Major burns patients usually present hypothermia after suffering a thermal burn, due to exposure during the accident, cooling of the burn and transfer. There are methods of reheating to avoid this heat loss, where nursing care is key.
ObjectiveTo analyse the constant temperature presented by large burns patients on admission to the Burns Unit and their progression over the first 72h.
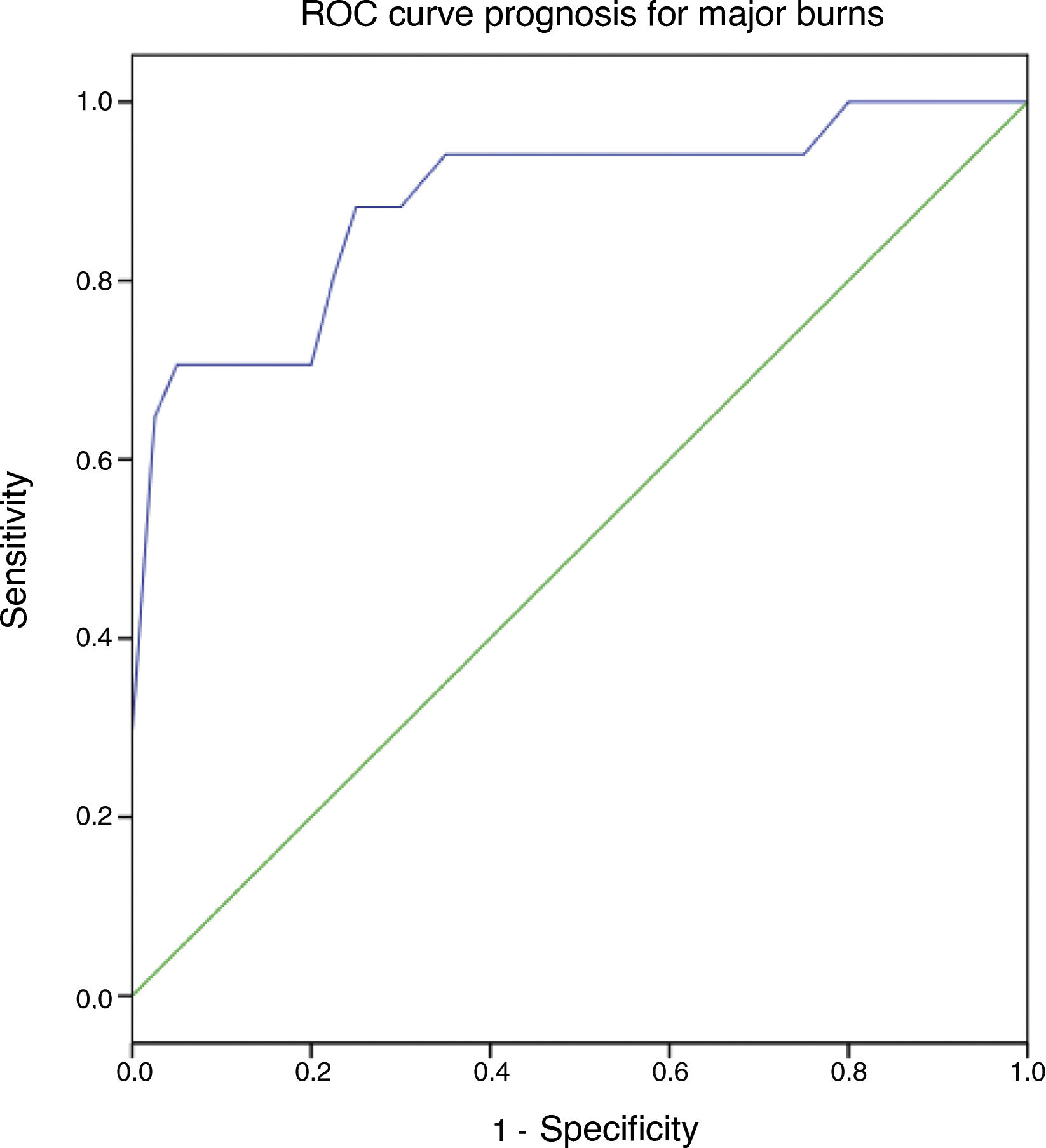
MethodRetrospective cross-sectional descriptive observational study of patients with thermal burns affecting more than 15% of body surface area, from December 2010 to May 2018. By reviewing databases and clinical records, demographic data, qualitative variables (origin of burn, previous pathologies, mechanical ventilation and ABSI and BOBI scales) and quantitative variables (burn depth and extension, temperature at admission and taken every 8h for 72h). Absolute, relative frequencies and the statistics of the quantitative variables were analysed. The study was verified by statistical tests according to the variables and contingency tables. A logistic regression model was developed expressed in a ROC curve.
ResultsOf the 57 patients included, 79.2% developed hypothermia on admission. They presented burns over 34.56%±16.64 of their body surface, with 28.04%±17.49 being deep burns. Mortality during the stay was 29.8%. The presence of hypothermia during the acute phase was statistically related to death during stay in the unit (p=0.033). It was observed that hypothermia is directly related to the extent of the burn (p=0.003).
ConclusionsDue to the presence of hypothermia on admission, and to the fact that the average temperature does not exceed 36°C until at least 16h after the burn, nurses must know and promptly administer adequate reheating measures to improve chances of survival in major burns.
Los grandes quemados habitualmente presentan hipotermia tras sufrir una quemadura de origen térmico debido a la exposición durante el accidente, enfriamiento de la quemadura y el traslado. Existen métodos de recalentamiento para evitar esta pérdida de calor, donde los cuidados enfermeros son claves.
ObjetivoAnalizar la constante temperatura que presentan los grandes quemados en la admisión en la unidad de quemados y su evolución durante las primeras 72horas.
MétodoEstudio observacional descriptivo transversal retrospectivo en pacientes con quemaduras térmicas con criterios de gran quemado, desde diciembre de 2010 hasta mayo de 2018. Mediante revisión de bases de datos e historias clínicas se recogieron los datos demográficos, variables cualitativas (origen de la quemadura, enfermedades previas, ventilación mecánica y escalas ABSI y BOBI) y variables cuantitativas (extensión y profundidad de quemadura, temperatura al ingreso y cada 8horas hasta las 72horas). Se analizaron frecuencias absolutas, relativas y los estadísticos de las variables cuantitativas. Se comprobó mediante test estadísticos en función de las variables y tablas de contingencia. Se desarrolló un modelo de regresión logística expresado en una curva ROC.
ResultadosDe los 57 pacientes incluidos el 79,2% mostró hipotermia al ingreso, con una temperatura media de 34,43±1,98°C. Presentaron quemaduras en el 34,56±16,64% de su superficie corporal, siendo quemadura profunda en el 28,04±17,49%. La mortalidad durante la estancia fue del 29,8%. La presencia de hipotermia durante la fase aguda se relacionó estadísticamente con el fallecimiento en estancia (p=0,033). Se observó que la hipotermia está directamente relacionada con la extensión de la quemadura (p=0,003).
ConclusionesDebido a la presencia de hipotermia al ingreso, y a que la temperatura media no supera los 36°C en quemados hasta pasadas 16horas desde la quemadura, las enfermeras deben conocer y administrar tempranamente las medidas de recalentamiento adecuadas para mejorar la supervivencia en grandes quemados.
