This study was aimed at developing and testing an instrument that can be used to evaluate self-efficacy for mobilization.
MethodPhase 1 was a qualitative study carried out through interviews. Phase 2 involved determining the content validity and testing the instrument legibility. Phase 3 involved ascertaining construct validity through a first order confirmatory factor analysis.
ResultsIn phase 1, seven themes were identified and used as bases for establishing the indicators of each self-efficacy dimension. In phase 2, a content validity 0.75–1 was obtained. In phase 3, valid items that measure the level, strength, and generality dimensions have four, six, and seven items, respectively.
ConclusionThe end product of the study was a concise and valid instrument that measures the self-efficacy of the patient for mobilization during hospitalization.
The prescription of bed rest for patients is widely implemented practice in hospital despite long-standing knowledge of the physiological and psychological effect of such treatment. Researchers showed that 83% of patients lie in bed throughout hospitalization and that 73% of patients who were able to walk after treatment did not engage in walking exercises during their stay in hospitals.1 The various conditions experienced by patients during hospitalization are a major obstacle to mobilization. Among these obstacles, the most commonly occurring are physical symptoms, such as weakness, pain, and fatigue; the placement of devices such as intravenous lines and urine catheters; fear of falling; and lack of staff assistance during patients’ off-bed activities.1
Nurses play an important role in optimizing the ability of patient's move. Nursing intervention intended to maintain patient mobilization is a fundamental activity in nursing care.2 Currently, an effort to satisfy the needs for patient mobilization continue to focus on improving physical ability, less attention is paid to enhancing psychological ability.1
It has been stated that a sufficient assessment of mobilization in nursing care encompasses both physical and psychological evaluation. A patient's ability to move is also influenced by psychological factors, among these factors, self-efficacy is the strongest determinant of the extent to which activities can be performed.3
The role of self-efficacy in the execution of action has been demonstrated in numerous studies, with research probing into issues such as the effects of self-efficacy on balance, daily activity, and adherence to exercise regimens.4 Some experts claimed that high self-efficacy could improve a person's ability to achieve a certain target beyond his/her actual capabilities,4 for example, indicated that self-efficacy could predict an individual functional ability. An assessment of the limitations of a person, ability combined with adequate self-efficacy can facilitate desired enhancements to abilities.4
Identifying self-efficacy for mobilization is an important task for nurses because this can help them determine appropriate nursing interventions for improving the ability of patients to move and thereby accelerates healing and prevent the negative effects of immobilization on both physical5–8 and psychological well-being.9,10 The problem is that no assessment instrument has been established for this purpose. This deficiency highlights the need to conduct research on developing and validating mobilization self-efficacy instruments that can serve as a reference for hospital nurses. Accordingly, this study developed an instrument for assessing self-efficacy for mobilization. To this end, a qualitative study was carried out (phase 1), the content validity of the designed instrument was determined (phase 2), and its construct validity was ascertained (phase 3).
MethodsPhase IDesignPhase 1 was conducted to explore matters relating to each self-efficacy dimension, namely, level, strength, and generality.11
SampleA total of 10 participants were selected via purposive sampling on the basis of the following criteria: compos mentis, lower limb muscle strength of at least 4, ability to get out of bed and sit beside the bed with or without help (from other people or the use of devices), and understanding of Bahasa Indonesia. The exclusion criteria were oxygen administration at more than 2 liters per minute, placement of a chest tube and/or a central line, and fever.
Measurement and procedureData were collected using interview guides prepared by the researchers, and interview sessions were recorded using an MP4 device. The interviews were aimed at exploring the indicators that can explain each of the self-efficacy dimensions conceptualized by Bandura11 as part of his self-efficacy theory.
After sampling, informed consent was obtained from the respondents. In-depth interviews that lasted for 30–60min were carried out, and the sessions were transcribed through textual description. The transcripts were then analyzed using the methods developed by Colaizzi to identify themes that can be used as bases for developing the indicators of the assessment instrument created in the current work.
Phase 2DesignA descriptive design was implemented in phase 2 of the research, in which the face and content validity of the instrument was determined on the basis of expert judgment and a test of the instrument's legibility.
Sample (expert and patients)Eight experts evaluated the developed instrument, and five participants were involved in the legibility testing. After the experts were selected, informed consent was obtained from them. The inclusion criteria applied to the selection of the legibility test participants were the same as those implemented in the first stage of the study.
