Fournier’s gangrene, a relatively rare form of necrotizing fasciitis, is a rapidly progressive disease affecting the deep and superficial tissues of the perineal, anal, scrotal, and genital regions. Despite the significant evolution in medical knowledge, there is still scarce evidence regarding the nursing care plan in patients affected by this pathology, which hinders its correct management. For this reason, we present the following clinical case of a 53-year-old male patient with Fournier’s gangrene who was admitted to the emergency department for 3 days of pain in the perineal area and fever.
ObjectiveThe objective was to establish an individualized care plan for the patient detailing the diagnoses, expected outcomes and interventions through nursing taxonomies.
Case developmentA systematic assessment was performed using Marjory Gordon’s model of functional health patterns as a reference. After drawing inferences, three collaborative problems and two nursing diagnoses were established with their outcome criteria and interventions. Once the plan was executed, the results obtained highlighted that the interventions were consistent in achieving the objectives set out in the problems present in the case patient.
ConclusionsThe development of an individualized plan made it possible to detect problems, establish realistic objectives and define interventions that optimized nursing care in this patient with Fournier’s gangrene.
La gangrena de Fournier, una forma relativamente rara de fascitis necrotizante, es una enfermedad rápidamente progresiva que afecta a los tejidos profundos y superficiales de las regiones perineal, anal, escrotal y genital. A pesar de la evolución significativa en el conocimiento médico, se destaca una evidencia aún escasa en torno al plan de atención de enfermería en pacientes afectados por esta patología, lo que dificulta su manejo correcto. Por esta razón, se presenta el siguiente caso clínico de un paciente varón de 53 años de edad con gangrena de Fournier que ingresó en el servicio de urgencias por dolor de 3 días de evolución en zona perineal y fiebre.
ObjetivoEl objetivo fue el de establecer un plan de cuidados individualizado para el paciente detallando los diagnósticos, los resultados esperados y las intervenciones a través de taxonomías enfermeras.
Desarrollo del casoSe realizó una valoración sistemática tomando como referencia el modelo de patrones funcionales de salud de Marjory Gordon. Tras la elaboración de inferencias, se establecieron tres problemas de colaboración y dos diagnósticos de enfermería con sus criterios de resultado e intervenciones. Una vez ejecutado el plan, los resultados obtenidos destacaron que las intervenciones fueron consistentes para lograr los objetivos planteados en los problemas presentes en el paciente del caso.
ConclusionesEl desarrollo de un plan individualizado hizo posible detectar problemas, establecer objetivos realistas y definir intervenciones que optimizaron los cuidados de enfermería en este paciente con gangrena de Fournier.
Fournier’s gangrene, a relatively rare form of necrotizing fasciitis, is a rapidly progressive disease that affects the deep and superficial tissues of the perineal, anal, scrotal, and genital regions.1 The disease involves the rapid spread of severe inflammatory and infectious processes along fascial planes that affect adjacent soft tissues. Therefore, the disease may initially go unnoticed or not be recognized, since there may be minimal or non-existent skin manifestations in its initial phases.2
This is a rare infection, constituting <.02% of all hospital admissions and showing a strong predilection for men over women, with a ratio of 10 to 1.3 In recent years, an increase in the incidence of this type of fasciitis has been recorded, especially among older patients with predisposing factors such as diabetes, alcoholism, cancer and immunosuppression.4 The current therapeutic approach pivots between metabolic stabilisation, antibiotic therapy and a combined three-stage surgical approach (wound control, temporalisation and reconstruction).5 Despite notable advances in treatment, the morbidity and mortality of this pathology continues to remain at considerably high levels, underlining the imperative of early diagnosis for early and aggressive treatment.1 The implementation of effective nursing care forms a fundamental basis for optimising the desired results of patients suffering from this complex pathology.6
The nurse, as a key piece in the multidisciplinary care team, plays an indispensable role in the complete recovery of patients facing Fournier’s Gangrene. Despite the significant evolution in medical knowledge, there is still little evidence regarding the nursing care plan in patients affected by this pathology, which hinders correct management.7,8 For this reason, the following clinical case of a male patient with Fournier’s gangrene is presented in the clinical context of post-critical hospital care, specifically in the interim stage of the surgical wound.