The pathophysiological effects and response triggered by thermal burns, as well as the rationale for the treatment of hypothermia by individual thermoregulation in burns patients and the measures that can be applied.
We provide a united vision of the treatment of hypothermia from the time the burn occurs and during the acute phase. By studying the response of patients to routine treatment the hypothesis of hypothermia through the acute phase is confirmed and the nursing care provided is assessed.
Implications of the studyThe study involves in-depth knowledge of temperature regulation through the acute phase in major burns patients and evaluation of nursing care in thermoregulation which is necessary to review the suitability of the standardised care plan.
Hypothermia, acidosis and coagulopathy are the lethal triad in major burns.1 People who have suffered major body surface thermal burns that affect the deep skin layers usually develop hypothermia following the burn and receive more appropriate care when transferred to a Burns Unit.2
Pathophysiological changes in the first hoursExtensive burns trigger a systemic inflammatory response, manifested by symptoms similar to sepsis, therefore it is necessary to differentiate between the two processes. This inflammatory response is the primary cause of hypermetabolism in major burns patients. At least during the first week following the accident, and up to 2 months thereafter, irrespective of the body surface without coverage, both the surface temperature and the core temperature are elevated. In the first 72h there will be a decrease in this response, then a hypermetabolic phase that will last more than 9 months after the burn.3 The loss of a large area of skin alters the peripheral capacity to maintain thermoregulation, and therefore to avoid excessive temperature loss a higher external temperature is required. The hypothermic response, even in the absence of infection, is caused by inflammation mediators, stimulated by the hypothalamic regulatory centre.4
HypothermiaTechnically hypothermia occurs when the internal temperature is below 36.5°C; however, the clinical threshold for healthy subjects is considered to be less than 35°C. Hypothermia can be classified into 3 groups: mild from 35°C to 32°C, moderate from 32°C to 30°C and severe below 30°C. For patients with injuries this changes slightly: mild from 36°C to 34°C, moderate from 34°C to 32°C and severe below 32°C.5
Effects of hypothermiaHypothermia has several detrimental effects: impaired immune and stress responses, impaired clotting and platelet function, dysfunction of normal neurological and cardiac homeostasis, arrhythmias, respiratory depression, decreased oxygen supply, decreased responsiveness of the central nervous system, worsening of acidosis, and impaired wound healing.6,7 The burns patient is predisposed to hypothermia due to the large amount of intravenous fluid without a warming system used in resuscitation, heat loss through conduction and evaporation due to heat escape from burned skin4 and exposure of the patient during transport and wound care.7 These patients cannot produce the heat needed to raise their temperature, leading to an increased inability to overcome stress factors. For these reasons Shiozaki et al. concluded that this inability to generate heat and the resulting hypothermia increases morbidity and mortality in these patients.8
An important distinction should be made between induced hypothermia and spontaneous or accidental hypothermia:
- •
Induced hypothermia is a controlled state in which the metabolic rate decreases and shivering is prevented, but cellular energy reserves are maintained.9
- •
Accidental hypothermia is defined as an involuntary decrease in core temperature during exposure to cold in people without intrinsic thermoregulatory dysfunction.9
In the case of accidental hypothermia, homeostatic mechanisms counteract the decrease in body temperature, which produces physiological stress and a decrease in the effectiveness of rewarming. In addition, depending on the severity of the injury, and of the accidental hypothermia, hypothermia causes depletion of plasma ATP levels (increasing cardiac output and oxygen consumption). By contrast, induced hypothermia preserves ATP storage.9 Shafi et al. argued that hypothermia is an independent risk factor for increased mortality due to the severity of the burn, and therefore must be prevented in these patients.10
Heat regulation in burns patientsDespite advances in resuscitation, wound coverage, and infection control, burns patients still have significant morbidity and mortality secondary to complex metabolic changes after the burn. These changes are called hypermetabolism and are characterised by increased body temperature, glycolysis, proteolysis, and lipolysis.
Wilmore et al.11 showed that ambient temperature significantly influences the hypermetabolic response after the accident. They suggested that burns patients require a core body temperature of 38.5°C and that increased ambient temperature would greatly reduce the hypermetabolic response. In fact, they showed that raising the ambient temperature to 33°C instead of 20°C decreased resting energy from 2.0 to 1.4 in patients with burns greater than 40% of total burned body surface area. Without appropriate ambient temperature the metabolic rate increases to compensate for profound water and heat loss. Water loss is estimated at approximately 4000ml/m2 of the burns surface area per day.12 The body's natural response is to raise the core and skin temperature 2°C more than normal in that of non-burns patients.13
Therefore, ambient temperature up to 33°C should be maintained to reduce unnecessary calorie expenditure and decrease the hypermetabolic response that occurs with lower ambient temperatures. This intervention, however, does not completely eliminate the effects of hypermetabolism.14
Measures to prevent heat loss- •
Conduction: the patient should be moved from any cold surface as quickly as possible and placed on a surface that is warmer or that protects them from continuous heat loss.
- •
Convection: move the patient from any wet or windy atmosphere as soon as possible.
- •
Radiation: cover as much of the patient as possible to prevent heat loss to the environment.
- •
Evaporation: damp and sweaty patients lose body heat.15
According to the recommendations of the International Society for Burn Injury, flame burns should be cooled, optimally with clean running water, and the temperature adjusted to the person's preference for 15–20min. After cooling, the patient should be kept warm.16 When transferring a burns patient it is important to ensure that they are not transported with wet dressings. Prolonged use of hydrogel dressings can cause hypothermia. Because the benefits of cooling are heterogeneous between superficial and deep burns, there is a current line of research.17 If hypothermia develops, cooling should be discontinued. In addition, early bleeding should be controlled, as bleeding can also lead to hypothermia. The administration of cold intravenous fluids, sedatives or prolonged evacuation time can worsen heat loss in burns patient.15,18,19
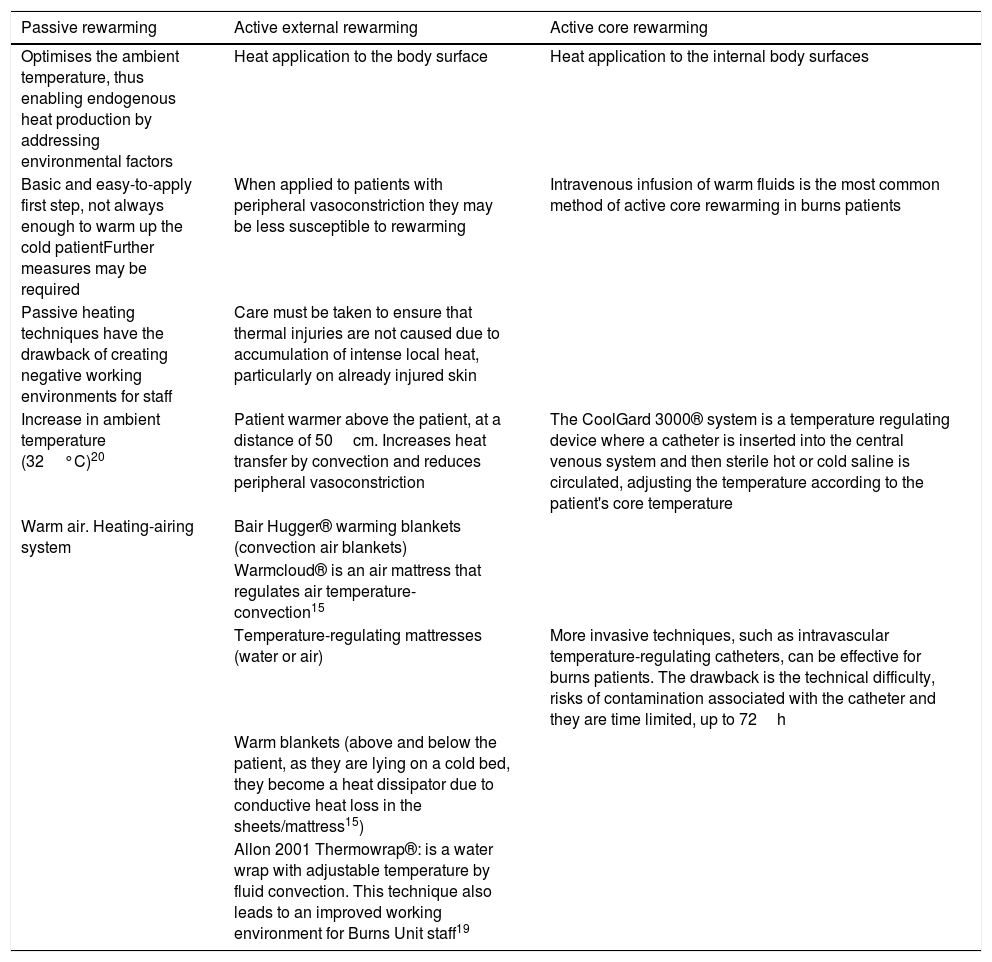
Rewarming methodsThree general strategies can be used to rewarm hypothermic patients (Table 1).
