The incidence of trauma has been high and is considered to have increased throughout the years. This study aimed to describe the pain intensity and pain-management strategies of hospitalized trauma patients. Ninety-five adults presenting trauma with full consciousness, and who were admitted to surgical wards were recruited. Outcomes were assessed in a 3-day follow-up of pain and pain management from January to February 2016 by using questionnaires for interviews. Data were analyzed using descriptive statistics and repeated measures ANOVA. Preliminary research found that hospitalized trauma patients perceived mild to severe pain intensity. The trend of pain at its worst, pain at its least, average pain, and current pain decreased from Day 1 to day 3, which were statistically and significantly different (p < .001). The pain management often used by patients were: praying (84.2%), slow and deep breathing (78.9%), and at an attempt at toleration (46.3%). The least frequent method of pain management included immediately informing nurses about the pain (15.8%), reading (15.8%), and changing position (17.9%). Besides the pharmacological and nonpharmacological interventions received from physicians and nurses, strategies were crucial to alleviating pain in hospitalized trauma patients related to cultural context.
Apparently, the incidence of trauma has been high and is considered to have increased throughout the years (World Health Organization [WHO]1,2. Hospital admissions were reportedly 2.3 million in the United States and 5.7 million in European countries (Centers for Disease Control and Prevention [CDC]3,4. Most trauma patients were admitted due to motor-vehicle collisions (MVC) or falls2. Likewise, in Indonesia, the incidence of trauma from MVC accounted for close to 1.3 million every year1. This number is indicated that MVC was sitting in the top 10 of leading causes of death.
Previous research in Western countries found a high prevalence of moderate to severe pain in trauma patients during hospitalization. For instance, 80 percent of musculoskeletal injury patients in a study conducted by Rosenbloom perceived moderate to severe pain when they were admitted to a large hospital in Canada5. Similarly, most patients with other types of trauma, such as burns and orthopedics injuries rated the same level of pain6,7. Also, two qualitative studies have interviewed hospitalized trauma patients in westernized cities of Asia8,9. These studies revealed that most trauma patients with orthopedic and burn injuries reported severe pain during hospitalization.
Pain management is essential to eliminate the cause of pain10. Evidence noted that trauma patients might receive pharmacological or nonpharmacological methods (e.g., relaxation, guided imagery, and information about pain)8,11–15. Moreover, patients are able to apply their strategies, such as music, relaxation, or praying16–19. However, the study showed that the nonpharmacological strategy was underutilized20.
Although pain and pain management in hospitalized traumatic patients has been well documented in western countries and Asia (i.e., Hong Kong), the differences of culture, society, and health care system among countries has recognized as one of the influencing factors to how person perceives and reacts to pain experience21. In Indonesia, little research on pain in hospitalized traumatic patients exists. Therefore, a study was needed to examine the issue of the intensity of pain and pain management so as to conduct preliminary estimates of the rates of pain and the types of pain management strategies used by hospitalized trauma patients. Such knowledge will be helpful in providing basic information to healthcare providers to gain an understanding about pain and its management based on patients’ preferences. Consequently, healthcare providers can provide pain management properly based on individual needs as they relate to the Indonesian context.
MethodThis descriptive study analyzed hospitalized trauma patients in the surgical wards of Hasan Sadikin hospital, a teaching hospital in West java, Indonesia. Eligible patients included those admitted to the wards in one day, had a Glasgow Coma Scale score of 15, were at least 18 years old, had sustained trauma to areas of the face, chest, abdomen, pelvis, musculoskeletal structure, or limbs, or had been burned, had no psychiatric disorder, and spoke Indonesian.
After the research ethics committee of the Faculty of Nursing and Hasan Sadikin hospital gave its approval, patients who agreed to participate in the study provided their informed consent. Then the first researcher collected data. On the first day, all patients were interviewed about personal information and asked to rate their pain on a numeric rating scale of the brief pain inventory (BPI).
The Indonesian version of the BPI was used to measure pain intensity. It included four items of pain and assessed pain over past one day: pain at its worst, pain at its least, pain on average, and pain right now. This version showed good reliability by Cronbach's alpha equal to .77. The BPI continued assesses the pain of patients on Day 2 and 3. On the third day, in addition to the assessment of the intensity of pain, patients were asked to complete the pain management questionnaire. This questionnaire was developed by the researcher based on a symptom-management model21 and literature review. It consisted of 11 options for pain. A blank space also provided that allowed patients to describe the strategies that may not have been among the options.
Data were statistically analyzed and described by the descriptive statistic. In addition, for the benefit of the analysis, pain intensity was categorized as mild (BPI, 1-4), moderate (BPI, 5-6), and severe (BPI, 7-10)7.
