We present the clinical case report on a 33-year-old woman who, after a perinatal death, presented a complicated grieving process.
The aim was to apply an individualised care plan that enabled reestablishment of the woman’s emotional balance and environment after an experience of perinatal death.
During the first visit to her midwife, the Athens Insomnia, Continuity Bonds and Goldberg Anxiety and Depression scales were applied. Focussed assessment was made using the Gordon patterns and based on the nursing approach described in the Dysfunctional Bereavement Theory.
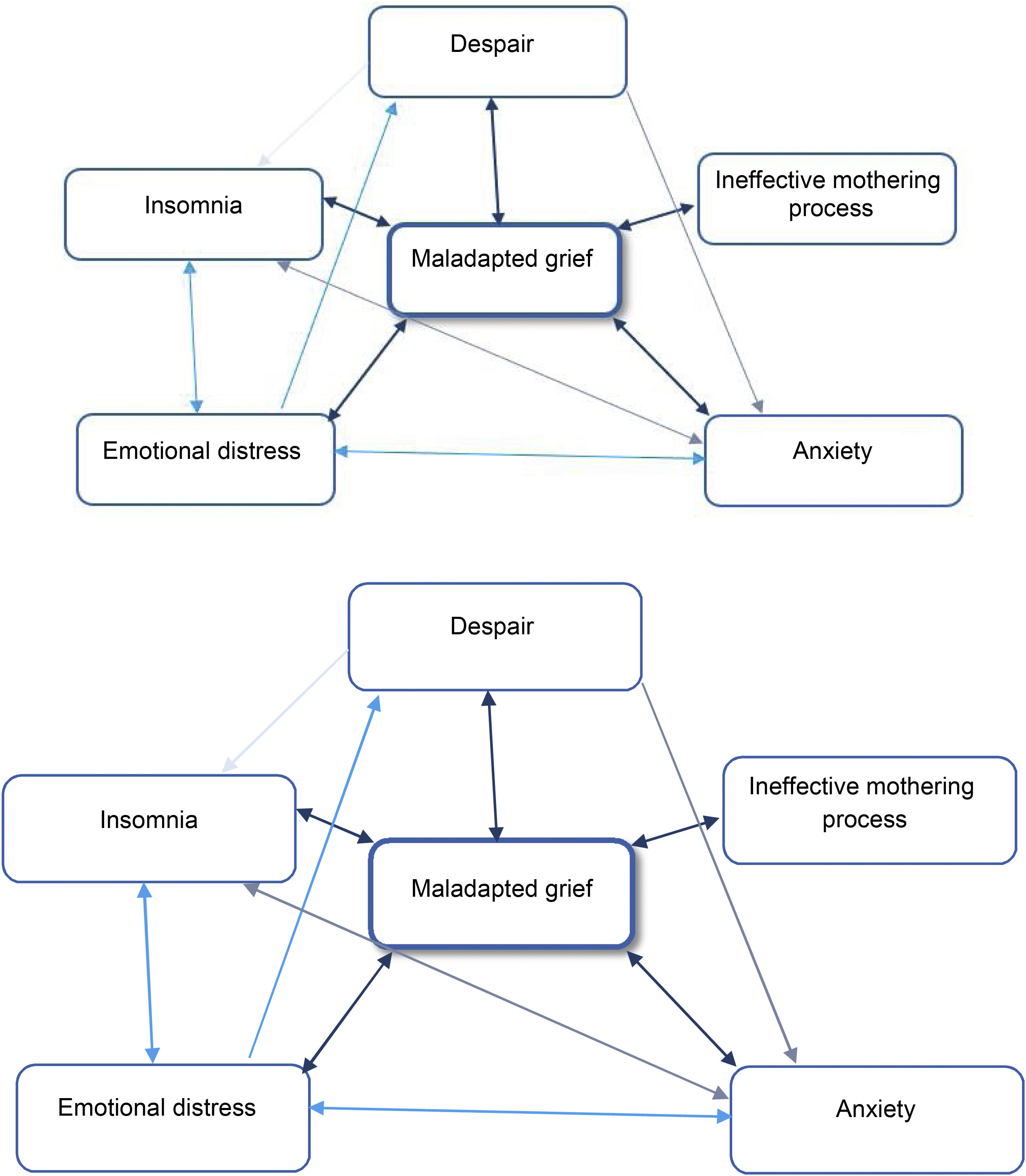
Six International NANDA diagnostic labels were identified (maladaptative grieving, insomnia, hopelessness, ineffective mothering process, moral distress and anxiety), and these were prioritised using clinical network reasoning, using the Outcome Present State Test (OPT) model, observing the relationships between the labels, diagnoses and identifying how they affected the rest.
