This study aimed to describe the relationship between the score of sequence organ failure assessment (SOFA) and the length of time of vventilatoruse by patients hospitalized in Intensive Care Unit.
MethodThis research is analytic observational with a cross-sectional design. Data collected include age, sex, diagnosis medic, length of stay in ICU, length of ventilator use and SOFA score. The SOFA components include respiratory, platelet, liver, neurology, cardiovascular, renal and urine output in 24h. The data platelet and liver were collected based on the new data. The respiratory data used FiO2/SaO2; Neurological data used Glow Coma Scale value; and cardiovascular data used mean atrial pressure value (MAP). Each organ system is assigned a point from 0 to 4. The SOFA scores range from 0 to 24. The highest score is defined as the worst condition. This instrument was created by the European Society of Intensive Care Medicine. The number of samples was 40 patients who admitted in ICU for two days minimum. The data were collected in two months by a team. Data collected were analyzed by percentage, mean, and fisher exact to see the relationship of SOFA score and duration to use the ventilator. The data were analyzed by Fisher exact statistic because there are three cells have expected account less than 5.
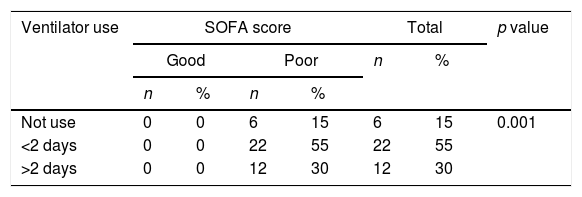
ResultsMajority of the respondents admitted in the ICU caused of neurological function with mean of SOFA score of 7.78 (score minimum is 4 and score maximum 12). The duration used ventilator majority less than 3 days (55%). The result shows that there was the relationship between the score of SOFA with duration to use ventilator (p value <0.01). The highest score of SOFA is indicating more severity of the function of organ respiratory.
ConclusionsSOFA score is one instrument for evaluating the severity and prognosis of the patients.
As the patients entering the ICU really need monitoring, one of the tools that can be used is the sequential organ failure assessment (SOFA) scoring. Organ dysfunction can be identified as an acute change in Sequential (Sepsis-related) Organ Failure Assessment score ≥2 as a consequence of infection.
SOFA scores include 6 organ functions, namely respiration, coagulation, liver, cardiovascular, central nervous system, and kidneys are chosen based on the literature review, each of which has a value of 0 (normal function) to 4 (very abnormal) which gives the possibility of values from 0 to 24. SOFA scoring is not only assessed at one time, it can also be assessed periodically by looking at the increase or the decrease in the score. The variable assessment parameters are said to be ideal for describing organ dysfunction or failure. The main objective of scoring organ failure is to describe the sequence of complications, not to predict mortality.
Organ dysfunction is a process that often occurs in patients who experience critical illness due to serious illness. Evaluation of organ dysfunction every time the treatment in the ICU is very helpful in following disease development and can provide a strong correlation picture with the end result of ICU care. A number of physiological parameters are used to define organ dysfunction, such as lung, cardiovascular, renal, hepatic, hematological, and central nervous systems.
The most common failure in patients admitted to the ICU is the failure of respiratory function to require a ventilator machine to maintain their lives. Patients with ventilators are very skilled at the disease, often called ventilator-associated pneumonia. This will also weigh on other organ functions so that the condition can be increased to accelerate other organ failures.
Assessing organ dysfunction in patients admitted to the ICU is one method that can also be used to reduce death. This assessment is also a continuous assessment of valuing and solving the problem that often gives a sense of satisfaction to the customer and achieving the quality technical education.
The SOFA must be measured for all patients treated in the ICU to differentiate the level of anger and mortality. Information from the SOFA review can also see the prognosis of the patient's severity. It can also improve the percentage of patients in his family, as well as can be used for the condition experienced by the most convenient for intervention. The SOFA is used for the measurement of severity in serial and functional organs on a serial basis every day.1 Although the value of the level of severity of the Acute Physiology and Chronic Health Evaluation Simplified Acute Physiology Score based on the first 24h in the ICU is very different from the SOFA, it covers all of the participants in the participation cycle as a whole. This is what nurses must do to maintain the entire disease process.6
Formulation of the problemICU patients who require ICU care need to do triage specifically for an effective and en efficient work system and the quality of service provided. The treatment given to patients is also a continuation and can require a very long time. For an additional treatment, the assessment of the disease of the sufferers is especially affected in patients who use ventilators as respiratory aids because the length of the use of ventilators will affect all the organs of the patients related to infection and oxygenation. Based on the rationales and considerations, the problem of this study is formulated as: what is the relationship between length of time of ventilator use and SOFA score?
MethodResearch locationThis research was conducted in the Intensive Care Unit of the Hospital Arifin Achmad Pekanbaru. This research site was chosen as it is a reference to the ICU in Riau Province. It is also the place for practice of medical and nursing students and nearly 50% of those treated using a ventilator.
This research was carried out for two months in which the measurement conditions used the form to determine the health status of patients. The samples used in this research are patients being treated in the ICU who admitted in ICU from outside submissions and the ventilator is mounted. The samples were forty patients who used ventilators selected using accidental sampling technique.
Types and sources of dataThe data to be measured from the samples are data related to the demographic data, medical diagnosis, long day care, ventilator mode, and scoring the SOFA covering the functions of liver, heart, lungs, and kidneys, neurological and bodily fluids. The data were obtained by looking at the results of laboratory examination, physical examination, observation of the monitor or the daily chart.
Data collection techniquesThe results of the SOFA examination laboratory were taken from the results of the last examination that was close to when taking data. The data were about platelets, liver function (bilirubin) and PaO2 and creatinine. For the values of MAP, GCS and FiO2 as well as fluid balance, they were taken when the research project was undertaken.