AimThe objective of the study was to establish an individualised care plan for a patient with Fournier’s gangrene, detailing the diagnoses, expected results and interventions through nursing taxonomies.
Case descriptionA 53-year-old male patient with no known drug allergies and a history of Type II Diabetes Mellitus and smoking since he was 15 years old was admitted to the emergency department due to a three-day onset pain in the perineal area and fever. Upon admission to the emergency department he had BP 130/87, HR 96ppm, axillary temperature 37°C, Sat 02 98%. Analysis was performed and after physical examination cellulitis was observed in the perineum with areas of skin necrosis. After confirmation by imaging tests, Fournier’s gangrene was diagnosed, broad-spectrum antibiotic therapy (Piperacillin-tazobactam and Clindamycin) was administered and the gangrenous wound was debrided by perineo-scrotal approximation. A necrectomy was performed with surgical lavage and after primary control of the wound and clinical stabilisation of the patient in the Intensive Care Unit, a closed drainage system with negative pressure therapy was applied to prepare the wound for surgical reconstruction.
The patient was received in the surgical inpatient unit for monitoring and evolutionary control until reconstruction. Medical treatment included: broad-spectrum antibiotic therapy, fluid therapy, drainage control and monitoring of the patient’s general condition.
AssessmentA comprehensive nursing assessment was carried out through an interview, physical examination and data from the medical records and the nursing care plan of the previous unit based on Marjory Gordon’s conceptual model of functional health patterns.
The most relevant data from the pattern assessment is described below.
Pattern 1: health perception-managementNo known drug allergies. Smoker of 20 cigarettes/day since age 15. Non-insulin dependent type II diabetic for 45 years.
Pattern 2: nutritional-metabolicSize: 1.73m. Weight: 93kg. BMI: 31.1 (obesity). Temperature: 36.4°C.
No problems with food or liquid intake. Peripheral venous line port number 18 in the left upper extremity.
Surgical debridement performed on the perineum with a silver nitrate sponge connected to hermetic drainage with continuous negative pressure at 125mmHg. Wound diameter=10cm. System changes scheduled every 48–72h. Slight oedema in the debrided perineal region. Norton scale score: 17 (Low risk).
Pattern 3: eliminationCarrier of discharge colostomy due to perineal involvement, evacuates soft and formed stools. Carrier of urethral catheter type Foley No. 16, urine of clear colour without sediment.
Pattern 4: activity-exerciseBlood pressure upon admission to the ward: 123/68mmHg, Heart Rate: 81bpm, Respiratory rate: 21rpm, Saturation: 98% in room air.
Limited mobility, requires help for self-care due to the discomfort of the surgical process and therapeutic regimen. Without difficulties in changing position autonomously.
Pattern 5: sleep-restThe patient reports resting adequately.
Pattern 6: cognitive-perceptualConscious and oriented. He reports slight residual pain in the perineal area of up to 3 points out of 10 on a numerical verbal scale that he controls through prescribed analgesia.
Pattern 7: self-perception-self-conceptThe patient reports nervousness and concern about the pathological process to be faced.
Pattern 8: role-relationshipsAccompanied by his wife and daughter with whom he shares a family unit.
Pattern 9: sexuality-reproductionHe reports concern about possible consequences related to sexuality.
Pattern 10: coping-stress toleranceHe refers to the ability to recover from the situation.
Pattern 11: values-beliefsHe does not report having beliefs or value systems superior to himself.
After analysing the data collected, dysfunctional patterns were therefore identified.
Pattern 2: nutritional-metabolic: perineal surgical wound.
Pattern 4: activity-exercise: limited mobility due to pain.
Pattern 6: cognitive-perceptual: reports pain.
Pattern 7: self-perception-self-concept: expresses nervousness and concern regarding the evolution of the process.
DiagnosisAfter drawing up inferences, the care plan was prepared considering the activities that would be carried out interdependently, derived from the medical process, and the problems in which action would be taken independently.
