The objective of this study was to identify the impact of implementing community health nurse assistance for high-risk pregnant women on utilization of health services.
MethodThe study was quasi experimental with a control group design. The sample included high-risk pregnant women in 10 community health centers in Indonesia who were selected by consecutive sampling. The total sample included 66 women in both the intervention and the control groups. The high-risk pregnant women in the intervention group received nurses’ assistance during the third trimester and until giving birth. Before and after the intervention, the knowledge, attitudes, and behavior of the women were measured.
ResultsThe average scores for the knowledge, attitudes, and behavior of women in the intervention group increased. Differences were found in health care utilization between the two groups. All women in the intervention group received antenatal care during the third trimester more than once and were assisted by skilled health personnel during childbirth, while in the control group 10.6% of respondents were assisted by a paraji shaman (traditional birth attendant). All women in the intervention group accepted family planning, and the contraceptive choice varied.
ConclusionsThe assistance of community health nurses improves the knowledge, attitudes, and behavior of high-risk pregnant women and positively impacts the rate of health care utilization.
The maternal mortality rate (MMR), an indicator of the health of mothers, has remained high in Indonesia. The Demographic Health Survey of Indonesia (Survey Demokrasidan Kesehatan Indonesia (SDKI) found that maternal deaths jumped sharply for the 2007 to 2012 period1.
One strategy to reduce the rate of maternal deaths is the greater involvement of health providers, who have traditionally been mostly doctors or midwives. However, a number of studies have concluded that the integration of nursing and midwifery can improve the quality of maternal health2. In this context, community health nurses can work with mothers and families to promote proper health practices. Under this strategy, nurses hold key roles during the care of pregnant women through the screening and the assessment of antenatal risk factors throughout pregnancy3.
Data shows that 86.68% of mothers in 2014 received antenatal care and attended four medical visits, which is less than the target of 95%, as stated in the Health Ministry's Strategic Plan. About 88.68% of deliveries were assisted by professional care providers, which was slightly under the Health Ministry's target of 90%4.
Furthermore, nurses represent the highest number of health providers in primary, secondary, and tertiary care. For this reason, the provision of nurse assistance during pregnancy can be one solution for optimizing maternal care and for enabling women with high-risk pregnancies to utilize health services at a higher rate5.
The hypothesis of this study was that nurse assistance can significantly improve the utilization of health facilities by high risk pregnant women, while the minor hyphotesis was improving knowledge, attitude, and behavior high risk pregnant woman could be done through implementing of nurses assistance.
MethodThis research utilized a quasi experimental design with a control group. This research adhered to ethical principles and was approved by the Ethical Committee of the Faculty of Nursing, University of Indonesia (Universitas Indonesia).
High-risk pregnant women who met the inclusion criteria were included in the study, following a consecutive sampling technique. The inclusion criteria were high risk pregnant women with one of the Four T criteria (Too old, Too young, Too often childbirth, Too near the distance between delivery) and in the third trimester pregnancy. The determination of the required number of subjects using different hypothesis tests indicated that a minimum of 30 subjects were required. To account for potential drop out, the required number of subjects plus 10% was used, resulting in a sample of 33 women for both the intervention group and the control group, or 66 high-risk pregnant women in total. The intervention group received assistance accompanied by home visit by community health nurse.
Independent variable in this research is knowledge, attitude and behaviours of high risk pregnant women. Dependent variable in this research is Indicators of health care utilization include the number of antenatal care visits during pregnancy, place of delivery and birth attendance. The measurement of the independent variables for the intervention group was performed twice: before the intervention and three months after intervention. These measurements were separated by three months since pregnant women were first interviewed in the third trimester of pregnancy and were expected to have given birth by the second interview three months later, thus allowing researchers to assess the effect of the intervention. The control group was only interviewed once during pregnancy. The measurement of the dependent variable for both the intervention and control groups was carried out postpartum6.
Data were collected using instrument to measure the knowledge, attitudes, and behaviours of high risk pregnant woman, and postpartum observations were made to identify the use of the facilities for antenatal care (ANC) and examination, place of delivery, and acceptance of family planning measures. Type question for knowledge include understanding of risk pregnancies, signs and risks of risky pregnancy, physical and psychological complications, actions when complications occur and family planning. The instrument consists of 30 questions. Reliability test using covarian item procedure with Cronbach alpha formula with value 0,763. Attitude questions include positive and negative attitude responses in addressing the high risk conditions experienced. The instrument consists of 25 questions. Reliability test using covarian item procedure with Cronbach alpha formula with value 0,822.
The data then were analyzed using t-test and logistic regression.