Rewarming strategies in the acute phase in burns patients.
| Passive rewarming | Active external rewarming | Active core rewarming |
|---|---|---|
| Optimises the ambient temperature, thus enabling endogenous heat production by addressing environmental factors | Heat application to the body surface | Heat application to the internal body surfaces |
| Basic and easy-to-apply first step, not always enough to warm up the cold patientFurther measures may be required | When applied to patients with peripheral vasoconstriction they may be less susceptible to rewarming | Intravenous infusion of warm fluids is the most common method of active core rewarming in burns patients |
| Passive heating techniques have the drawback of creating negative working environments for staff | Care must be taken to ensure that thermal injuries are not caused due to accumulation of intense local heat, particularly on already injured skin | |
| Increase in ambient temperature (32°C)20 | Patient warmer above the patient, at a distance of 50cm. Increases heat transfer by convection and reduces peripheral vasoconstriction | The CoolGard 3000® system is a temperature regulating device where a catheter is inserted into the central venous system and then sterile hot or cold saline is circulated, adjusting the temperature according to the patient's core temperature |
| Warm air. Heating-airing system | Bair Hugger® warming blankets (convection air blankets) | |
| Warmcloud® is an air mattress that regulates air temperature-convection15 | ||
| Temperature-regulating mattresses (water or air) | More invasive techniques, such as intravascular temperature-regulating catheters, can be effective for burns patients. The drawback is the technical difficulty, risks of contamination associated with the catheter and they are time limited, up to 72h | |
| Warm blankets (above and below the patient, as they are lying on a cold bed, they become a heat dissipator due to conductive heat loss in the sheets/mattress15) | ||
| Allon 2001 Thermowrap®: is a water wrap with adjustable temperature by fluid convection. This technique also leads to an improved working environment for Burns Unit staff19 |
Warmed intravenous fluids in combination with other warming strategies have been shown to be an effective approach in the treatment of hypothermia (grade B evidence).15
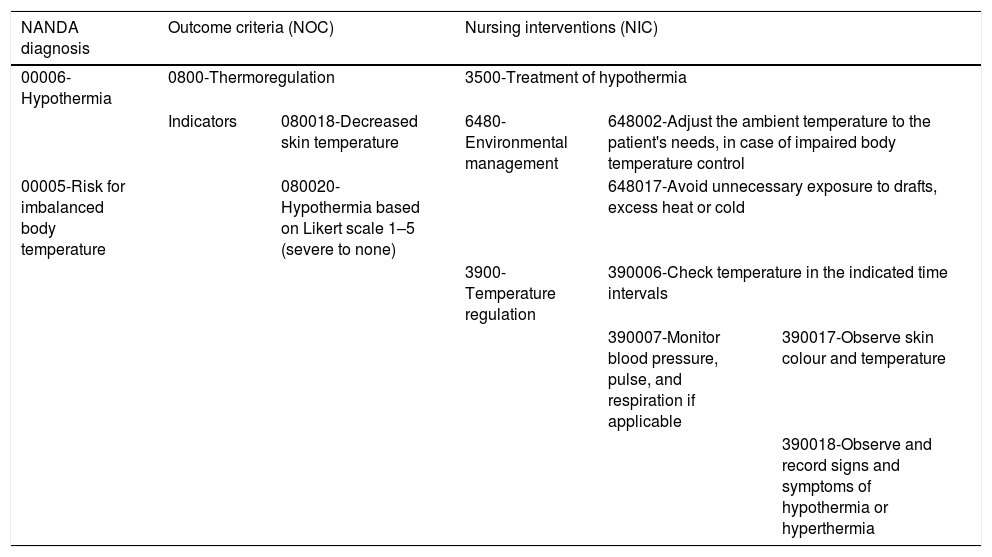
Nursing care planThese nursing actions are carried out systematically in the standardised care plan. After comprehensive assessment of the patient, nursing diagnoses will be defined within the metabolic nutritional pattern, establishing outcome criteria and interventions as shown in the NNN interrelationship in Table 2.21–23 Based on the risk in major burns of developing hypothermia and the mechanisms of temperature regulation described above, our aim is to study the factors that influence temperature on admission to our Burns Unit, where the history and characteristics of the person, as well as the extension of the burn, are considered the main elements of risk for hypothermia. We also assess other factors such as the season of the year or travel time that could be associated with hypothermia and mortality.
Nursing process in temperature control in the acute phase of the major burns patient.
| NANDA diagnosis | Outcome criteria (NOC) | Nursing interventions (NIC) | |||
|---|---|---|---|---|---|
| 00006-Hypothermia | 0800-Thermoregulation | 3500-Treatment of hypothermia | |||
| Indicators | 080018-Decreased skin temperature | 6480-Environmental management | 648002-Adjust the ambient temperature to the patient's needs, in case of impaired body temperature control | ||
| 00005-Risk for imbalanced body temperature | 080020-Hypothermia based on Likert scale 1–5 (severe to none) | 648017-Avoid unnecessary exposure to drafts, excess heat or cold | |||
| 3900-Temperature regulation | 390006-Check temperature in the indicated time intervals | ||||
| 390007-Monitor blood pressure, pulse, and respiration if applicable | 390017-Observe skin colour and temperature | ||||
| 390018-Observe and record signs and symptoms of hypothermia or hyperthermia | |||||
The objective of the study is to analyse the temperature maintained by patients with thermal burns on admission and during the first 72h of the acute phase in the Burns Unit. The aim is to check whether patients present hypothermia on admission and how this parameter progresses during the first hours of their stay. The specific objectives are: to describe the characteristics of the sample and the variables related to the burn, to analyse states of hypothermia or normothermia and their relationship with survival through survival and mortality prediction scales: Abbreviated Burn Severity Index (ABSI) and Belgian Outcome of Burn Injury (BOBI)24 and to describe the factors that influence the mortality of these patients.