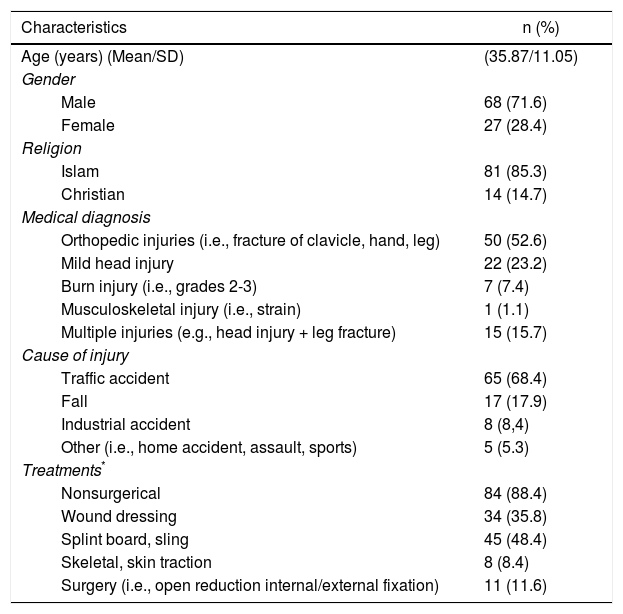
ResultsCharacteristics of the hospitalized trauma patientsA total of 95 hospitalized trauma patients were enrolled in this pilot study. The average of age of the patients was 35.87 (SD=11.05). Most patients were male (71.6%) and Islamic. Half of the patients had orthopedic injuries (52.6%). Most patients received nonsurgical treatments (88.4%) (Table 1).
Patients’ characteristics (n=95).
| Characteristics | n (%) |
|---|---|
| Age (years) (Mean/SD) | (35.87/11.05) |
| Gender | |
| Male | 68 (71.6) |
| Female | 27 (28.4) |
| Religion | |
| Islam | 81 (85.3) |
| Christian | 14 (14.7) |
| Medical diagnosis | |
| Orthopedic injuries (i.e., fracture of clavicle, hand, leg) | 50 (52.6) |
| Mild head injury | 22 (23.2) |
| Burn injury (i.e., grades 2-3) | 7 (7.4) |
| Musculoskeletal injury (i.e., strain) | 1 (1.1) |
| Multiple injuries (e.g., head injury + leg fracture) | 15 (15.7) |
| Cause of injury | |
| Traffic accident | 65 (68.4) |
| Fall | 17 (17.9) |
| Industrial accident | 8 (8,4) |
| Other (i.e., home accident, assault, sports) | 5 (5.3) |
| Treatments* | |
| Nonsurgerical | 84 (88.4) |
| Wound dressing | 34 (35.8) |
| Splint board, sling | 45 (48.4) |
| Skeletal, skin traction | 8 (8.4) |
| Surgery (i.e., open reduction internal/external fixation) | 11 (11.6) |
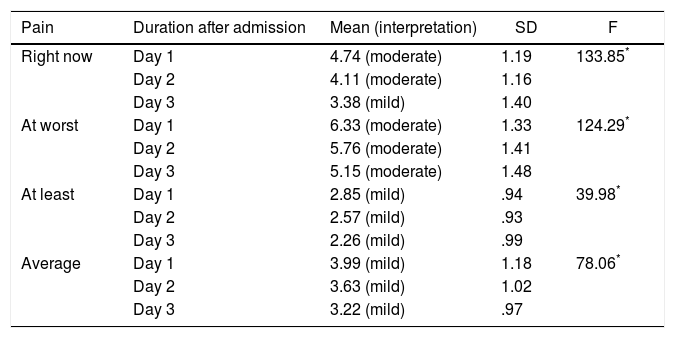
Overall, the pain intensity of hospitalized trauma patients during the first 3 days after admission was at a mild to moderate level. The average pain was 3.99 (SD=1.18) on day 1, 3.63 (SD=1.02) on day 2, and 3.22 (SD=.97) on day 3. Furthermore, the repeated measures ANOVA test revealed statistically significant differences in pain on day 1, day 2, and day 3 after hospital admission (p < .001) (Table 2).
Pain intensity during day 1, day 2, and day 3 after patients were admitted to the hospital (n=95).