For each International NANDA diagnostic labels, the nursing outcomes were planned, along with the planned nursing interventions. The expected results included the description of the evaluation indicators using the Likert scales. Both results and interventions were agreed between the professional and the mother.
The care plan raises the difficulty that nursing professionals face when attending to situations of complicated grief, and specifically, those associated with perinatal death. This situation makes key competencies necessary in training, as well as the need to find out about new nursing approaches.
Se presenta el caso clínico de una mujer de 33 años que, tras una muerte perinatal, presenta un proceso de duelo complicado.
El objetivo es aplicar un plan de cuidados individualizado que permita un restablecimiento del equilibrio de la mujer y su entorno tras una vivencia de muerte perinatal.
La valoración se inició durante la primera visita a su matrona en la que se aplicaron las escalas de insomnio de Atenas, de continuidad de vínculos y de ansiedad y depresión de Goldberg. Se realizó una valoración focalizada mediante los patrones de Gordon y desde el enfoque descrito en la Teoría del Duelo Disfuncional.
Se identificaron 6 etiquetas diagnósticas NANDA Internacional (duelo inadaptado, insomnio, desesperanza, proceso de maternidad ineficaz, sufrimiento moral y ansiedad), y se procedió a la priorización utilizando razonamiento clínico en red mediante el modelo Análisis de Resultados del Estado Actual, observando las relaciones entre las etiquetas diagnósticas e identificando cómo incidían sobre el resto.
Para cada una de las etiquetas diagnósticas NANDA Internacional se planificaron los resultados esperados junto con las intervenciones enfermeras planificadas. Los resultados esperados contaron con la descripción de los indicadores de evaluación utilizando las escalas de Likert. Tanto resultados como intervenciones fueron consensuados entre el profesional y la mujer.
El plan de cuidado plantea la dificultad que para los profesionales de enfermería supone la asistencia de situaciones de duelo complicado y concretamente, asociadas a una muerte perinatal. Esta situación hace necesarias competencias clave en la formación, así como la necesidad de conocer nuevos enfoques enfermeros.
The concept of perinatal death is defined as being from the 28th week of gestation to the first 28 days of life (including late foetal death and neonatal death)1,2. In Catalonia, the perinatal mortality rate in 2021 was estimated at 3.59 deaths per thousand live births3. This perinatal loss for the mother and her surrounding environment is associated with a painful process that creates a huge emotional impact that is difficult to manage and which occurs in cases of dysfunctional and/or complicated bereavement.
The normal affective or adaptive response of any person to any loss is known as bereavement and is most often accompanied by specific physical and psychological responses that lessen in intensity over time, as acceptance of the death or loss occurs2,4.
However, in high-impact situations, there are people who experience a deficit in coping that is maintained over the long term, giving rise to what is known as complicated bereavement5. Health professionals have to tackle these situations and actually experience them as failure, along with anxiety due to the heavy emotional burden they experience, presenting responses that range from crying, sadness, pain, anger and even fear5,6.
The Dysfunctional Bereavement Theory, first described by G. Eakes, M. Burke and M. Hainsworth in 1989, is a mid-range nursing theory that provides management approaches that take into account the internal and external triggers of the dysfunctional bereavement process and, in this case, allows for the development of an individualised care plan7.
The aim of the present study was to implement an individualised healthcare plan to restore the equilibrium of this person and her environment after a perinatal death experience.
Description of the caseA 33-year-old mother who, after an uncomplicated multiple pregnancy, in the 38th+6th week of gestation was informed in one of the ultrasound scans run, that one of the two foetuses did not have a heartbeat, sudden death being established as the probable cause. The news was communicated to her by a professional in a darkened room where the rest of the tests were undertaken to complete the study. At that moment, all she could think of were the words of the professional in front of her: "one is there but the other is not". Over the next few hours, further ultrasound scans and preoperative tests confirmed the diagnosis and led to the need for an emergency caesarean section that same day.
Overall assessmentAfter one month, the mother went to see the midwife for a check-up and a nursing assessment was made taking the Dysfunctional Bereavement Theory approach, adopting Marjorie Gordon's Functional Patterns (FP)8, in order to be able to structure and analyse the narrative obtained during that first visit and the following two planned visits (with a 1-month separation between them). The first session was recorded with the mother's consent, in order to go deeper into the analysis of the discourse she presented, and the content was subsequently transcribed and validated by the mother herself.