Material and methodsA retrospective cross-sectional descriptive observational study was conducted on burns patients admitted in the last 8 years, from December 2010 to May 2018 to our 4-bed critical care unit. The participants were elderly patients with thermal burns, with criteria for admission to the major Burns Unit. This design allowed us to determine the progression of the temperature variable over time, identifying risk groups by burned body surface area, degree of hypothermia on admission or presence of previous diseases, and to identify possible variables affecting the nursing process in temperature control.
The measurements of the main temperature variable were taken at body level, in the axillary or inguinal area, by means of a Hartmann Thermoval® electronic clinical thermometer, with 0.1°C accuracy, complying with the requirements of use and safety, respecting the indications of temperature and environmental humidity described by the manufacturer.
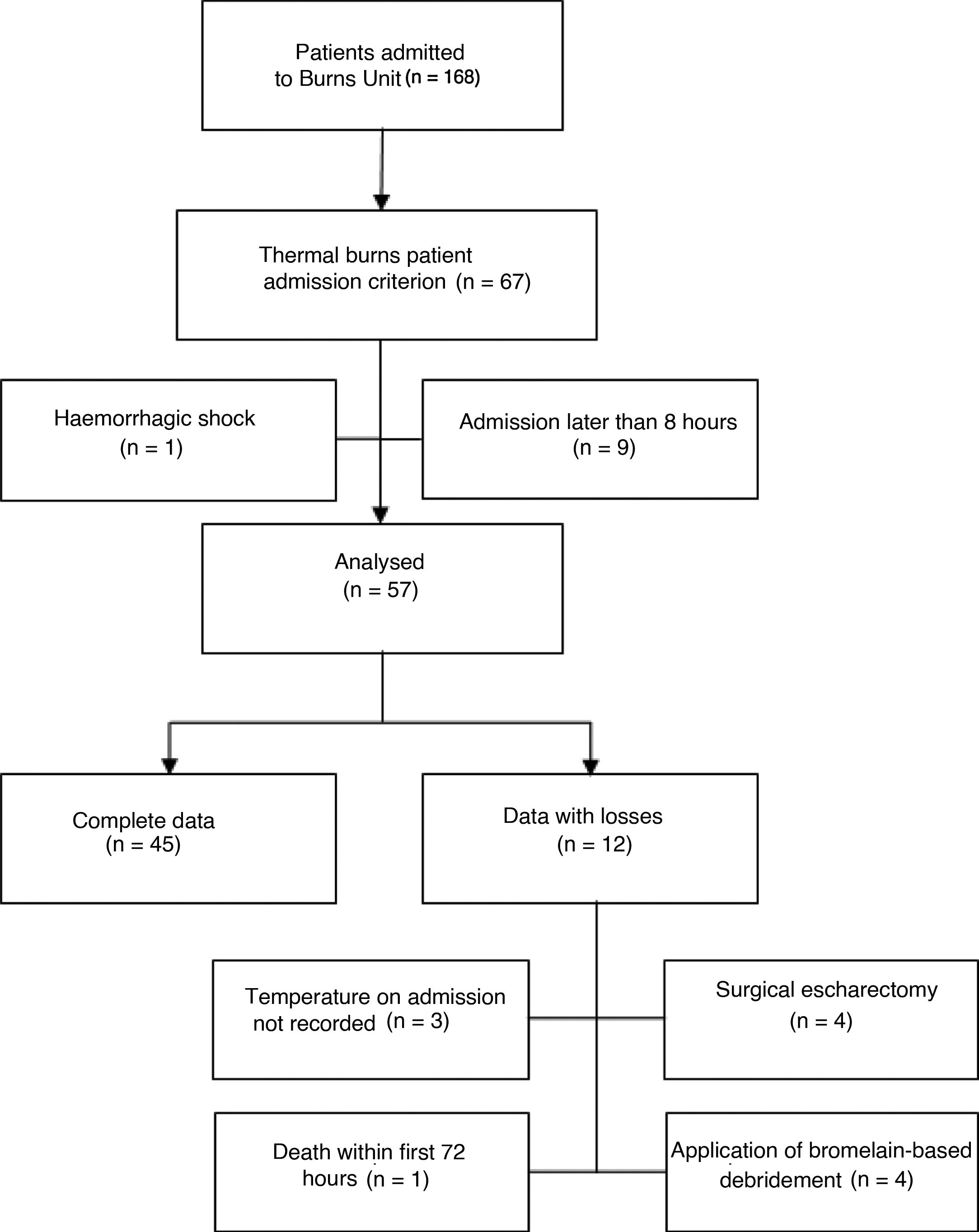
In addition, conditions were defined that could vary the outcome of the study of body temperature progression to control for confounding variables, and therefore subjects were excluded who had been admitted 8h after the accident, since temperatures on admission could bias the data and alter the scale data collection pattern of every 8h, and if there had been haemorrhagic shock due to its association with hypothermia. Other processes were treated as loss of data: patients who were transferred to the operating room during the first 72h to undergo burn escharectomy, because of the time of exposure and its hypothermic effect, patients with bromelain-based enzymatic debridement, because of the inflammatory reaction that can cause hyperthermia, and patients whose temperature had not been recorded on admission.
The study authors individually collected data including all possible candidates in June 2018, and they were validated by at least one other investigator. Data were collected by reviewing clinical histories and databases. Data processing was coded, ensuring the anonymity of the participants. Demographic data, previous illnesses, information about the accident, characteristics of the burn, length of stay in the Burns Unit, use of mechanical ventilation, survival and mortality scales and progression of the temperature variable were collected.
Temperature control is managed through the following protocolised actions: ambient temperature of 28°C, closed and individual room with positive pressure as passive external rewarming methods, anti-perspiration blanket and reduced body exposure. The Aspira® MTC 400 patient warmer was used in the emergency room and the room as a method of active external rewarming. This is a height-adjustable heating device, up to 50cm from the patient, with a skin temperature probe, which generates radiant heat at low temperature (up to 39°C) distributed evenly.
The study, Ref.:PI084-18, was approved by the research ethics committee of the referral centre. The authors declare that they have no personal or financial conflict of interest and comply with confidentiality, data protection and research bioethics standards.