Interdependent problems are presented through the PC (Potential Complication) contraction of the pathophysiological situation, medical treatment and diagnostic tests. In this case, they derived from the need for attention to the post-surgical stage of an infectious process such as Fournier’s gangrene.
PC: sepsis secondary to perineal infection.
PC: haemorrhage secondary to aggressive surgical debridement.
PC: thrombosis secondary to aggressive surgical intervention and immobility.
Meanwhile, nursing diagnoses were presented in PES format (Problem, Aetiology and Signs/Symptoms). The problem corresponds to the diagnostic label of the NANDA taxonomy. The aetiology is equivalent to the related factors or risk factors and the signs or symptoms are the defining characteristics that the patient manifests. The links used in the formulation correspond to “related to” (r/t) and “manifested by” (m/b) and efforts have been made to show the indications that have led to the diagnostic judgment.
Pattern 4: activity-exerciseNANDA [0085]: impaired physical mobility r/t pain m/b expression of discomfort.
Pattern 7: self-perception-self-conceptNANDA [00146]: anxiety r/t stressors m/b expression of worries.
PlanningAfter carrying out the diagnostic judgment, the therapeutic judgment was prepared for the collaboration problems and for the nursing diagnoses of the case through the use of the NOC and NIC9 taxonomies. Thus, objectives were established, identifying the nursing outcome criteria (NOC) with their indicators and the nursing interventions criteria (NIC) with their activities. To facilitate the interrelationships between the different taxonomies and develop the care plan, the NNN consult9 online platform was used.
A time limit was established for each of the indicators using the following names: CV (current value of the patient's state before the execution phase) and TV (desired value of the patient’s state in the final evaluation of the process). Thus, to measure the indicators, the 5-point Likert-type scale was used, with 1 being the least desirable score and 5 being the most desired.
Prior to developing the comprehensive care plan, the problems of the case were prioritised in order to ensure that the priority of care was directed to the most urgent ones. Tables 1–3 show the highest priority patient care issues, collaboration issues identified.
Potential complication: sepsis.
| PC: Sepsis secondary to perineal infection. | |
|---|---|
NOC [0703]: Severity of the infection.Indicators:
| NIC [6680]: Monitoring of vital signsActivities:
|
CV: Current value; TV: Target value; VA: Value achieved.
Likert a Scale Scores: (1) Severe, (2) Substantial, (3) Moderate, (4) Mild, (5) None.
Potential complication: bleeding.
| PC: Bleeding secondary to aggressive surgical debridement | |
|---|---|
NOC [1103]: Wound healing: by secondary intention.Indicators:
| NIC[3662]: Wound care: closed drainageActivities:
|
CV: Current value; TV: Target value; VA: Value achieved.
Likert a Scale Scores: (1) Extensive, (2) Substantial, (3) Moderate, (4) Scarce, (5) None.
Likert b Scale Scores: (1) Severely Compromised, (2) Substantially Compromised, (3) Moderately Compromised, (4) Mildly Compromised, (5) Not Compromised.
Potential complication: Thrombosis.
| PC: Thrombosis secondary to aggressive surgical intervention and immobility | |
|---|---|
NOC [1932]: Risk control: thrombi.Indicators:
| NIC [4110]: Precautions in embolismActivities:
|
CV: Current value; TV: Target value; VA: Value achieved.
Likert Scale Scores a: (1) Never demonstrated, (2) Rarely demonstrated, (3) Sometimes demonstrated, (4) Frequently demonstrated, (5) Always demonstrated.
Likert b Scale Scores: (1) Severe deviation from normal range, (2) Substantial deviation from normal range, (3) Moderate deviation from normal range, (4) Slight deviation from the normal range, (5) No deviation from the normal range.
Likert c Scale Scores: (1) Severe, (2) Substantial, (3) Moderate, (4) Mild, (5) None.
Meanwhile, Tables 4 and 5 show the nursing diagnoses established in detail, ordered according to Marjory Gordon’s functional health patterns.
