Losing a newborn is for many mothers a painful end in which death occurs when life is expected, which makes them live a time of loneliness, personal doubt and feeling of failure. After carrying out a previous qualitative study analyzing the experiences of 25 women who suffered a spontaneous perinatal loss at any time during pregnancy and a systematic review of the factors that affect the emotional response after perinatal losses, a nursing care proposal is presented based on Watson’s Theory of Transpersonal Human Care to respond to the needs of women who experience this loss process. This care plan proposal is intended to achieve individualized care for women who suffer perinatal losses adapted to their needs, not only physical but also emotional.
Perder a un recién nacido es para muchas madres un final doloroso en el que acontece la muerte cuando se espera la vida, que les hace vivir un tiempo de soledad, duda personal y sentimiento de fracaso. Tras realizar un estudio cualitativo previo analizando las vivencias de 25 mujeres que sufrieron una pérdida perinatal espontánea en cualquier momento del embarazo y una revisión sistemática de los factores que afectan a la respuesta emocional tras las pérdidas perinatales, se presenta una propuesta de cuidados de enfermería basado en la Teoría del Cuidado Humano Transpersonal de Jean Watson para dar respuesta a las necesidades de las mujeres que experimentan dicho proceso de pérdida. Con esta propuesta de plan cuidados, se pretende conseguir un cuidado individualizado a las mujeres que sufren pérdidas perinatales adaptado a sus necesidades, no sólo físicas sino también emocionales.
Perinatal loss affects women in many different ways, transforming them physically, psychologically and socially.1 Nurses lack training for offering support during perinatal grief,2,3 although the use of intermediate-range theories brings the theory of discipline closer to clinical practice, promoting excellence in care and thus improving care quality. The Transpersonal4 care theory invites us to develop a concern for understanding human behaviour from the patient’s own frame of reference, providing care centred on the culture, values, and beliefs of people through the transpersonal nurse/patient relationship.5,6 Watson understands that the domain of nursing is the application of care for the maintenance or recovery of health, as well as support in the end-of-life process and moment of death.5 The transpersonal relationship seeks to protect, to enhance and preserve the dignity, humanity, integrity and inner harmony of both the person receiving care and the person giving it, and can be influenced by the moment of care through the choices and actions decided in the relationship.4–6 According to Watson the nurse must cultivate “Caring”, which means caring by healing. To do this, in the inter-relationship with the patient, the nurse must help him or her adopt health-seeking behaviours, using other care supportive elements such as: silence, singing, music, touching, “being present” through art, non-verbal expressions, statements full of spirituality and energy that lead to peacefulness and healing.4–6 It is based on the harmony between mind, body and soul, through the helpful, trusting relationship between the cared for person and the caregiver.4,5 After carrying out an integrative review of the factors that affect women experiencing perinatal loss and conducting research that collected the needs of 25 women who suffered perinatal loss at different times during pregnancy,7,8 we drew up a proposal for a Care Plan for these women based on Watson’s Transpersonal Care Theory.