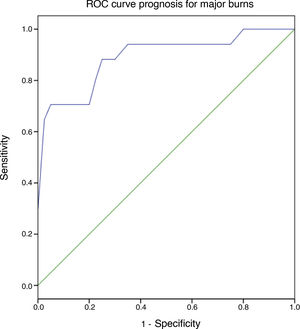
Discrete qualitative and quantitative variables were analysed using absolute and relative frequency tables. For continuous quantitative variables, the following statistics were found: median, mean, standard deviation (SD), extreme values and quartiles. A descriptive analysis of the variables collected was carried out. The distribution of the variables was checked by means of the Kolmogorov–Smirnov test. In the analytical statistics of qualitative variables, contingency tables were used applying the Chi-square test or Fisher's test depending on the distribution of the variables. For the comparison of differences between independent means, the student's t- or Mann–Whitney's U-test was used according to the distribution of the variables. Rho Spearman's coefficient was applied to measure the degree of correlation between freely distributed quantitative variables. If necessary, truncation of the variables was applied to calculate the test statistics. Multivariate analysis of the variables introduced in a logistic regression model was performed, determining the association of variables with mortality during the stay in the Burns Unit. The predictive capacity of the model was expressed by means of a ROC curve, the area under the curve showing a predicted probability with a 95% confidence interval. The statistical analysis was performed with Microsoft Excel® v 14.07 and IBM SPSS® Software v 23.0. Statistical significance was estimated at p<0.05.
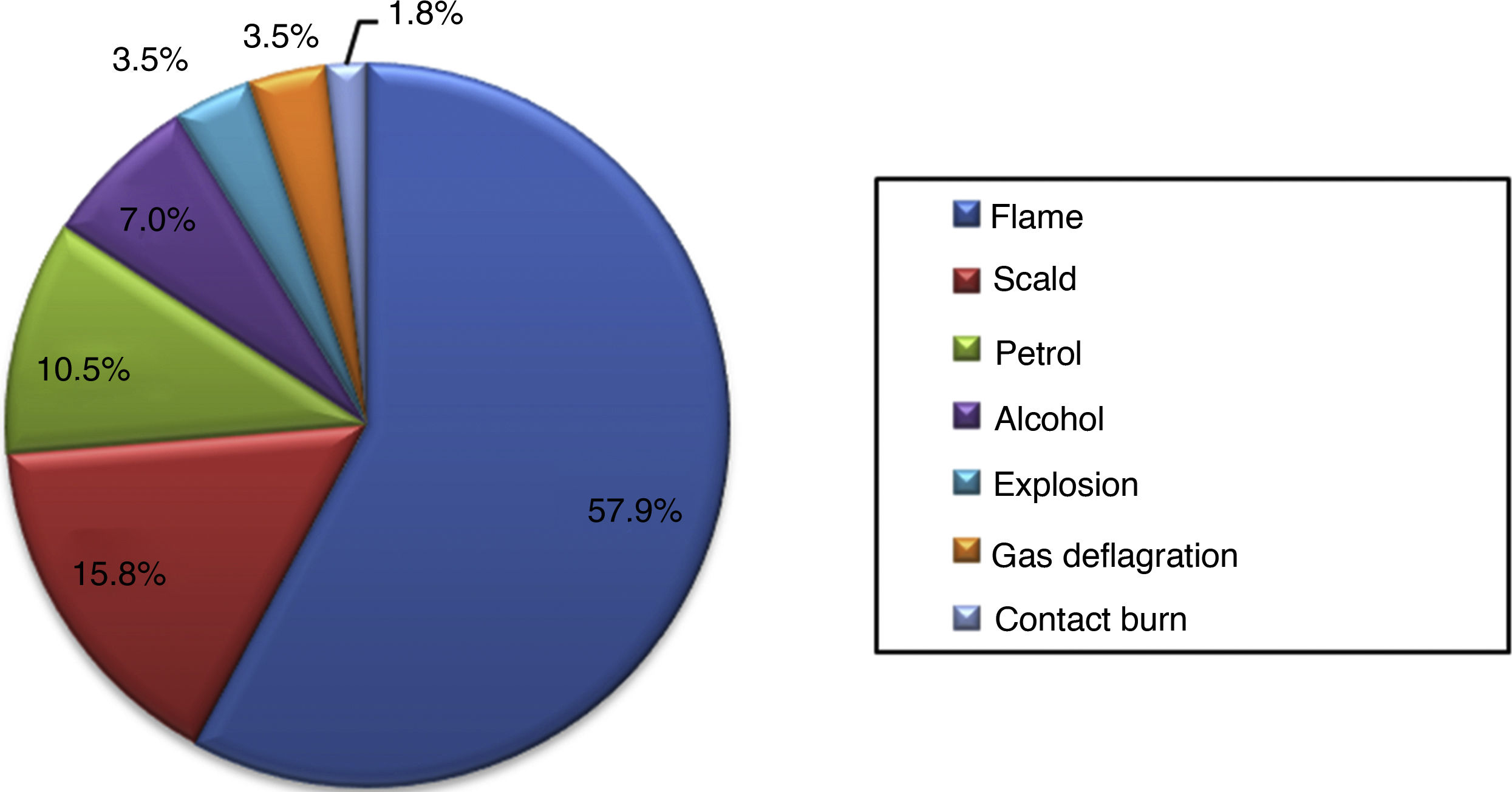
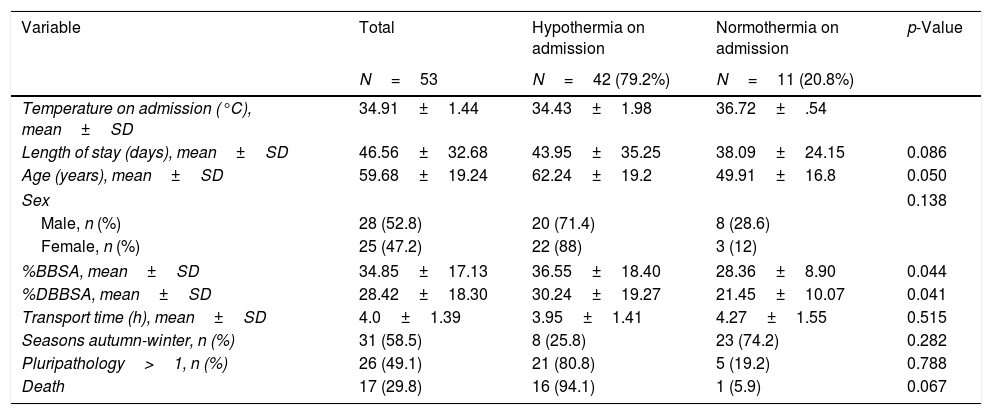
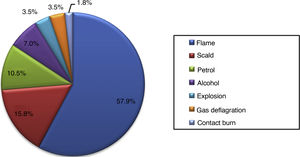
ResultsThe study participants were selected by applying the criteria of inclusion, exclusion, and treatment of loss of data as shown in Fig. 1, including a total of 57 major burns. The characteristics of the patients with thermal burns are detailed in Table 3, dividing the sample into groups of hypothermia and normothermia on admission and in the first 72h. The aetiology of the thermal burns of the patients included in the study is shown in Fig. 2. We observe that 79.2% of the subjects included in the study presented hypothermia on admission, 34.9°C (median), 34.05–35.9°C (IQR), being severe in 3.8% of cases.