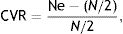
Measurement and procedureContent validity analysis was performed on 30 instrument items. Each of the self-efficacy dimensions (level, strength, and generality) consists of 10 positive items. The assessment was carried out using a Likert scale ranging from 0 to 3 (0=“not sure”, 1=“less sure”, 2=“sure”, and 3=“very sure”). Each expert scored each item using four options: 1 for “poor”, 2 for “less”, 3 for “good”, and 4 for “excellent”. Items that were scored 1 and 2 were then classified as non-essential items, whereas those rated 3 and 4 were categorized as essential items. The content validity ratio (CVR) of the items was calculated using Eq. (1), where Ne denotes the items rated as essential, and N represents the number of experts. Items with a CVR less than 0.75 were excluded from the instrument.12
The legibility test was conducted to determine whether the instrument items are clearly stated and understood. On the basis of the results, further evaluations and revisions were made. The elimination of unfavorable items was expected to strengthen the validity of the instrument. The results of phases 1 and 2 were used as bases in phase 3.
Phase 3DesignSimilar to phase 2, phase 3 was also of a descriptive design, directed toward ascertaining the construct validity of the instrument.
SampleA sample of 306 patients admitted to the department of internal medicine in four hospitals in Bandung City, West Java, Indonesia was recruited for this phase. The inclusion and exclusion criteria were the same as those applied in phases 1 and 2.
Measurement and procedureThe results of phase 1 (face and content validity) and phase 2 (legibility) were used. As previously stated, the instrument has 30 items, which are distributed across the level, strength, and generality dimensions (10 items each).
Construct validity was determined using first-order confirmatory factor analysis (CFA) run on the Mplus 7.4 program. The instrument's fitness was evaluated using the root mean square error of approximation (RMSEA). An RMSEA <0.05 indicates satisfactory model matching. The validity test via CFA was performed with the following steps: (1) A unidimensional fit model was obtained, and (2) items with a negative loading factor and non-significance were excluded.
ResultsPhase 1The results of phase 1 revolve around patient characteristics and the thematic analysis conducted in the qualitative study.
Characteristics of participantsAmong the participants, three were men and seven were women with an age range of 22–72 years. Educational attainment varied from elementary to university level. Four of the participants were employed, and six were unemployed. All the participants had a muscle strength of 5 and were hospitalized for 3–6 days.
Results of the qualitative thematic analysisThe seven themes obtained were as follows:
- a.
In-bed mobilization of patients: Typical movements are changing of positions, sitting, and getting out of bed.
- b.
Off-bed mobilization of patients: Usual movements are sitting on a chair, walking around the bed, walking out of the room.
- c.
Physical barriers to mobilization: The physical obstacles that are perceived by patients as affecting mobilization are a weakness, tiredness, pain, dizziness, difficulties resulting from infusion therapy, and catheter placement.
- d.
Psychological barriers to mobilization: The psychological barriers that are perceived by patients as affecting mobilization are laziness, feelings of discomfort with other patients, and fear of prohibition by doctors and nurses.
- e.
Facility- and support-related barriers to mobilization: The facilities/support that patients need for mobilization are sticks, wheelchairs, and assistance from people in walking.
- f.
Mobilization required to satisfy daily needs: The daily mobilization activities that patients need to engage in are sitting down when eating and drinking, walking to the toilet, and walking to the nurses’ station.
- g.
Mobilization for health improvement: Mobilization during hospitalization is often exercised for the purpose of improving health and not to satisfy the need for daily activity.
These themes were developed into indicators of the dimensions for measurement, see Table 1.
Dimensions, indicators, number of items in the mobilization self-efficacy instrument.
| Dimension | Indicator | Number of items |
|---|---|---|
| Level | In-bed mobilization | 2 |
| Off-bed mobilization | 8 | |
| Strength | Physical barriers to mobilizing | 3 |
| Psychological barriers to mobilization | 4 | |
| Facility-/support-related barriers to doing mobilization | 3 | |
| Generality | Mobilization to meet daily needs | 5 |
| Mobilization for the improvement of health | 5 |
The CVRs of the instrument items are listed in Table 2. As can be seen, none of the items exhibited values below 0.75. Thus, all the items were incorporated into the instrument.
Results of legibility testThe instrument was generally evaluated as understandable, unambiguous, and unrepetitive. All the items qualitatively passed the test, requiring only some grammatical revisions.
Phase 3Characteristics of participantsAmong the 306 participants, 38.24% were young adults, and 32.03% were older adults; 84.97% had a muscle strength of 5, and 46.08% were assessed as having a good capability for mobilization. Males accounted for 56.53% of the sample.
Results of construct validity analysisThe results of the construct validity analysis are presented in Table 3. The RMSEA values were below 0.05, and the Prob.RMSEA values were above 0.05. Thus, the items were regarded as valid measurements of each dimension.
Results of item analysisThe description and factor loading of each valid item are provided in Table 4.