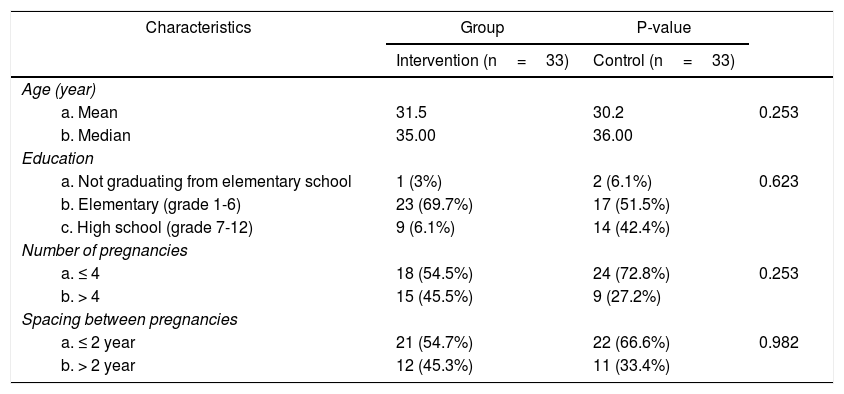
ResultsTable 1 shows the distribution of respondents by age, education, and number of pregnancies. The characteristics of the respondents of the intervention group did not significantly differ from those of the control group. The proportion of respondents with high-risk pregnancies was 54.5% in intervention group and 72.8% in the control group. Pregnancies were considered high risk for women who had previously birthed more than four children. Meanwhile, 54.7% of mothers in the intervention group had been pregnant within the previous two years in comparison to 66.6% of the control group.
Demographic characteristics of high-risk pregnant women in the intervention and the control groups at 10 health centers in Cianjur, West Java, in 2015.
| Characteristics | Group | P-value | |
|---|---|---|---|
| Intervention (n=33) | Control (n=33) | ||
| Age (year) | |||
| a. Mean | 31.5 | 30.2 | 0.253 |
| b. Median | 35.00 | 36.00 | |
| Education | |||
| a. Not graduating from elementary school | 1 (3%) | 2 (6.1%) | 0.623 |
| b. Elementary (grade 1-6) | 23 (69.7%) | 17 (51.5%) | |
| c. High school (grade 7-12) | 9 (6.1%) | 14 (42.4%) | |
| Number of pregnancies | |||
| a. ≤ 4 | 18 (54.5%) | 24 (72.8%) | 0.253 |
| b. > 4 | 15 (45.5%) | 9 (27.2%) | |
| Spacing between pregnancies | |||
| a. ≤ 2 year | 21 (54.7%) | 22 (66.6%) | 0.982 |
| b. > 2 year | 12 (45.3%) | 11 (33.4%) | |
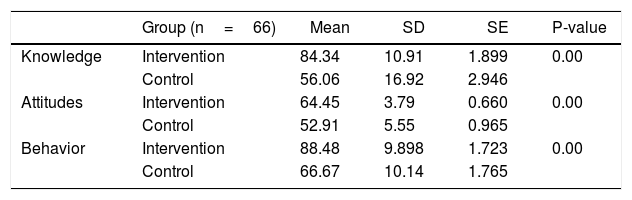
Table 2 shows knowledge, attitudes, and behavior of high-risk pregnant women in intervention and control groups. There are differences of knowledge, attitude, and behavior of high-risk pregnant women in intervention and control group, which is indicated by the value of knowledge, attitude, and behavioral significance of 0.00 (P value < 0.05).
Overview of the knowledge, attitudes, and behavior of high-risk pregnant women at 10 health centers in Cianjur, West Java, in 2015.
| Group (n=66) | Mean | SD | SE | P-value | |
|---|---|---|---|---|---|
| Knowledge | Intervention | 84.34 | 10.91 | 1.899 | 0.00 |
| Control | 56.06 | 16.92 | 2.946 | ||
| Attitudes | Intervention | 64.45 | 3.79 | 0.660 | 0.00 |
| Control | 52.91 | 5.55 | 0.965 | ||
| Behavior | Intervention | 88.48 | 9.898 | 1.723 | 0.00 |
| Control | 66.67 | 10.14 | 1.765 |
Knowledge high risk pregnant women for pre and post intervention groups are generally included in 30 items covering five themes: Understanding risk pregnancy (9 items), signs and risk of pregnancy at risk (7 items), physical complications that may occur during pregnancy, childbirth and childbirth In pregnant women at risk (8 items), knowing what to do when complications occur (2 items) and Family Planning (3 items). Attitudes of high risk pregnant women of intervention groups pre and post intervention are generally contained in 25 items that include attitudes toward positive attitude response Pregnant women at risk in responding to high risk conditions experienced (12 items), and attitude toward negative attitude response Pregnant women at risk in responding to the condition high risk experienced (13 items). Behavior high risk pregnant women for pre and post intervention intervention groups are generally contained in 15 items that include behaviors capable of determining the choices to be undertaken and engaging in activities that lead to behaviors that support hazardous conditions with routine pregnancy check-ups at health facilities as well as delivery at facilities Health services (10 items), and behav-ior received support from the family (husband) associated with the decision to be made in the maintenance of her condition (5 items).