Characteristics of burns patients and according to the presence of hypothermia or normothermia on admission and in the 72h of the acute phase.
| Variable | Total | Hypothermia on admission | Normothermia on admission | p-Value |
|---|---|---|---|---|
| N=53 | N=42 (79.2%) | N=11 (20.8%) | ||
| Temperature on admission (°C), mean±SD | 34.91±1.44 | 34.43±1.98 | 36.72±.54 | |
| Length of stay (days), mean±SD | 46.56±32.68 | 43.95±35.25 | 38.09±24.15 | 0.086 |
| Age (years), mean±SD | 59.68±19.24 | 62.24±19.2 | 49.91±16.8 | 0.050 |
| Sex | 0.138 | |||
| Male, n (%) | 28 (52.8) | 20 (71.4) | 8 (28.6) | |
| Female, n (%) | 25 (47.2) | 22 (88) | 3 (12) | |
| %BBSA, mean±SD | 34.85±17.13 | 36.55±18.40 | 28.36±8.90 | 0.044 |
| %DBBSA, mean±SD | 28.42±18.30 | 30.24±19.27 | 21.45±10.07 | 0.041 |
| Transport time (h), mean±SD | 4.0±1.39 | 3.95±1.41 | 4.27±1.55 | 0.515 |
| Seasons autumn-winter, n (%) | 31 (58.5) | 8 (25.8) | 23 (74.2) | 0.282 |
| Pluripathology>1, n (%) | 26 (49.1) | 21 (80.8) | 5 (19.2) | 0.788 |
| Death | 17 (29.8) | 16 (94.1) | 1 (5.9) | 0.067 |
| Characteristics of burns patients and according to the presence of hypothermia or normothermia in the acute phase (72h) | ||||
|---|---|---|---|---|
| Acute phase hypothermia | Acute phase normothermia | |||
| N=57 | N=43 (75.4%) | N=14 (24.6%) | ||
| Death, n (%) | 17 (29.8) | 16 (94.1) | 1 (5.9) | 0.033 |
| Sex | 0.036 | |||
| Male, n (%) | 31 (54.4) | 20 (64.5) | 11 (35.5) | |
| Female, n (%) | 26(45.6) | 23 (88.5) | 3 (11.5) | |
| Mechanical ventilation, n (%) | 39 (68.4) | 30 (76.9) | 9 (23.1) | 0.702 |
%BBSA: burned body surface area; %DBBSA: deep burned body surface area.
As for the time period in which the accidents occurred, most of the burns occurred early in the morning and early in the afternoon: 19.3% between 8:00 and 10:00 (n=11), and 28.1% between 14:00 and 16:00 (n=16) 28.1%, which added together form 47.4% of daily total accidents.
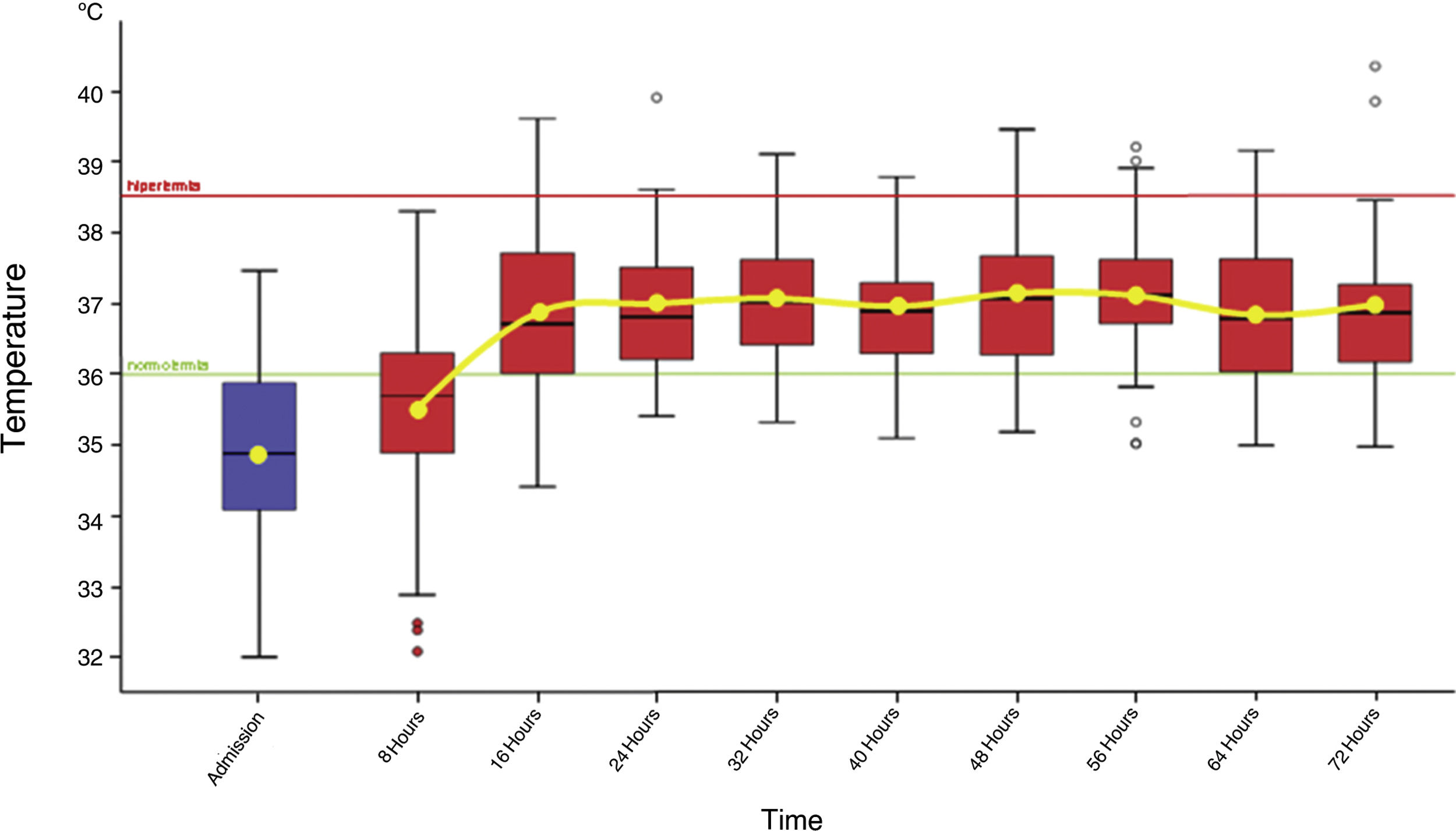
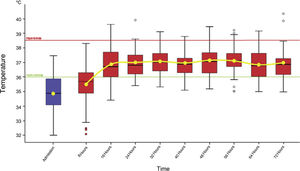
The temperatures collected on admission, every 8h and even 72h since the burn occurred, were grouped in box plots, identifying the average temperatures and their progression. The desired temperature range was established between 36°C, which establishes normothermia, and 38.5°C, from which hyperthermia was considered. Fig. 3 shows how normothermia is not restored until 16h following the accident.
The interventions aimed at rewarming and maintaining the burns patient's body temperature were evaluated by analysing the variation in temperature measured at 2 set times:
- 1)
Difference in temperature between admission and at 8h:
ΔT admission-8h: mean 0.51°C±0.83 SD. min: −1.4°C; max: 3.1°C (n=53).
- 2)
Difference in temperature between 8 and 16h:
ΔT 8h–16h: mean 1.39°C±1.62 SD. min: −1.8°C; max: 5°C (n=57).