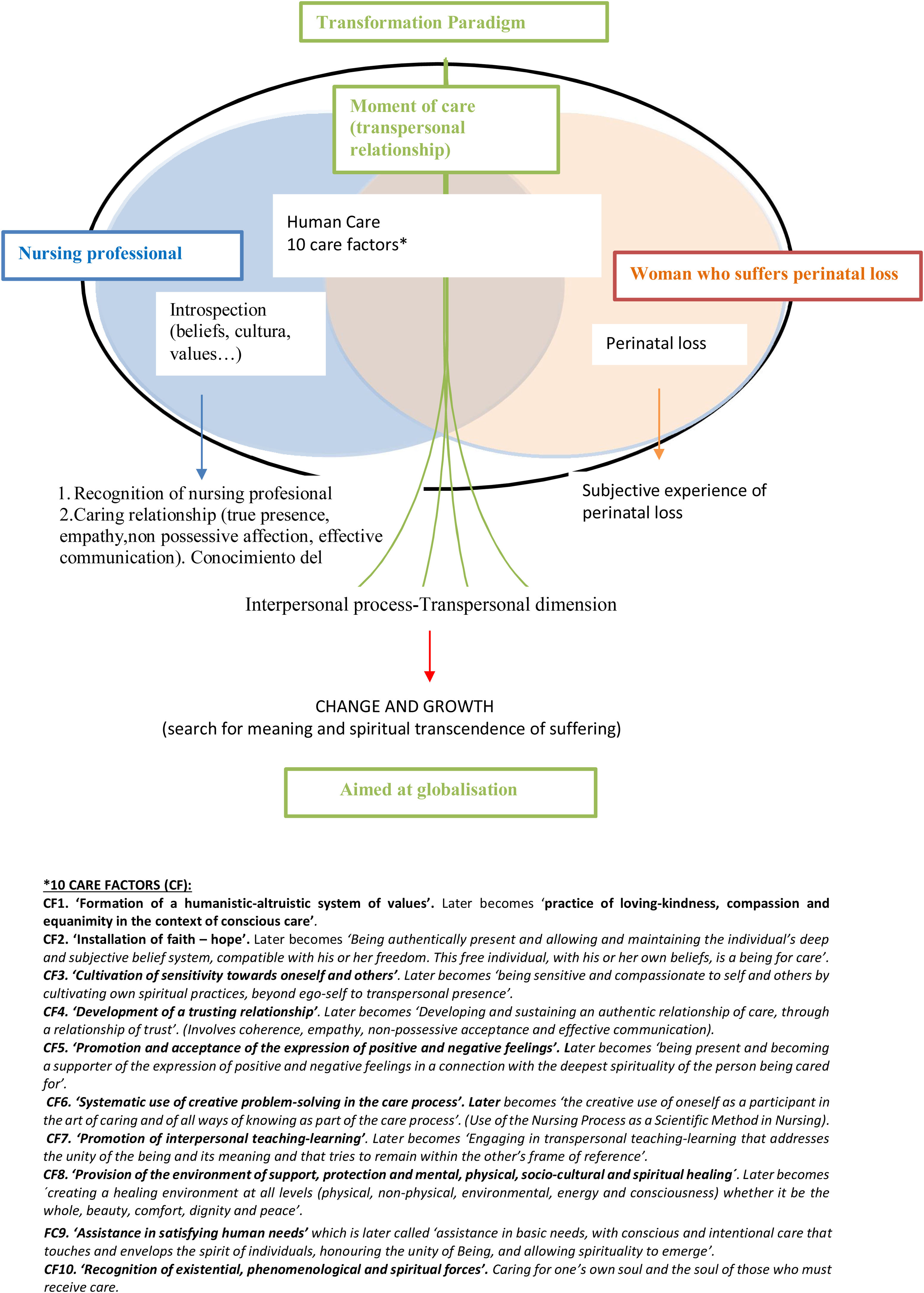
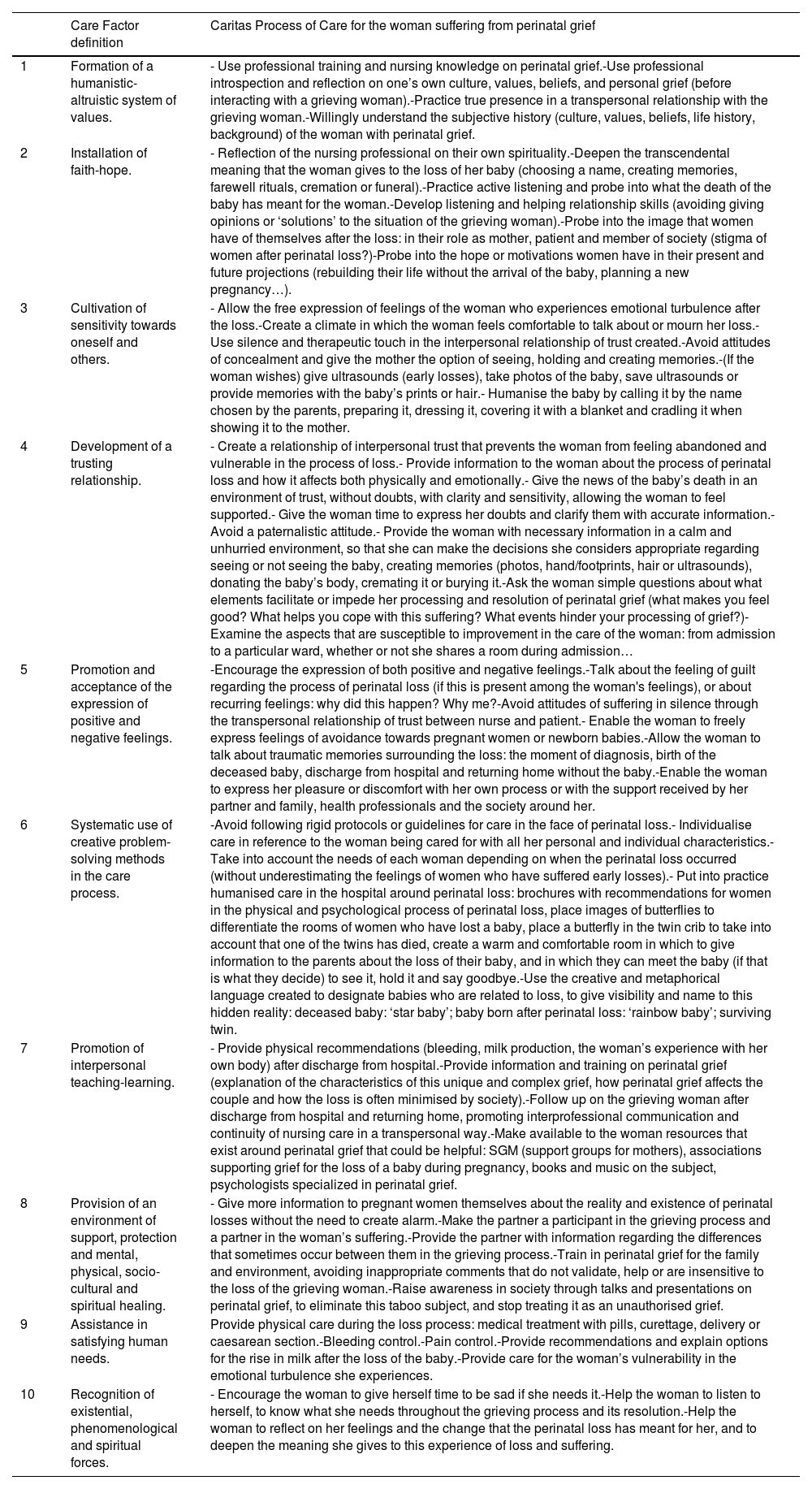
DevelopmentWatson’s theory was divided into ten care factors (CF), which were later modified to develop the “caritas" care processes (CCP), with a clearly spiritual dimension and aimed at transpersonal care. From these 10 care factors and the recommendations and improvements in care proposed by women who suffered a perinatal loss,3 a Care Plan was proposed based on Watson's Transpersonal Theory with the 10 caritas care processes adapted to the care of women in perinatal grief (Fig. 1 and Table 1).
Theory of Human Care by Jean Watson adapted to the care of women who suffer perinatal losses.
*10 CARE FACTORS (CF):
CF1. ‘Formation of a humanistic-altruistic system of values’. Later becomes ‘practice of loving-kindness, compassion and equanimity in the context of conscious care’.
CF2. ‘Installation of faith – hope’. Later becomes ‘Being authentically present and allowing and maintaining the individual’s deep and subjective belief system, compatible with his or her freedom. This free individual, with his or her own beliefs, is a being for care’.
CF3. ‘Cultivation of sensitivity towards oneself and others’. Later becomes ‘being sensitive and compassionate to self and others by cultivating own spiritual practices, beyond ego-self to transpersonal presence’.
CF4. ‘Development of a trusting relationship’. Later becomes ‘Developing and sustaining an authentic relationship of care, through a relationship of trust’. (Involves coherence, empathy, non-possessive acceptance and effective communication).
