al 2011; Lorente et al, 2006; Topeli et al, 2004) found that there is no statistically different on the mortality rate caused by VAP on both groups. This means that either closed or open endotracheal suction systems had no relation to the mortality (heterogeneity: chi-squared = 0.18; df = 2; P = .91; I2 = 0%). This also suggested that closed endotracheal suction could not decrease the number of mortality that caused by ventilator-associated pneumonia. In addition, in Topeli et al (2004) found several following factors, such as: older age, high APACHE II score, low GCS, pulmonary causes, duration of intubation (MV), and development of VAP were the predictors that could increase mortality. In addition, David et al (2011) found that patient who treated endotracheal suction experienced lower duration MV.
ConclusionsSuctioning is an important procedure for patients with artificial airway support particularly in the ICU. However, it should be performed using an aseptic technique, universal precautions, and also in-line with current guidelines. This review demonstrates that there is no difference in the incidence of VAP and mortality rate between open and closed endotracheal suction systems. Hence, it is not possible to recommend one method of suctioning, over another based upon VAP incidence or mortality rates. However, there may be other factors, such as cost, which might favor one method. The cost of implementing open or closed suctioning was outside the scope of this review.
There were many concerns relating to study design, quality and sample sizes. Future studies should address quality standards identified in quality assessment tools. Apriority sample size calculations should be conducted so that sample sizes are sufficient to identify differences in clinical outcome.