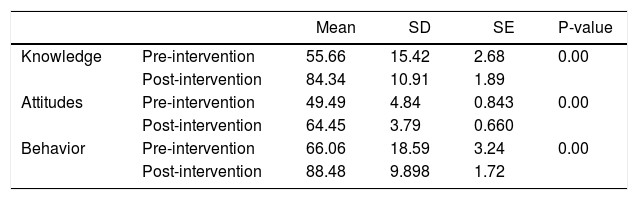
Table 3 shows a significant improvement (P=0.00) in the knowledge, attitudes, and behavior of high-risk pregnant women in the intervention group following intervention by a nurse. These results prove the minor hypothesis that high-risk pregnant women who received interventions will have the knowledge, attitudes, and behavior to appropriately manage their pregnancies and health. For the intervention group, the average mean scores for knowledge increased from 55.66 before the intervention to 84.34 after the intervention. For attitudes and behaviors, the mean scores increased from 49.49 to 64.45 and from 66.06 to 88.48 before and after the intervention, respectively.
Knowledge, attitudes, and behavior of high-risk pregnant women (n=33) in the intervention group, before and after intervention by nurses.
| Mean | SD | SE | P-value | ||
|---|---|---|---|---|---|
| Knowledge | Pre-intervention | 55.66 | 15.42 | 2.68 | 0.00 |
| Post-intervention | 84.34 | 10.91 | 1.89 | ||
| Attitudes | Pre-intervention | 49.49 | 4.84 | 0.843 | 0.00 |
| Post-intervention | 64.45 | 3.79 | 0.660 | ||
| Behavior | Pre-intervention | 66.06 | 18.59 | 3.24 | 0.00 |
| Post-intervention | 88.48 | 9.898 | 1.72 |
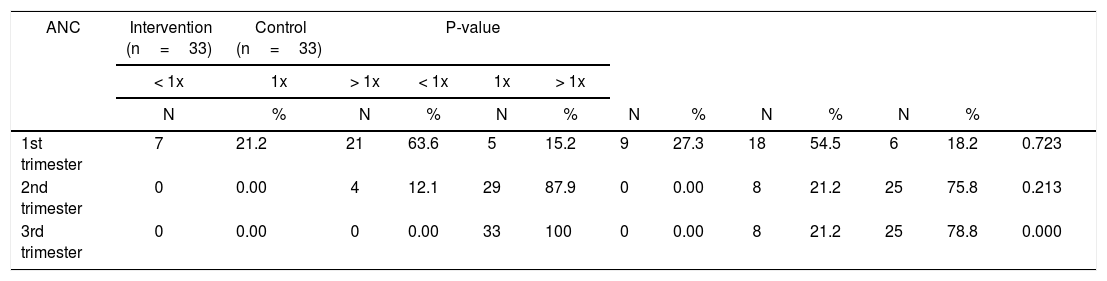
Table 4 highlights that no differences were found in the utilization of antenatal care between the high-risk pregnant women of the intervention and the control groups in the first and the second trimesters. However, for antenatal care in the third trimester, a significant difference (P=0.00) was found between the intervention and the control groups. While 100% of high-risk pregnant women in the intervention group received antenatal care more than once, this percentage lowered to 78.8% for the control group. The additional 21.2% of women in the control group received antenatal care only once during the third trimester.
Differences in receival of antenatal care (ANC) between high-risk pregnant women (n=66) of the intervention and the control groups.