CF5. ‘Promotion and acceptance of the expression of positive and negative feelings’.Later becomes ‘being present and becoming a supporter of the expression of positive and negative feelings in a connection with the deepest spirituality of the person being cared for’.
CF6. ‘Systematic use of creative problem-solving in the care process’.Later becomes ‘the creative use of oneself as a participant in the art of caring and of all ways of knowing as part of the care process’. (Use of the Nursing Process as a Scientific Method in Nursing).
CF7. ‘Promotion of interpersonal teaching-learning’. Later becomes ‘Engaging in transpersonal teaching-learning that addresses the unity of the being and its meaning and that tries to remain within the other’s frame of reference’.
CF8. ‘Provision of the environment of support, protection and mental, physical, socio-cultural and spiritual healing’. Later becomes ‘creating a healing environment at all levels (physical, non-physical, environmental, energy and consciousness) whether it be the whole, beauty, comfort, dignity and peace’.
FC9. ‘Assistance in satisfying human needs’which is later called ‘assistance in basic needs, with conscious and intentional care that touches and envelops the spirit of individuals, honouring the unity of Being, and allowing spirituality to emerge’.
CF10. ‘Recognition of existential, phenomenological and spiritual forces’.Caring for one’s own soul and the soul of those who must receive care.
Human Caring proposal supported by Jean Watson’s theory for women who suffer from a perinatal loss.
| Care Factor definition | Caritas Process of Care for the woman suffering from perinatal grief | |
|---|---|---|
| 1 | Formation of a humanistic-altruistic system of values. | - Use professional training and nursing knowledge on perinatal grief.-Use professional introspection and reflection on one’s own culture, values, beliefs, and personal grief (before interacting with a grieving woman).-Practice true presence in a transpersonal relationship with the grieving woman.-Willingly understand the subjective history (culture, values, beliefs, life history, background) of the woman with perinatal grief. |
| 2 | Installation of faith-hope. | - Reflection of the nursing professional on their own spirituality.-Deepen the transcendental meaning that the woman gives to the loss of her baby (choosing a name, creating memories, farewell rituals, cremation or funeral).-Practice active listening and probe into what the death of the baby has meant for the woman.-Develop listening and helping relationship skills (avoiding giving opinions or ‘solutions’ to the situation of the grieving woman).-Probe into the image that women have of themselves after the loss: in their role as mother, patient and member of society (stigma of women after perinatal loss?)-Probe into the hope or motivations women have in their present and future projections (rebuilding their life without the arrival of the baby, planning a new pregnancy…). |
| 3 | Cultivation of sensitivity towards oneself and others. | - Allow the free expression of feelings of the woman who experiences emotional turbulence after the loss.-Create a climate in which the woman feels comfortable to talk about or mourn her loss.-Use silence and therapeutic touch in the interpersonal relationship of trust created.-Avoid attitudes of concealment and give the mother the option of seeing, holding and creating memories.-(If the woman wishes) give ultrasounds (early losses), take photos of the baby, save ultrasounds or provide memories with the baby’s prints or hair.- Humanise the baby by calling it by the name chosen by the parents, preparing it, dressing it, covering it with a blanket and cradling it when showing it to the mother. |
| 4 | Development of a trusting relationship. | - Create a relationship of interpersonal trust that prevents the woman from feeling abandoned and vulnerable in the process of loss.- Provide information to the woman about the process of perinatal loss and how it affects both physically and emotionally.- Give the news of the baby’s death in an environment of trust, without doubts, with clarity and sensitivity, allowing the woman to feel supported.- Give the woman time to express her doubts and clarify them with accurate information.- Avoid a paternalistic attitude.- Provide the woman with necessary information in a calm and unhurried environment, so that she can make the decisions she considers appropriate regarding seeing or not seeing the baby, creating memories (photos, hand/footprints, hair or ultrasounds), donating the baby’s body, cremating it or burying it.-Ask the woman simple questions about what elements facilitate or impede her processing and resolution of perinatal grief (what makes you feel good? What helps you cope with this suffering? What events hinder your processing of grief?)-Examine the aspects that are susceptible to improvement in the care of the woman: from admission to a particular ward, whether or not she shares a room during admission… |