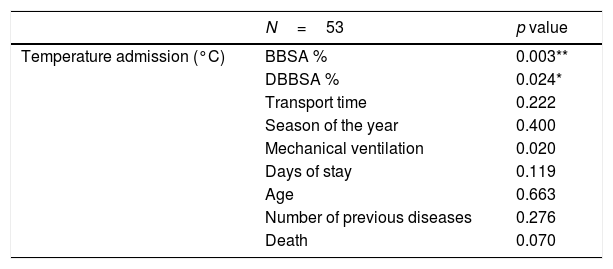
The association with the different variables was checked to establish the factors that have a relationship with the body temperature of patients with thermal burns on admission to the Burns Unit, as detailed in Table 4.
Statistical analysis of temperature on admission of burns patients by means of contingency tables.
| N=53 | p value | |
|---|---|---|
| Temperature admission (°C) | BBSA % | 0.003** |
| DBBSA % | 0.024* | |
| Transport time | 0.222 | |
| Season of the year | 0.400 | |
| Mechanical ventilation | 0.020 | |
| Days of stay | 0.119 | |
| Age | 0.663 | |
| Number of previous diseases | 0.276 | |
| Death | 0.070 |
BBSA: burned body surface area; DBBSA: deep burned body surface area.
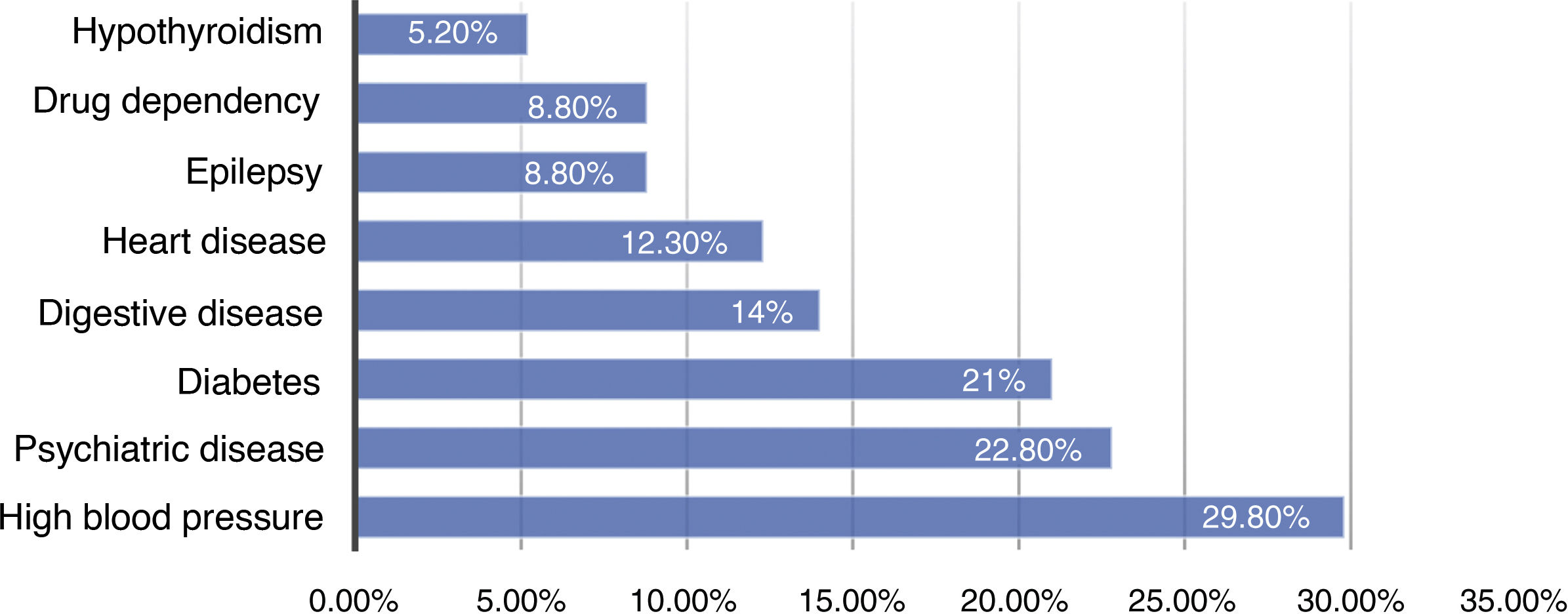
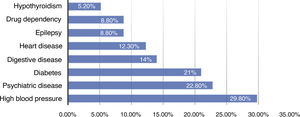
The proportion of associated diseases of these patients was: without a disease process 9.3%, with a disease process 35%, 2 conditions 22.8%, 3 diseases 12.3% and more than 3 diseases 10.6%. The aetiology of these previous conditions and their proportion is represented in Fig. 4.
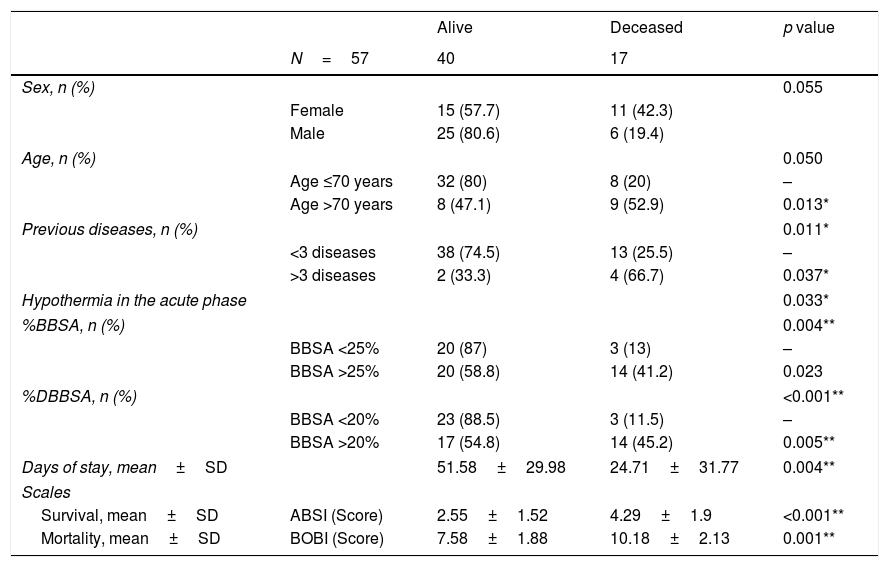
To determine the causes of mortality of these patients, the relationship with the different variables was studied, and then these variables were dichotomised to study mortality by means of contingency tables (Table 5). The results for each group of the BOBI and ABSI scales are also detailed, with an overall result of 3, IQR [2–4] and 8, IQR [7–10] points, respectively.