| ANC | Intervention (n=33) | Control (n=33) | P-value | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| < 1x | 1x | > 1x | < 1x | 1x | > 1x | ||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | ||
| 1st trimester | 7 | 21.2 | 21 | 63.6 | 5 | 15.2 | 9 | 27.3 | 18 | 54.5 | 6 | 18.2 | 0.723 |
| 2nd trimester | 0 | 0.00 | 4 | 12.1 | 29 | 87.9 | 0 | 0.00 | 8 | 21.2 | 25 | 75.8 | 0.213 |
| 3rd trimester | 0 | 0.00 | 0 | 0.00 | 33 | 100 | 0 | 0.00 | 8 | 21.2 | 25 | 78.8 | 0.000 |
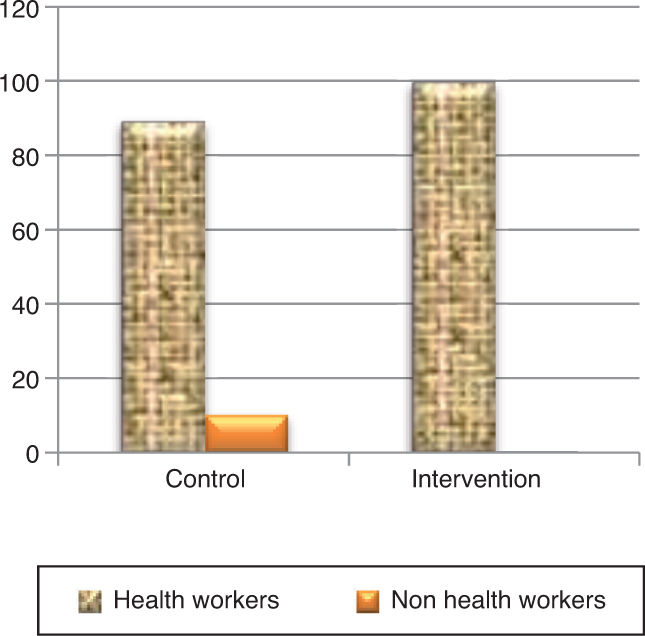
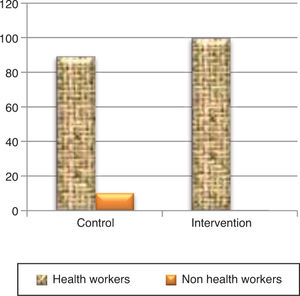
Figure 1 shows that 100% of high-risk pregnancies in the intervention group were attended to by health personnel at delivery in comparison to 89.4% of pregnancies in the control group. In the latter group, 10.6% of women were attended to by non-health personnel (paraji shaman). These differences were significant (P=0.00).
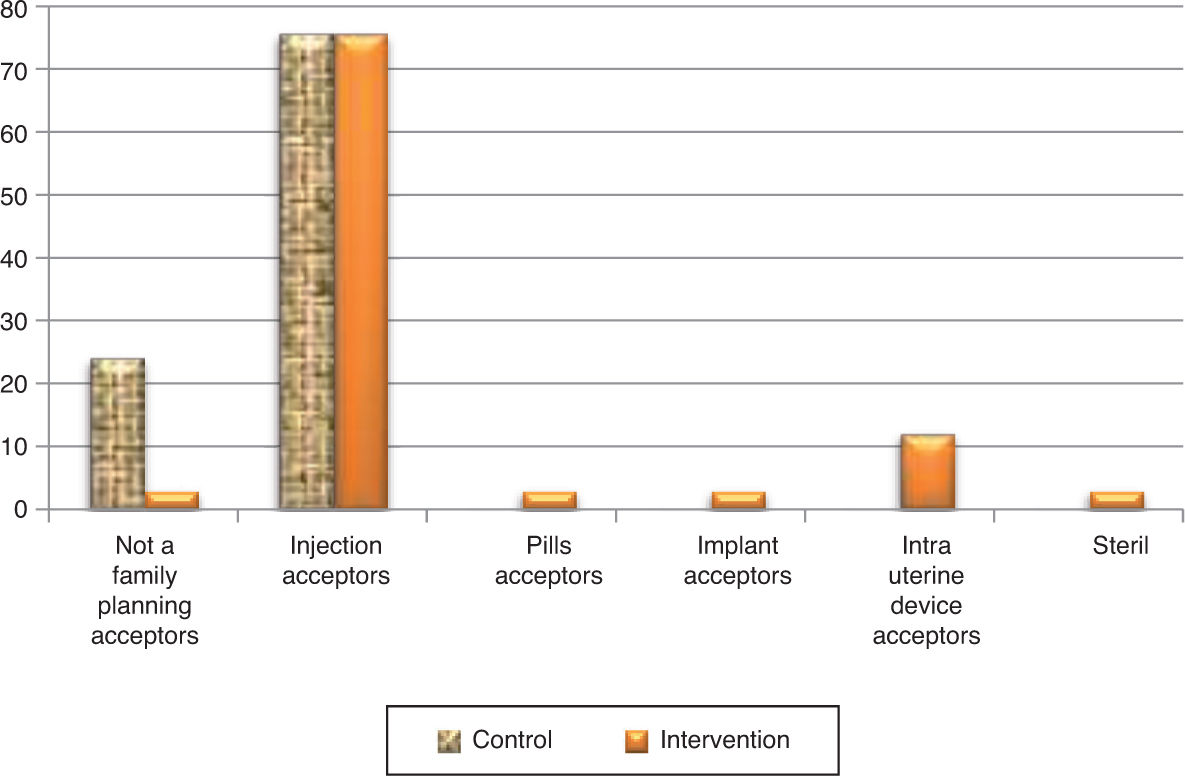
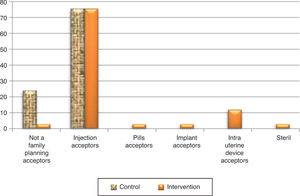
Figure 2 indicates the type of birth control that high-risk pregnant woman chose following delivery. The most common method chosen by respondents in both the intervention and the control groups is injection, including 75.8% of women in the intervention group and 75.8% of women in the control group. In the intervention groups, a percentage of women (12.1%) opted for intrauterine devices (IUD) in addition to implants (3%), pills (3%), and injections (3%). The number of high-risk pregnant women who refused family planning was largest in the control group (24%), whereas only 3% of the intervention group rejected family planning.