| 5 | Promotion and acceptance of the expression of positive and negative feelings. | -Encourage the expression of both positive and negative feelings.-Talk about the feeling of guilt regarding the process of perinatal loss (if this is present among the woman's feelings), or about recurring feelings: why did this happen? Why me?-Avoid attitudes of suffering in silence through the transpersonal relationship of trust between nurse and patient.- Enable the woman to freely express feelings of avoidance towards pregnant women or newborn babies.-Allow the woman to talk about traumatic memories surrounding the loss: the moment of diagnosis, birth of the deceased baby, discharge from hospital and returning home without the baby.-Enable the woman to express her pleasure or discomfort with her own process or with the support received by her partner and family, health professionals and the society around her. |
| 6 | Systematic use of creative problem-solving methods in the care process. | -Avoid following rigid protocols or guidelines for care in the face of perinatal loss.- Individualise care in reference to the woman being cared for with all her personal and individual characteristics.- Take into account the needs of each woman depending on when the perinatal loss occurred (without underestimating the feelings of women who have suffered early losses).- Put into practice humanised care in the hospital around perinatal loss: brochures with recommendations for women in the physical and psychological process of perinatal loss, place images of butterflies to differentiate the rooms of women who have lost a baby, place a butterfly in the twin crib to take into account that one of the twins has died, create a warm and comfortable room in which to give information to the parents about the loss of their baby, and in which they can meet the baby (if that is what they decide) to see it, hold it and say goodbye.-Use the creative and metaphorical language created to designate babies who are related to loss, to give visibility and name to this hidden reality: deceased baby: ‘star baby’; baby born after perinatal loss: ‘rainbow baby’; surviving twin. |
| 7 | Promotion of interpersonal teaching-learning. | - Provide physical recommendations (bleeding, milk production, the woman’s experience with her own body) after discharge from hospital.-Provide information and training on perinatal grief (explanation of the characteristics of this unique and complex grief, how perinatal grief affects the couple and how the loss is often minimised by society).-Follow up on the grieving woman after discharge from hospital and returning home, promoting interprofessional communication and continuity of nursing care in a transpersonal way.-Make available to the woman resources that exist around perinatal grief that could be helpful: SGM (support groups for mothers), associations supporting grief for the loss of a baby during pregnancy, books and music on the subject, psychologists specialized in perinatal grief. |
| 8 | Provision of an environment of support, protection and mental, physical, socio-cultural and spiritual healing. | - Give more information to pregnant women themselves about the reality and existence of perinatal losses without the need to create alarm.-Make the partner a participant in the grieving process and a partner in the woman’s suffering.-Provide the partner with information regarding the differences that sometimes occur between them in the grieving process.-Train in perinatal grief for the family and environment, avoiding inappropriate comments that do not validate, help or are insensitive to the loss of the grieving woman.-Raise awareness in society through talks and presentations on perinatal grief, to eliminate this taboo subject, and stop treating it as an unauthorised grief. |
| 9 | Assistance in satisfying human needs. | Provide physical care during the loss process: medical treatment with pills, curettage, delivery or caesarean section.-Bleeding control.-Pain control.-Provide recommendations and explain options for the rise in milk after the loss of the baby.-Provide care for the woman’s vulnerability in the emotional turbulence she experiences. |
| 10 | Recognition of existential, phenomenological and spiritual forces. | - Encourage the woman to give herself time to be sad if she needs it.-Help the woman to listen to herself, to know what she needs throughout the grieving process and its resolution.-Help the woman to reflect on her feelings and the change that the perinatal loss has meant for her, and to deepen the meaning she gives to this experience of loss and suffering. |
CCP1: A trusting, secure atmosphere must be established between the woman who has suffered the loss of her child and the professional who will provide care. A nurse who can be introspective and willing to understand the singular, subjective history of the woman who has suffered the loss, and who is able to understand other systems of values, race, social class and generations, will be in a position to provide humanised care. To understand the woman in perinatal mourning, it is essential to know her life history and what her child meant to her.