Analysis and contingency tables of factors related to the death of patients with thermal burns.
| Alive | Deceased | p value | ||
|---|---|---|---|---|
| N=57 | 40 | 17 | ||
| Sex, n (%) | 0.055 | |||
| Female | 15 (57.7) | 11 (42.3) | ||
| Male | 25 (80.6) | 6 (19.4) | ||
| Age, n (%) | 0.050 | |||
| Age ≤70 years | 32 (80) | 8 (20) | – | |
| Age >70 years | 8 (47.1) | 9 (52.9) | 0.013* | |
| Previous diseases, n (%) | 0.011* | |||
| <3 diseases | 38 (74.5) | 13 (25.5) | – | |
| >3 diseases | 2 (33.3) | 4 (66.7) | 0.037* | |
| Hypothermia in the acute phase | 0.033* | |||
| %BBSA, n (%) | 0.004** | |||
| BBSA <25% | 20 (87) | 3 (13) | – | |
| BBSA >25% | 20 (58.8) | 14 (41.2) | 0.023 | |
| %DBBSA, n (%) | <0.001** | |||
| BBSA <20% | 23 (88.5) | 3 (11.5) | – | |
| BBSA >20% | 17 (54.8) | 14 (45.2) | 0.005** | |
| Days of stay, mean±SD | 51.58±29.98 | 24.71±31.77 | 0.004** | |
| Scales | ||||
| Survival, mean±SD | ABSI (Score) | 2.55±1.52 | 4.29±1.9 | <0.001** |
| Mortality, mean±SD | BOBI (Score) | 7.58±1.88 | 10.18±2.13 | 0.001** |
%BBSA: percentage of burned body surface area; %DBBSA: percentage of deep burned body surface area.
A logistic regression model was adjusted to explain mortality (n=57) by age, burned body surface area associated with deep burned body surface area, previous associated diseases, and hypothermia during the acute phase (temperature under 36°C). An adjusted model was obtained with the variables entered according to automated criteria; p=0.003. The logistic regression analysis indicated an 89.5% probability of predicting mortality when the criteria included in the model are met. The Nagelkerke's R2 value indicates that the model shown explains 0.620 of the mortality variance. A ROC curve was designed (Fig. 5) with an area under curve of 89.3% (95% CI: 0.791–0.994) prognostic probability of mortality analysed.
Significantly related to mortality were: age (p=0.011; OR: 1.068; 95% CI: 1.000–1.003), previous diseases (p=0.021; OR: 1.833; 95% CI: 1.010–1.129) and the variable of the interaction of depth of body surface burned with depth (p=0.05; OR 1.068; 95% CI: 1.001–3.357).
DiscussionAccording to the data collected and analysed throughout the study exclusively in major burns, compared with the other studies that collect all types of extensions and burns, we observed hypothermia on admission, which would be explained by exposure at the time of the accident and cooling of the burn.
The transfer time to the unit is considered relevant, due to the great geographical dispersion; the territorial coverage area is 94,226km2, where the distance to the healthcare centre can be as much as 275km, a circumstance that could delay the start of rewarming in the Burns Unit, although no relationship with hypothermia was found in this study.
As regards the season of the year in which the burn occurs, there is no relationship between lower temperatures of patients on admission and the seasons considered colder, despite the fact that in the coldest periods of the winter temperatures can reach −10°C, even recording minimum temperatures of −20°C in high points of the region. Steele et al. do not establish a relationship between hypothermia and external agents either.25 However, Hostler et al. found a higher incidence in winter and spring.26
It is observed that a greater number of burns occur in the early morning and early afternoon, possibly related to the beginning or end of an activity.
The nursing actions carried out from 8 to 16h after the accident are important for correct rewarming, thus reaching a safe temperature range. The established procedures were confirmed to have been undertaken correctly, as patients were kept at an average temperature close to 37°C, although, prior to the study, participants were expected to maintain a temperature closer to 38°C by the end of the acute phase.
The high presence of mechanical ventilation for the first 72h in these patients should be reflected upon, and measures included in the rewarming strategy, such as heated humidification of the ventilatory circuit from the outset. The application of warming prior to exposure could help prevent the body temperature lowering, as hypothermia is considered life-threatening.27
Severe hypothermia in patients admitted for rewarming in ICU is 13% in the study by Sequeira,28 in contrast to the scarce presence of severe hypothermia in our study. Hostler and Weaver recorded a 40%–42% presentation of hypothermia on admission in patients with burns.2,26
The intensity of hypothermia on admission does not show an association with mortality in this type of patient, but it does show an association when the patient presents with hypothermia in the acute phase, therefore, rewarming measures are considered effective and should be maintained throughout this phase. The relationship between greater extension of burned body surface area and greater degree of hypothermia is justified.
There is a high mortality rate, which is statistically related to the extension and depth of the burn. Steele shows that hypothermia would be related to the severity of the burn and the physiological state of the patient.25 Burned body surface area (BBSA) greater than 20%, advanced age and other morbidities increase the risk of hypothermia.2
Mortality by group matches that of other studies with that by Hostler et al.: it increases with age, female sex, BBSA>40% and comorbidities.26 It coincides with Singer et al. who showed a relationship between hypothermia and mortality in large burns victims p<0.0001 with no differences between hypothermia and normothermia groups in length of stay in days p=0.426.6
In this sample the dose-dependent effect with respect to mortality is found in patients over 70 years of age, female, with pluripathology (more than 3 previous diseases) and a greater burn extension (greater than 25% BBSA and a surface area greater than 20% of BBSA at total thickness). Hostler et al. also show a dependent effect of greater extension of body burned, lower temperature OR=3.66 [3.15–4.25].26 In contrast to other studies and our results, Steel et al. found no difference in hospital stay (p=0.547) or in hospital mortality (p=0.151).25
Rizzo et al. describe mild hypothermia as a protective factor, there's being induced hypothermia,29 this is not comparable with this study. Tan et al. suggest that intravascular induced hypothermia between 32°C and 34°C would not prolong survival in burns patients.30
Taking these factors into account, efforts to rewarm patients with these characteristics should be increased, since nursing care in this field is observed to have an impact and could reduce mortality.
The effectiveness of the ABSI mortality predictor scales, which would show a moderately severe to severe threat to life, and BOBI survival with a predicted mortality between 5% and 20%, show similar accuracy. In comparison, other studies show an overall score for predicting mortality BOBI=2 IQR (1–4).25 It should also be noted that the proposal for the modified ABSI scale could be even more accurate.31
The limitations of the study are inherent to the retrospective design. We detected that it was not possible to collect some data since they had not been recorded in the records, such as the assessment of the techniques used in burn cooling and rewarming by the emergency teams, and therefore we consider further studies analysing these actions are required.
ConclusionsThe hypothesis of the presence of hypothermia on admission and its association with mortality when present in the acute phase is confirmed. Appropriate rewarming is also observed in patients with thermal burns. Even so, maintaining or increasing rewarming measures should be considered to achieve a higher target temperature in major burns and to be able to decrease metabolic output.
The mean temperature of patients does not exceed 36°C until 16h from the time the burn occurred, which suggests the need to expedite the start of rewarming.
Therefore, nurses must know and apply appropriate rewarming measures promptly in major burns.
Conflict of interestsThe authors have no conflict of interests to declare.
We are deeply grateful to our patients, the true heroes of the Burns Unit, for their guidance, teaching and support.
Please cite this article as: Alonso-Fernández JM, Lorente-González P, Pérez-Munguía L, Cartón-Manrique AM, Peñas-Raigoso MC, Martín-Ferreira T. Análisis de la hipotermia durante la fase aguda del paciente gran quemado: cuidados enfermeros. Enferm Intensiva. 2020;31:120–130.