Impairment of mobility.
| Domain 4: Activity/RestClase 2: Activity/exercise | |
|---|---|
| NANDA [0085]: Impairment of physical mobility r/t pain m/b expression of discomfort. | |
NOC [1605]: Pain control.Indicators:
| NIC [2210]: Administration of analgesics.Activities:
|
CV: Current value; TV: Target value; VA: Value achieved.
Likert a Scale Scores: (1) Never demonstrated, (2) Rarely demonstrated, (3) Sometimes demonstrated, (4) Frequently demonstrated, (5) Always demonstrated.
Likert b Scale Scores: (1) Severe, (2) Substantial, (3) Moderate, (4) Mild, (5) None.
Likert b Scale Scores: (1) Not at all satisfied, (2) Somewhat satisfied, (3) Moderately satisfied, (4) Very satisfied, (5) Completely satisfied.
Anxiety.
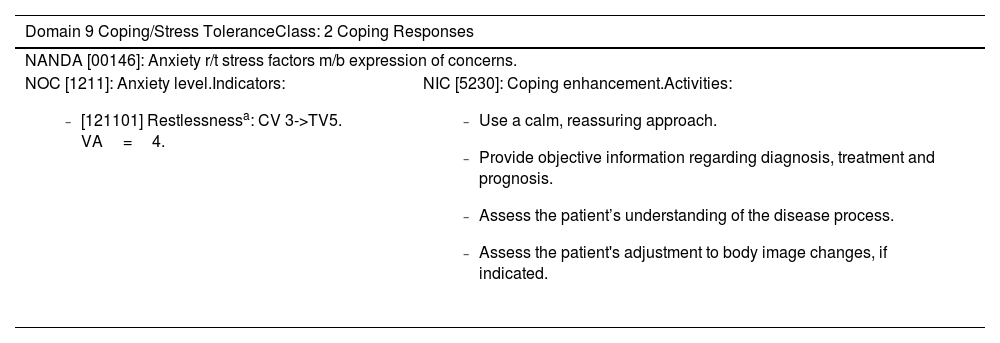
| Domain 9 Coping/Stress ToleranceClass: 2 Coping Responses | |
|---|---|
| NANDA [00146]: Anxiety r/t stress factors m/b expression of concerns. | |
NOC [1211]: Anxiety level.Indicators:
| NIC [5230]: Coping enhancement.Activities:
|
CV: Current value; TV: Target value; VA: Value achieved.
Likert Scale Scores a: (1) Severe, (2) Substantial, (3) Moderate, (4) Mild, (5) None.
During this phase, the nursing actions established for the patient were executed. In relation to the priority problem of the case. The main objective of the treatment plan was the debridement of the underlying necrotic tissue and the control of the bacterial load to prepare the area for reconstruction. To this end, changes of the vacuum drainage system were scheduled every 48–72h, washing of the wound with .9% physiological saline with mechanical debridement of non-viable tissue and irrigation and exposure for 5min with a polyhexanide-undecylenamidopropyl betaine solution.
When performing the first cure, 48h after the primary debridement in the operating theatre, the content of the drainage was approximately 70ml of serohaematic fluid with detrital remains. Upon removing the sponge, an exhaustive assessment of the characteristics of the wound was performed, which presented a rhomboidal appearance, with exposure of superficial perineal tissues and tunnelling towards deep tissues. Some necrotic remains were observed in the bed. The edges of the wound were hydrated, well defined and pink, while the perilesional skin was slightly swollen, with no signs of maceration or dryness.
The primary approach consisted of cleaning with .9% saline and mechanical debridement of non-viable tissue with gauze. Smegma accumulated in the glans was also removed using gauze and physiological saline to prevent possible complications. After applying the polyhexamide-undecylenamidopropyl betaine solution to the wound bed and drying it, a silver sponge was applied and concluded with a negative pressure therapy device. This same sequence was repeated during the two subsequent cures, which were performed on the fourth day and the seventh day of the primary surgical debridement.
After the first week, an almost complete reduction in exudate, a significant bacterial discharge and a considerable reduction in necrotic tissue and biofilm could be seen. The multidisciplinary team agreed to remove the vacuum drainage system and modify the dressing plan, scheduling dressings every 72h to prepare the wound for reconstruction. The approach consisted of cleaning the wound with saline solution plus application of silver hydrofibre dressing plus hydrocolloid dressing. After seven days of healing, a significant increase in granulation tissue was observed with a considerable reduction in the dimensions of the wound, free of necrotic tissue.