CF2. Installation of faith – hopeCCP2: Perinatal loss leads women to reflect on their existence, their transcendence and the role they play in society. Spirituality is an innate component of human beings that allows them to seek meaning in life by questioning their origins and identity, which strengthens their ability to adapt to different life situations.4 The nursing relationship of help aims to achieve acceptable emotional stability and to recover hope to continue living as a mourner in order to reposition themselves in life in a different way. If it is not possible to change a painful situation, nurses can always encourage women to adopt the attitude they need to face this suffering.
CF3. Cultivation of sensitivity towards oneself and othersCCP3: Perinatal loss causes emotional turbulence in women that destabilises and breaks down their emotional balance. They must therefore be allowed to express their feelings and be helped to understand and accept them. In the transpersonal nurse-patient relationship, we seek to create a climate in which the woman feels comfortable talking about her child and mourning their loss, developing the ability to listen and truly be present, and humanising the deceased child by offering the mother the chance to see them, hold them, and create memories such as photos or hand/footprints.
CF4. Development of a trusting relationshipCCP4: To create a transpersonal relationship between a nurse and a woman in perinatal grief, an individual relationship is recommended. This allows both people to get to know each other in all aspects of being human, avoiding paternalistic attitudes and providing information to the woman about the process of loss to make her feel less vulnerable and more secure. Nurses should provide information and decision options in a calm environment, answering questions without rushing. As care professionals, they need to understand what elements facilitate or hinder the woman’s processing of perinatal grief.
CF5. Promotion and acceptance of the expression of positive and negative feelingsCCP5: Through this process, the woman who has suffered perinatal loss is expected to express what she finds positive or negative or what she does not agree with. To do this, nurses must encourage the woman to feel free to express the disordered feelings that her loss brings about. Some of the feelings expressed may be guilt, avoidance and traumatic memories around situations of perinatal loss.
CF6. Systematic use of creative problem-solving in the care processPCC6: Here, care can be supported by the Nursing Care Process, as this helps nurses to think critically, reflectively and creatively. Nurses can also review the guidelines and protocols in cases of perinatal loss. However, it is their responsibility to ensure that this care is not systematised, using creativity to humanise care in these losses.
CF7. Promotion of interpersonal teaching-learningPCC7: The goal here is to achieve a collaborative relationship for the woman in her own care process, providing her with recommendations upon hospital discharge from a holistic, individualised care package viewpoint. Furthermore, it is important to encourage this human care to continue at an inter-professional level, ensuring that the woman is monitored in her grieving process. It is important to talk to the woman about the fact that in some cases the socialisation to which we are subjected is the reason why the family and the partner assimilate roles of strength and integrity shortly after the loss, which far from helping the woman who has suffered a perinatal loss to accept the situation, prevent or hinder it. The death of a family member constitutes a highly important change that affects the balance of the entire family group and causes adaptive changes in the other members that lead to different styles and rhythms of the grieving process. It can be helpful for the woman to be given existing resources around perinatal grief such as ‘Support Groups for Mothers’, associations, books, music, and contact with a specialised professional, such as a perinatal psychologist.
CF8. Provision of an environment of support, protection and mental, physical, socio-cultural and spiritual healingPCC8: In this Caritas process, the aim is to create a safe external environment and an internal environment of relaxation and peace, making the woman feel safer, less fearful and less vulnerable. To do this, information relating to perinatal grief should be increased during pregnancy itself and social awareness of this grief extended. To provide the woman with a safe and supportive environment at all levels, her partner, family and social environment must be able to meet her needs. For this reason, and given the secrecy and taboo that has long existed around perinatal loss, it is important to educate and train the woman, her partner and the social environment that surrounds the woman, to provide them with tools that help them understand, validate and accompany her in this complex and difficult loss.