During the first scheduled visit, different self-administered scales were applied. Sleep was assessed using the Athens Insomnia Scale in its reduced version9, obtaining an initial value of 11/15 (taking into account that each item responds to a Likert-type scale in which 0 corresponds to "not a problem" and 3 to a "major problem", considering 6 as the cut-off point for the consideration of chronic insomnia). The bond with the deceased son was assessed using the bond continuity scale (ECoVin in its Spanish acronym)10, with a value of 35/64 (where higher scores denote greater strength in the continuity of the bond with the deceased son, with 16 points being the minimum score and 64 points the maximum). The degree of anxiety was screened using the Goldberg Anxiety and Depression Scale (EAD-G)11, with a value of 5/9 (with three of the items being affirmative for anxiety and the remaining two for depression). As cut-off points, this last scale presents 4 or more affirmative answers for the anxiety subscale, and 2 or more for the depression subscale.
The focussed assessment relating to each of the functional patterns was structured taking into account the experience of the loss, the discrepancies between what was expected and what was actually experienced, and the coping methods, as described in the Dysfunctional Bereavement Theory.
The experience of lossAccording to the health perception management pattern, the mother stated that, after receiving the fateful news, she experienced the worst possible feeling that any human being could ever have during their life. She told us that at that time her health was not good, as she felt that "…one part of me had died while the other part was kept alive by [her other son]".
She was aware, thanks to family support systems, that she did not present any kind of deficit in her nutritional pattern. It was her mother who encouraged her to eat in order not to skip any of the daily meals. This is described within the role-relationship pattern.
She had seen her sleep-rest pattern altered by the difficulty she had with long and "bad" nights. She compensated for the immense emotional pain "with armour that has nullified me as a person". She admitted that she had not been oriented in time and place for a long time, as if the world had stopped.
She stated that it was painful not to have seen her son's face, as she did not want to do so in those first moments, "I will always regret it", she said. With regard to the cognitive-perceptual pattern, she had reflected on this situation, and considered that it would have been important to her, as a result of the possibility of saying goodbye. Her partner did do this and considered that it had been positive for him.
She verbalised guilt in terms of the pattern of self-perception: "What have I done wrong for this to have happened", were the phrases that were repeated in her dialogue, together with the crying that accompanied her throughout those months. She stated that she felt a sadness that she did not think she would be able ever to get rid of until she met her little boy "in heaven". She felt dead in life, considering that "one part of me has died while the other is kept alive by [her other son]".
She said that her relationship with her partner had been affected by the loss and, especially, because they did not think about becoming parents again. She considered that fear had been key because of the fear of going through the same situation again.
The arrival home after the birth was stressful, considering the pattern of adaptation-stress tolerance. On entering her home, she felt lost. She had left "fine" but arrived back devastated.
Discrepancies between what was expected and what was experiencedThe mother's discourse expressed discrepancies between what she imagined she would experience and what this turned out to be. She expressed this as "you never imagine that it will happen to you".
The communication of the news by the professional who attended her, in her view, was not the most appropriate at that moment, due to the lack of any intimacy, empathy or warmth, which were lacking in that professional, and which influenced her ability to resist the changes to which she was subjected; all of this defined within the pattern of adaptation-tolerance to stress.
This situation was compounded by the lack of information that they were given as a couple, making it difficult for them to be conscious of and manage their own health. She says that they did not know what steps to take; what they had to do administratively; what emotional support they could count on and, most difficult of all; how they should proceed to bury their deceased son. She recalled how painful it was when she received a call to tell her that they had to collect her son's body. Added to this was the lack of any administrative recognition that her son had received. He had been a fully-fledged unborn child, but since he was stillborn, he would not be recorded anywhere.
She considered herself lucky to have had her partner by her side, helping her to move forward.
She acknowledged that each anniversary presented her with a dichotomy; the happiness of celebrating one more year of her son’s life but also the memory of the loss of her other son. She told us that a small bouquet of flowers accompanied them every year.
Management methodsIn this situation and, as mechanisms for managing the pattern of perception management of health, the mother, on an internal level, clung to her inner strength; to the introversion that the moments of isolation allowed her; and to her own feelings of anger and bereavement. But she recognised that what helped her most was her own son. This helped her to get up every morning and be strong enough to move forward. Her son was the most important thing at that time; this need for care made the days shorter and her mind had no time for bereavement.