| Pain | Duration after admission | Mean (interpretation) | SD | F |
|---|---|---|---|---|
| Right now | Day 1 | 4.74 (moderate) | 1.19 | 133.85* |
| Day 2 | 4.11 (moderate) | 1.16 | ||
| Day 3 | 3.38 (mild) | 1.40 | ||
| At worst | Day 1 | 6.33 (moderate) | 1.33 | 124.29* |
| Day 2 | 5.76 (moderate) | 1.41 | ||
| Day 3 | 5.15 (moderate) | 1.48 | ||
| At least | Day 1 | 2.85 (mild) | .94 | 39.98* |
| Day 2 | 2.57 (mild) | .93 | ||
| Day 3 | 2.26 (mild) | .99 | ||
| Average | Day 1 | 3.99 (mild) | 1.18 | 78.06* |
| Day 2 | 3.63 (mild) | 1.02 | ||
| Day 3 | 3.22 (mild) | .97 |
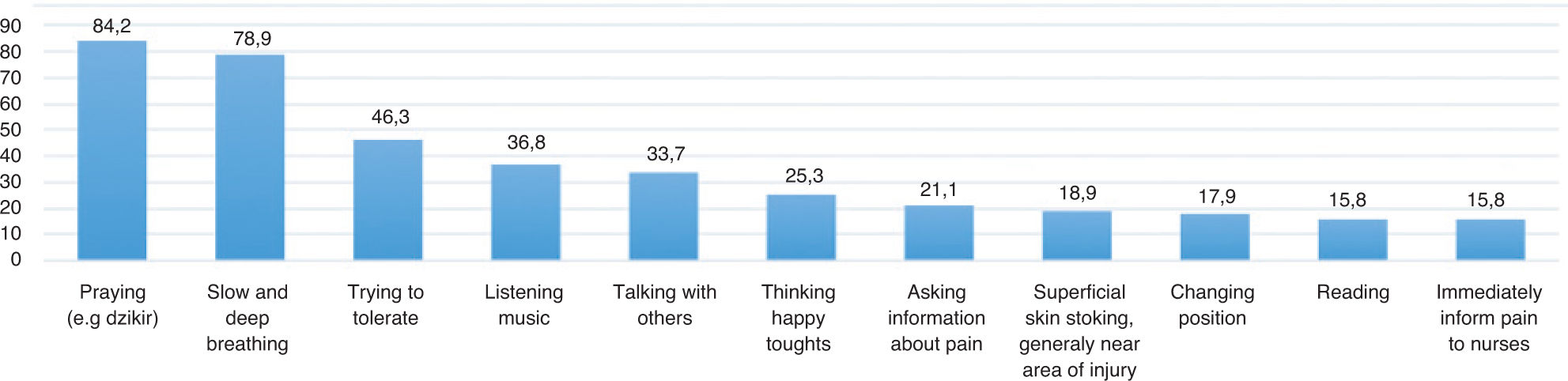
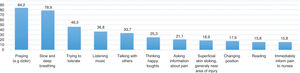
Generally, all patients used the strategies provided in the questionnaire to reduce their pain (Figure 1). Most hospitalized trauma patients frequently used praying (84.2%) as their strategy to reduce pain. This strategy was followed by Slow and Deep Breathing (SDB) (78.9%) and an attempt to tolerate it (46.3%). Meanwhile, other strategies least frequently used by patients included changing position, reading, and immediately telling the nurses about the pain (17.9%, 15.8%, and 15.8%, respectively).
DiscussionThe objective of this study was to provide a pilot description of the rate of the intensity of pain and frequency of pain-management strategies of hospitalized trauma patients. This study found that the intensity of pain of hospitalized trauma patients was at the mild to moderate level. These findings contrasted with those of previous studies in Western countries that found that the intensity of pain was at a moderate to severe level5–7. The result of current find-ing can be explained as follows. The patients in this study had a single injury, which indicated minor-injury level22. Also, patients received several pharmacological pain-management, including paracetamol, ketorolac, tramadol, and fentanyl, which were used to relieve pain effectively. Pa-tients also applied several strategies by themselves.
With respect to patients’ pain-management strategies, most patients in this study reported that they prayed to relieve their pain. This is not surprising because most patients were Muslim. The spiritual aspects are personal concerns that relate to the belief about pain and affect patients’ views on pain management23. Patients in this study noted that the pain and its relief came from God (Allah); therefore, they prayed frequently and recited the name of Allah (Dzikir). Moreover, they noted that hope and asking for help from God could make them calm and relax them. Factoring praying into pain management is important because it can improve patients’ physical and emotional well-being, enhance the immune system, and foster pain relief24. In a cross-sectional study, chronic pain patients found that praying was related to pain tolerance. Patients with a high level of praying had a lower intensity of pain25.
The SDB was in second place. It has been proved to be effective in reducing pain14. Consistent with this finding, trauma patients in this study applied it when they felt pain at its worst. More specifically, orthopedic trauma patients reported that they performed SDB while nurses made up their bed. In addition, almost half the patients tried to bear their pain (trying to tolerate). No patients gave the reason for these strategies. Wong and Chan noted that patients tried to bear and tolerate the pain because of their perception that pain is normal if one is wounded8.
Meanwhile, some pain-management strategies were used by patients the least, such as reading and immediately informing the nurse about pain. Patients were reluctant to report pain intensity to nurses and preferred to endure the pain - this behavior was possibly related to gender and the nature of nursing work.
This study was supported by Thailand's Education Hub for ASEAN Countries (TEH-AC). We thank Graduate School and Faculty of Nursing, Prince of Songkla University, Thailand, Hasan Sadikin general hospital, Indonesia, and all participants of this study.