CF9. Assistance in satisfying human needsPCC9: In the care relationship, the woman who has lost a child should be helped to satisfy her basic and transcendental needs. To do this, care should be taken of the physical aspects of the woman such as the process of administering medication, bleeding, pain… as well as the emotional aspects mentioned above and which are basic needs for the well-being of the woman going through perinatal grief.
CF10. Recognition of existential, phenomenological and spiritual forcesPCC10: Nurses should take care of themselves and protect themselves from the suffering of others by introspecting and developing their own grieving processes. As a result, they will be able to be a support in the suffering of others and care for the grieving woman, encouraging her to allow herself to be sad or to listen to herself to know what she wants or needs at each moment of the grieving process.
Discussion/implications for clinical practiceBased on the results of a previous qualitative research study applying the grounded theory methodology,8 it was shown that a person in perinatal mourning needs not only immediate physical care and interventions for their recovery, but also emotional and human care in their mourning process that will continue from the moment of the loss until they are able to draw on and resolve the grief for the lost child. Women who experience these processes need to be cared for holistically.3,6
In the NANDA-I, NIC and NOC Taxonomies we find labels that can illustrate the proposed care plan. Among the NANDA-I nursing diagnoses we can identify: Risk for maladaptive grief (00302), Risk for spiritual distress (00067) or Compromised family coping (00074). The most relevant NOC results would be: Postpartum maternal health behaviour (1624), Grief resolution (1304), Coping with problems (1302) or Family functioning (2602). Finally, the NIC interventions that can best describe the proposed care plan would include: Facilitating grief: perinatal death (5294), Facilitating spiritual growth (5426), Family support (9140) and Postpartum care (6930).
The lack of training of nurses in perinatal grief can be mitigated with nursing theories that allow them to provide excellent care and achieve quality of care optimisation.2,3 The use of Watson’s Transpersonal Human Care theory can guide and empower nurses to provide holistic and humanised care based on self-knowledge and the establishment of the nurse-patient relationship,4,5,9 which strengthens professional identity and creates new perspectives for ethical and humane nursing, with no loss of scientific vision, but guided by the highest human values.10
ConclusionUsing Jean Watson’s Theory of Human Care as a framework, we proposed the use of the 10 caritas care processes described above and adapted to perinatal grief and the individual experience of each woman who experiences it. Through the holistic care of nurses attending to all the dimensions of the grieving woman, the proposal is to help her to move along the path of grieving and to accept the duality of life and death.
Ethical considerationsEthical approval for this study was obtained from the Clinical Research Ethics Committee of Navarra (identification number: 2016/39). Participation was free and voluntary, with the option to withdraw from the study at any time during the research. All participants signed “Informed Consent” forms and confidentiality and anonymity of participants were always guaranteed through the use of codes.
Total or partial funding of the study if applicableIn accordance with the usual requirements, we declare that this manuscript has not been published in whole or in part elsewhere and is not currently being considered for publication elsewhere. At the time this manuscript was submitted for publication, there was no external funding or support for this research.
Authors’ contributionsAll authors contributed significantly to the preparation of this manuscript following the guidelines of the International Committee of Medical Journal Editors.
SFE, BMF and PEH: Made substantial contributions to the conception and design, or acquisition of data, or analysis and interpretation of data.
SFE, BMF and PEH: Were involved in drafting the manuscript or revising it critically for important intellectual content.
SFE, BMF and PEH: Gave final approval of the version to be published. Each author was sufficiently involved in the work to take public responsibility for appropriate parts of the content.
SFE, BMF and PEH: Agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work were appropriately investigated and resolved.
Sara Furtado-Eraso: Conceptualisation, Formal analysis, Methodology, Writing - original draft, Writing - review and editing; Blanca Marín-Fernández: Methodology, Supervision, Writing - review and editing; Paula Escalada-Hernández: Methodology, Supervision, Writing - review and editing.
Conflict of interestsThe authors have no conflict of interests to declare and an ethical declaration is not applicable in this manuscript.
Availability of dataThe data supporting the findings of this study are available from the corresponding author, [SFE], upon reasonable request.
The authors express their deepest gratitude to the mothers who participated in this study.