External mechanisms involved moments of crying, locked in her bedroom, expressing the pain that was crushing her chest. The possibility of verbalising and expressing those feelings was centred on one figure, her partner.
She admitted that when she got angry with herself, she thought about what she would say to other mothers in the same situation: "you get so angry, […]… every day that goes by you get angrier, but the pain gets gradually lighter […] otherwise we wouldn't be able to live".
As a result of the nursing assessment, 6 NANDA International diagnostic labels (NANDA-I) were identified, which considered the presence of at least two defining characteristics or risk factors, as proposed by Herdman in 202112. The diagnoses identified were: maladaptive bereavement, insomnia, hopelessness, an ineffective mothering process, emotional distress and anxiety.
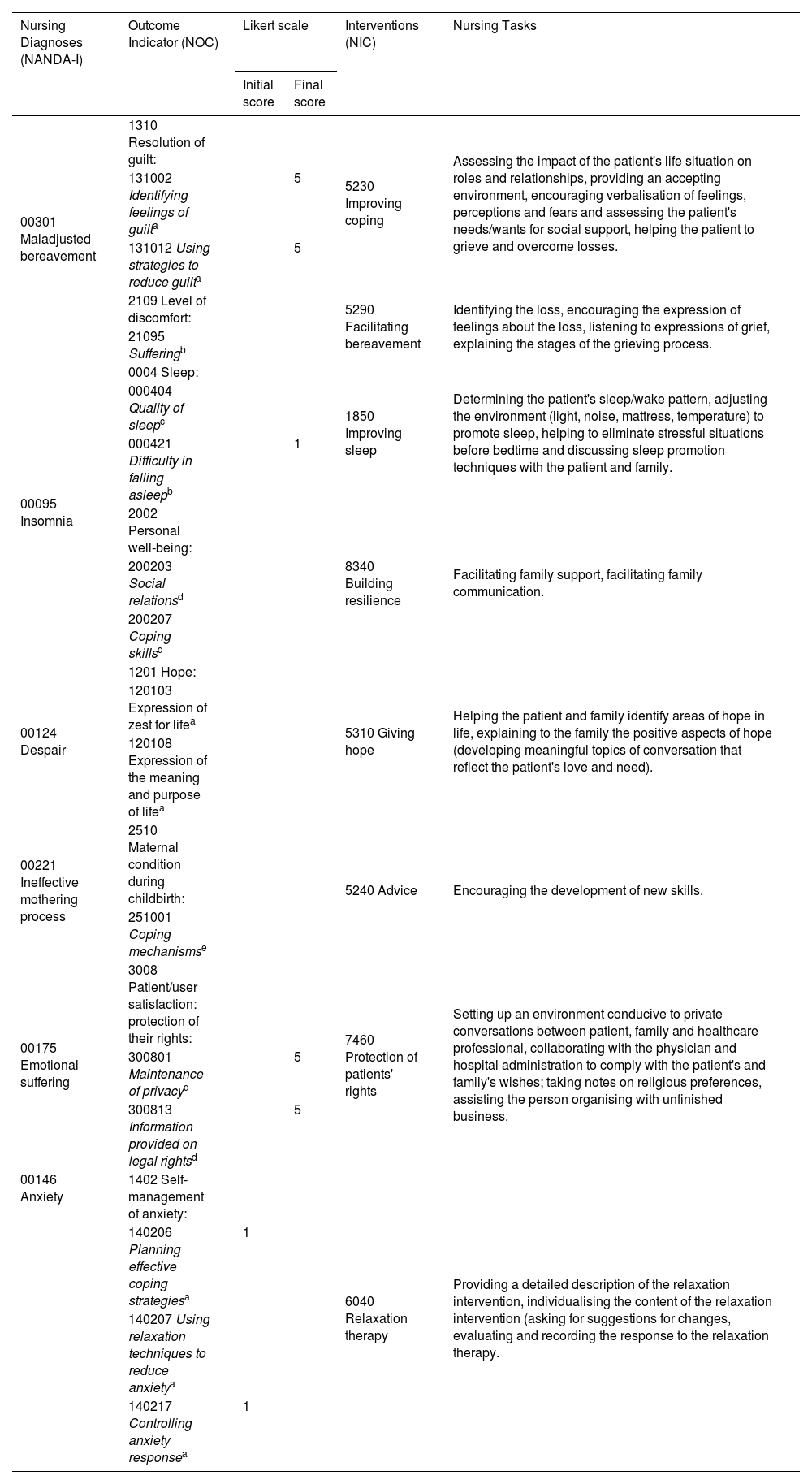
Care planning and implementationBased on the diagnostic labels identified, a care plan was devised, setting out the expected results and the interventions undertaken, following the taxonomy of expected outcomes (NOC: Nursing Outcomes Classification) and nursing interventions (NIC). These were included in the patient’s individualised care plan, using the NNNConsult online platform and determining the quantitative value for each of the outcomes indicators, according to a 5-point Likert-type scale, on a continuum of least to most desirable, and providing a score at the time of assessment.