SOFA scoring was calculated using an observation sheet. The SOFA was measured by the researcher by looking at the data from the observation sheet and the results of the diagnostic tests that were in the patients’ status. The diagnostic examination data were taken based on the latest date for platelet measurement and liver function. Data of GCS, MAP, and FiO2/PaO2 were measured based on the conditions when the researchers arrived. 24-h urine was taken from the observation of fluid balance measurements at 07.00 WIB on the day of the study. The type of ventilator mode was recorded at the time of the study too. There was also notes about the day of the patients using the ventilator. The duration of using a ventilator was categorized as never use, more than three days use and less than three days. Patients who use less than three days means that the weaning process can be done perfectly. The SOFA score data indicates that the higher the patients’ condition, the more critical and more actions are needed to maintain the condition and to improve the patient's condition.
ResultsThis study examined the relationship between ventilator use and SOFA score in patients who were admitted to the ICU Arifin Achmad Pekanbaru Hospital who were treated for at least two days by 40 respondents.
The majority of respondents using ventilators were in early adulthood (43.8%) and males (52.5%). Most of them were treated less than three days in the ICU. The majority of respondents used ventilators less than two days (55%) with 100% SOFA score of more than 2 with an average of 7.8. Where the mean value of GCS was 8.8; MAP was 88.75; PaO2 was 79.8; and urine output for 24h with a mean of 1332.7ml.
Based on the duration of the ventilator use by 40 respondents, most of them used ventilators for more than two days (48h). There is very significant relationship which means that patients who use ventilators more than 2 days (p<0.001) will be at risk for organ infections that can lead to increasingly severe organ failure. See Table 1 for the data of the relationship of ventilator use and SOFA score.
DiscussionOrgan failure scores in patients at the ICU can help predict the length of stay.1 SOFA scores can be used to predict the prognosis of a patient's critical condition. Score SOFA was designed and developed to objectively evaluate failures in one organ or several organs. Components that are assessed based on SOFA are easy to assess and count to see the patient's condition. Data were measured based on patients’ clinical data and laboratory data.
The results showed that the SOFA score had a relationship with the duration of ventilator use in patients admitted to the ICU. The longer a ventilator is used, the bigger patients have a higher SOFA score. This shows the prognosis to get worse. Based on the results of the research of six components measured, namely respiration, cardiovascular, hematological, renal, liver and neurological functions, high levels of SOFA indigo were found to be a function of respiratory and neurological organs. In respiratory conditions from the average results, it was found that the SOFA score was above two (2.95) because patients possessed PaO2/FiO2 conditions between 100 and 200. This indicates that the oxygen level in the patients’ body is not optimal and can cause other organ dysfunctions. The condition of low PaO2 will cause hypoxia which can subsequently cause vasodilatation of brain blood vessels. This will be followed by an increase in the rate of blood flow to the brain and the result will produce lactic acid and metabolic acidosis. The long reduction in PaO2 will affect on the level of consciousness. The binding of O2 by hemoglobin will also aggravate hypoxia in cerebral and cause the respiratory function to be heavier and the death rate due to severe cerebral hypoxia increases.5
MAP of patients with ventilator was influenced by the position.3 Patients with the highest MAP in semi-fowler position at 15 degree and in this study showed that MAP patients were in normal conditions.4 This means that systemic venous return is normal to heart and tidal volume is not problematic in channeling oxygen carried by hemoglobin and plasma to meet tissue requirements in metabolic processes. Kidney function is still capable of performing its functions and can be seen from the results of research that urine secreted in the kidneys is still in enough limit.
The finding shows that the relationship between SOFA scores and the duration of ventilator use is strongly related (p<0.001). This indicates that patients who have a low SOFA score use a shorter ventilator where the majority of respondents use a ventilator less than 2 days. The patients’ meaning is minimal for infection due to ventilator use or Pneumonia associated Ventilator1 (VAP).
Ventilator Related Pneumonia/Associated Pneumonia Ventilator (VAP) is an inflammation of the lung parenchyma caused by a bacterial infection that incubates when the patient receives mechanical ventilation using a mechanical ventilator. Provision of prolonged mechanical ventilation (more than 48h) is the most important factor causing nosocomial pneumonia. VAP is defined as pneumonia which appears more than 48h after endotracheal intubation and initiation of mechanical ventilation.2 VAP divided into early onset which occurs within the first 96h of mechanical ventilation and late onset that occurs more than 96h after administration of mechanical ventilation.
Mechanical intubation and ventilation can increase the risk of VAP. The use of intubation that is not really needed should be avoided as much as possible. Non-invasive ventilators that use face masks can be used as an alternative in ICU patients who use a ventilator because they have a smaller risk of VAP when compared with invasive ventilator use.2 Several studies have identified the duration of ventilator use as one of the important factors triggering VAP. In patients with mechanical ventilation, the incidence of VAP increases with the length of ventilation and is not constant from time to time using a ventilator.
ConclusionThe majority of respondents using ventilators were in early adulthood (43.8%) and males (52.5%). Most of them were treated less than three days in the ICU. The majority of respondents used ventilators for less than two days (55%) with a 100% SOFA score of more than 2 with an average of 7.8. Data on the relationship between the duration of the use of a ventilator and a SOFA score shows that these two variables have a very significant relationship with p<0.001.
The researchers would like to thank all people who have helped them in the research process. This gratitude especially goes to ICU patients who have participated as respondents of this study and ICU nurses who have been very supportive during data collection. The researchers would also thank Universitas Riau that has provided funding assistance for this research.
Peer-review of abstracts of the articles is under the responsibility of the Scientific Committee of Riau International Nursing Conference 2018. Full-text and the content of it is under responsibility of authors of the article.