DiscussionImprovements in the knowledge, attitudes, and behavior of high-risk pregnant women is expected to improve the health outcomes of both these mothers and their children.
The American Nurse Association7 stated that the role of community health nurses in maternal care is to help families achieve and maintain an optimal balance between the personal needs of family members, including high-risk pregnant women, and family functions. Nurses can provide services to clients and families who are at risk, thereby preventing or attending to actual health problems as well as improving environment health in order to guarantee women's reproductive health. Nurses can also help to detect changes in health status and deviations from the optimal development, provide appropriate interventions and treatment, and refer women to the appropriate professionals in order to improve their health or recovery from potential diseases.
The results of the present study are consistent with research that considers public health nursing initiative[s] to promote antenatal health.” The activities of nurses in the community is often associated with family health and the promotion of healthy practices. In this sense, public health nurses occupy opportune positions for screening and assessing risk factors in pregnant women during antenatal care. From this research, nurses were shown to have important potential functions in primary prevention and education in the community3.
The analysis showed that the utilization of health facilities during antenatal care is influenced by knowledge. In other words, pregnant women who have knowledge of the importance of health services are more likely to receive adequate antenatal care. In this sense, the cognitive domain, or one's knowledge, is important for determining one's actions (overt behaviors). Research has shown that experiences and behaviors based on knowledge will be more lasting than behaviors not based on knowledge8.
The positive utilization of health care by high-risk pregnant women in the intervention group supports the four elements of innovation diffusion theory proposed by Rogers. The implementation of public health nurses in maternity care is a new approach that may benefit pregnant women who are at high risk in the community. Previously, women have been more familiar with obtaining care from doctors, midwives, or healers (paraji), who have been the main sources that pregnant women consult to obtain pregnancyrelated services or to address childbirth problems9.
In the control group, seven respondents gave birth assisted by a shaman paraji. As indicated by the nurses, these women tended to have more confidence in paraji shamans and believed them to be experienced in the birth process. Also, the high cost of labor and economic barriers may dissuade women from seeking skilled health personnel. Although this was not a topic of the present research, in the intervention group that was provided with health education, some respondents also requested continued enrollment in the national health insurance (JKN) plan in health centers in anticipation of labor.
The type of contraception most commonly adopted by the intervention and the control groups was injectable contraceptives. In the intervention group, several variations were witnessed in the choice of contraceptive IUD, implants, pills, or sterility with respect to the control group. Even so, some respondents rejected family planning. In some cases, the respondents were housed in boarding schools and did not anticipate becoming pregnant again, while others did not wish to make a decision without their husbands’ permission.
The present findings were also in line with several other studies. Haider, who conducted a qualitative study on childbearing and contraceptive decisions among Afghan men and women, suggested that education was of key importance for women's health, especially in the use of modern contraceptives. In this case, due to the low level of education and mobility of some women, the education of husbands was found to be likely to enable better family (wife) access to and use of modern contraceptive care10. Wagstaff inferred that the behavior of women or their low utilization of health services are affected by the quality and availability of health services, health financing, and infrastructure such as roads in addition to cultural norms, environmental factors, and housekeeping practices11.
The results of the present study supported the potential role of nurses in primary prevention and education in the community. Similarly, Olds, in his study on the “Effect of nurse home visiting on maternal life course and child development,” concluded that prenatal home visits by nurses improved the quality of life of both women and children12.