For the prioritisation, the Analysis of the Current Status of Results (AREA in its Spanish acronym) model was used as a tool for network-based reflective and critical reasoning. This analysis enabled the main problem to be identified, taking into account the actual situation of the mother and her environment (Fig. 1)13,14. This network prioritisation was undertaken by the midwife, establishing the relationships between the different diagnostic labels and observing which one had the greatest impact on the rest. In this case, the main problem identified was maladaptive bereavement after the death of a significant person for the patient.
Assessment of results/monitoringFollow-up on the expected outcomes was undertaken throughout the three scheduled visits, showing consistency between the real problem identified and the expected results for each of the indicators used. Bearing in mind that the diagnostic label of maladaptive bereavement was shown to be a priority in the design of the care plan, it was necessary to identify feelings of guilt as indicators; the use of strategies to reduce this; and the assessment of suffering, with results that denoted a positive evolution reaching the maximum value on the Likert scales, through interventions aimed at improving coping and facilitating bereavement (see Table 1).
Individualised care plan.
| Nursing Diagnoses (NANDA-I) | Outcome Indicator (NOC) | Likert scale | Interventions (NIC) | Nursing Tasks | |
|---|---|---|---|---|---|
| Initial score | Final score | ||||
| 00301 Maladjusted bereavement | 1310 Resolution of guilt: | 5230 Improving coping | Assessing the impact of the patient's life situation on roles and relationships, providing an accepting environment, encouraging verbalisation of feelings, perceptions and fears and assessing the patient's needs/wants for social support, helping the patient to grieve and overcome losses. | ||
| 131002 Identifying feelings of guilta | 5 | ||||
| 131012 Using strategies to reduce guilta | 5 | ||||
| 2109 Level of discomfort: | 5290 Facilitating bereavement | Identifying the loss, encouraging the expression of feelings about the loss, listening to expressions of grief, explaining the stages of the grieving process. | |||
| 21095 Sufferingb | |||||
| 00095 Insomnia | 0004 Sleep: | 1850 Improving sleep | Determining the patient's sleep/wake pattern, adjusting the environment (light, noise, mattress, temperature) to promote sleep, helping to eliminate stressful situations before bedtime and discussing sleep promotion techniques with the patient and family. | ||
| 000404 Quality of sleepc | |||||
| 000421 Difficulty in falling asleepb | 1 | ||||
| 2002 Personal well-being: | 8340 Building resilience | Facilitating family support, facilitating family communication. | |||
| 200203 Social relationsd | |||||
| 200207 Coping skillsd | |||||
| 00124 Despair | 1201 Hope: | 5310 Giving hope | Helping the patient and family identify areas of hope in life, explaining to the family the positive aspects of hope (developing meaningful topics of conversation that reflect the patient's love and need). | ||
| 120103 Expression of zest for lifea | |||||
| 120108 Expression of the meaning and purpose of lifea | |||||
| 00221 Ineffective mothering process | 2510 Maternal condition during childbirth: | 5240 Advice | Encouraging the development of new skills. | ||
| 251001 Coping mechanismse | |||||
| 00175 Emotional suffering | 3008 Patient/user satisfaction: protection of their rights: | 7460 Protection of patients' rights | Setting up an environment conducive to private conversations between patient, family and healthcare professional, collaborating with the physician and hospital administration to comply with the patient's and family's wishes; taking notes on religious preferences, assisting the person organising with unfinished business. | ||
| 300801 Maintenance of privacyd | 5 | ||||
| 300813 Information provided on legal rightsd | 5 | ||||
| 00146 Anxiety | 1402 Self-management of anxiety: | 6040 Relaxation therapy | Providing a detailed description of the relaxation intervention, individualising the content of the relaxation intervention (asking for suggestions for changes, evaluating and recording the response to the relaxation therapy. | ||
| 140206 Planning effective coping strategiesa | 1 | ||||
| 140207 Using relaxation techniques to reduce anxietya | |||||
| 140217 Controlling anxiety responsea | 1 | ||||
NOC: Nursing Outcomes Classification; NIC: Nursing Interventions Classification.