Description and factor loading items.
| Dimension and item | Description | Factor loading |
|---|---|---|
| Level | ||
| L1 | Sitting stable on a chair for more than 10min | 0.88 |
| L2 | Rising from a sitting position to a standing | 0.89 |
| L3 | Standing for more than 10min | 0.84 |
| L4 | Walking more than 10 steps | 0.83 |
| Strength | ||
| S1 | Mobilize even though the body is weak | 0.57 |
| S2 | Mobilize even though no one gives praise/motivation | 0.73 |
| S3 | Mobilize despite laziness | 0.73 |
| S4 | Mobilize despite lack of walking aids (wheelchair, cane, crutch) | 0.91 |
| S5 | Mobilize although unaccompanied by hospital staff/family | 0.85 |
| S6 | Mobilize despite the absence of special places for mobilization training | 0.88 |
| Generality | ||
| G1 | Sitting on a chair/bed during each eating and drinking task | 0.68 |
| G2 | Walking to nurses’ station to ask for help | 0.81 |
| G3 | Bathing in the bathroom | 0.70 |
| G4 | Sitting on a chair/bed at least 5 times a day | 0.77 |
| G5 | Walking exercise (at least 10 steps) once a day | 0.85 |
| G6 | Exercising outside room | 0.89 |
| G7 | Maintaining mobilization despite boredom | 0.80 |
Many studies have produced various self-efficacy instruments that are intended to determine self-efficacy for physical activity, functional self-efficacy, general self-efficacy, and self-efficacy for exercise.13–17 By contrast, no research has been devoted to the development of instruments that assess the self-efficacy of patients for mobilization during hospitalization. The present study is the first to develop such instrument.
The level dimension of mobilization self-efficacy focuses on the extent of patient confidence in the ability to complete mobilization tasks of different difficulty levels. Strength emphasizes the extent to which patients believe that they can overcome their illnesses with strong effort to engage in movement despite constraints and obstacles. Physical, psychosocial, and facility-related barriers affect a patient's mobilization ability.1,18 Generality describes a patient's belief in his/her ability to complete mobilization for broad tasks or those confined to a particular situation. Mobilization is also aimed at increasing activity tolerance, maintaining cardiovascular function, ensuring appropriate breathing, and achieving normal elimination patterns.2
The CFA results showed that the items in the developed instrument were significantly correlated with each of the self-efficacy dimensions. The valid items derived for the level, strength, and generality dimensions amount to 4, 6, and 7, respectively. The RMSEA values were below 0.05. Other studies on the development of self-efficacy instruments derived a goodness-of-fit value of 0.95, an RMSEA of 0.06, and a standardized root means square residual of 0.08 Hu and Bentler.19
Concerning the item analysis results, some of the items were excluded because they were excessively correlated with the other items. Only the valid items were included. A four-point Likert scale was used in the evaluation as providing more than two response options allows for more variability and renders a scale more sensitive to the relationship between psychosocial and behavioral variables.17 Some instruments on self-efficacy also use the same scale.13,16,17
The current instrument differs from other self-efficacy measurements in that the targets are hospitalized, patients. The mobilization tasks described in the instrument are those specific to mobilization under such conditions (i.e., hospitalization) and are not found in other self-efficacy instruments. Powell and Myers's (1995) Activities-specific Balance Confidence Scale, for instance, assesses the self-efficacy of the elderly for maintaining balance in performing daily tasks.3,20 The Falls Efficacy Scale developed by Tinetti (1990) assesses the self-efficacy of the elderly for performing daily tasks without falling.3,21 The Self-Efficacy for Functional Activities Scale developed by Resnick (1999) also assesses the elderly's self-efficacy in performing daily tasks.3 The Perceived Physical Activity Self-Efficacy Scale assesses self-efficacy for physical exercise from childhood to adolescence (school age).17
The results showed that the instrument items are valid measurements of mobilization self-efficacy, but the findings still require further validation because factor scores were used in analyzing the data collected using the instrument. Thus, future research should be devoted to additional analyses with tests of parallelity between items via second-order CFA. In addition, a limited sample of internal medicine patients was recruited. Further research with varied scopes, from backgrounds of diseases, rooms, and geographic and cultural differences, is needed. Other scholars should also determine the role of self-efficacy in a patient's mobilization ability.
A concise and valid instrument for measuring self-efficacy for mobilization during hospitalization has been produced. The instruments include three self-efficacy dimensions, namely, level (four items), strength (six items), and generality (seven items), all of which are valid measures.
Conflict of interestsThe authors declare no conflict of interest.
This work is supported by Hibah PITTA 2017 funded by DRPM Universitas Indonesia No.375/UN2.R3.1/HKP.05.00/2017.
Peer-review under responsibility of the scientific committee of the Second International Nursing Scholar Congress (INSC 2018) of Faculty of Nursing, Universitas Indonesia. Full-text and the content of it is under responsibility of authors of the article.