In summary, the evolution of the wound was satisfactory during this first stage of conceptualisation, so on the thirteenth day the patient was prepared for surgical reconstruction and re-admission to the unit to continue with the care process. One-time primary closure reconstruction was performed. Therefore, upon subsequent reception in the ward, the previously described plan was adapted, modifying the results and interventions related to the wound to its new characteristics. Specifically, NOC [1113]: Wound healing: by second intention was replaced by NOC [1102] Wound healing: by first intention. Consequently, NIC [3662]: Wound Care: Closed Drainage was also replaced by NIC [3660] Wound Care and Activities contained therein until the patient was discharged. Wound care included cleaning daily with .9% physiological saline, irrigation with 2% chlorhexidine and the application of a sterile dressing, in addition to pressure management measures in the area. No complications were recorded during first intention closure of the wound.
The patient was collaborative in his attitude during his care by the multidisciplinary team. He had support from his family throughout the care process, was able to verbalise his fears and adapted appropriately to the established plan.
AssessmentOnce he was discharged from the hospital, the care plan was assessed. To do this, the values achieved (VA) in each of the outcome criteria (NOC) were established. By comparing these values with the target values (TV) and those established at the time of admission to the unit (CV), the effectiveness of the plan could be determined.
The results obtained highlight that the nursing interventions carried out were consistent in achieving the proposed objectives for the problems present in the patient in this case.
DiscussionFournier’s gangrene is pathology of rare occurrence, little known and complex in approach. Isolated cases are reported in the literature, which somewhat limits the assessment of the various possible therapeutic approaches in relation to nursing care for this problem. In this case, late post-surgical care planning was carried out, although the role of nursing throughout the care process is essential to guarantee the control and full recovery of the patient.6
The first step in the care of Fournier’s gangrene consists of a meticulous assessment that includes the identification of risk factors, the extent of the infection, and the evaluation of the patient's general condition.1,3 To a large extent, assessment is mediated by the process’s rapid progression towards sepsis, organ dysfunction and death. Nurses should be alert to signs of deterioration and collaborate closely with the medical team to prioritise pain control, appropriate administration of antibiotics, and constant monitoring of vital signs. In this sense, interdisciplinary collaboration is essential to ensure a rapid and coordinated response.
Once the patient was stabilised, regarding the surgical setting, the primary debridement was aggressive until healthy tissue could be reached. Surveillance of the surgical wound is especially important, since a high percentage of patients require reintervention in the first 72h.5 The importance of good communication and the emotional support that nursing must provide to these patients and their families to reduce anxiety7 is also highlighted.
Thus, regarding the post-surgical care of Fournier’s gangrene, the role of nursing focused not only on the physical recovery of the patient, but also included the psychological and social sphere. The most technical care documented focused on the management of the postsurgical wound of this pathology, constituting a critical aspect of the care plan. The use of negative pressure drainage systems, such as the one in this case, has been shown to improve functional and aesthetic results after final wound closure.10
Finally, there is a need for correct coordination between primary care and the hospital setting for good follow-up, focused on recovering the quality of life that the patient had before the process. To this end, the importance of a continuity of care oriented towards health education, acceptance of the new body image and recovery of sexual and reproductive function is highlighted.
ConclusionsThe development of an individualised plan made it possible to detect problems, establish realistic objectives and define interventions that optimised nursing care in this patient with Fournier’s gangrene.
This clinical case highlights the need to continue studying, producing and disseminating care plans for rare pathologies that favour decision-making in clinical practice and that in turn serve as a frame of reference for similar cases.
Ethical considerationsPatient consent was obtained before sharing any information related to their case. All data presented in this context has been anonymised to safeguard patient privacy and confidentiality.
FundingFunding for open access publication was provided by the University of the Basque Country.
Conflicts of interestNone declared.
Availability of data and materialsData available upon request. The data on which this article is based will be shared upon reasonable request to the corresponding author.