Qualitative value of Likert scales.
1 (Never displayed), 2 (Rarely displayed), 3 (Sometimes displayed), 4 (Frequently displayed), 5 (Always displayed).
1 (Severely compromised), 2 (Substantially compromised), 3 (Moderately compromised9, 4 (Slightly compromised), 5 (Not compromised).
During the implementation of the interventions, it was essential to involve the partner in order to go deeper into achievement of the objectives and to consider this as one of the key elements for their success.
After the planned visits, the degree of insomnia was re-assessed with a significant improvement of 4 out of 15 on the Athens scale9. The ECoVin scale10 also showed a decrease, down to a weighting of 20, with an improvement in terms of emotional attachment to the deceased son. And in terms of anxiety-depression, there was an improvement to a value of 3 (two affirmative items for anxiety and one for depression). Both the mother herself and the couple were satisfied with the follow-up. undertaken by the professional and with the positive evolution they were obtaining. From the perspective that those months gave her, she told us that the pain had eased.
Discussion/Implications for clinical practiceThe grieving process, as a natural and self-limiting process of adaptation of the person, in highly stressful situations and, where this is associated with a lack of coping skills on the part of the subject, can lead to dysfunctional bereavement. This situation has major implications for professionals, adequate identification and an early diagnosis being necessary in order to plan care that would provide the person with the tools for effective coping2,5.
The recognition by professionals of the existence of risk factors that involve women16 (family, environment, support network), is a first step towards not ignoring these situations, which in many cases are silenced due to the serious emotional implications that they entail.
It was therefore of particular interest for the midwife to be able to identify the triggers or inputs that the mother received, both positive and negative, throughout the situation experienced. In the mother's discourse, the lack of knowledge in the hospital environment of how to communicate these events stood out. In her case, she expressed this as one of the most negative approaches. She considered that the lack of preparation of professionals to deal with situations of loss could be one of the causes. Nobody expected to get through a situation like this unscathed: "you are left in shock", but if the accompaniment is adequate, the mourning process may not become dysfunctional. This misinformation manifested by the mother influenced the altered outcome of the perception management pattern of her health.
On a positive note, the mother highlighted the nurses’ affection, empathy and silence accompanied by those looks that denoted sensitivity and that relieved the pain of those moments and that were provided by those nurses at the hospital.
The mother said that the closeness and accompaniment provided by the nurses at the centre had been key. She considered that, although the nurses may have lacked the skills to cope with such a situation of loss, they compensated for it with their empathy, sensitivity and ability to be warm.
The ability of nurses (including midwives in this concept) to reflect on their communication skills and relief of emotional pain was a step towards recognising the need to further work on the skills of a helping relationship, and this is a key element in understanding the role of nurses from this viewpoint within the Theory of Dysfunctional Bereavement2.
The use of intermediate nursing theories brings theorisation of the nursing discipline itself closer to actual clinical practice, especially taking into account the lack of knowledge of these approaches that enable the provision of excellent care and improve its quality6.
Among the main limitations of the care plan, it should be noted that perinatal bereavement continues to be a taboo subject in society and among professionals themselves — and is associated with under-recording due to a lack of knowledge of how to detect this. As a strength, we would highlight the fact that we have been able to bring visibility to this situation through a very personal account, highlighting essential elements for the quality care of those affected.
The development of a care plan for the management of complicated bereavement, planned jointly with the mother, led to results that responded to the problems identified. The sessions planned jointly between the midwife and the mother have been described by the latter as liberating, as a result of the feeling of being listened to.
Therefore, through this clinical case, it can be seen that the use of a middle-range theory by nurses, with a focus on maladaptive bereavement in highly stressful situations, would make it possible to focus on aspects of daily clinical practice that would not be possible to address from a different, more globalised and macro point of view.
FundingThis work has not received any funding.
Conflict of interestThe authors have no conflict of interest to declare.
We would like to thank the mother who has allowed her experience of perinatal bereavement to be made visible in this article. The story was recorded, transcribed and validated by her afterwards. The phrases or words in quotation marks and in italics correspond to part of the story.