To analyse whether adherence to non-pharmacological measures in the prevention of ventilator-associated pneumonia (VAP) is associated with nursing workload.
MethodsA prospective observational study performed in a single medical-surgical ICU. Nurses in charge of patients under ventilator support were assessed. Variables: knowledge questionnaire, application of non-pharmacological VAP prevention measures, and workload (Nine Equivalents of Nursing Manpower Use Score). Phases: 1) the nurses carried out a educational programme, consisting of 60-min lectures on non-pharmacological measures for VAP prevention, and at the end completed a questionnaire knowledge; 2) observation period; 3) knowledge questionnaire.
ResultsAmong 67 ICU-staff nurses, 54 completed the educational programme and were observed. A total of 160 observations of 49 nurses were made. Adequate knowledge was confirmed in both the initial and final questionnaires. Application of preventive measures ranged from 11% for hand washing pre-aspiration to 97% for the use of a sterile aspiration probe. The Nine Equivalents of Nursing Manpower Use Score was 50±13. No significant differences were observed between the association of the nurses’ knowledge and the application of preventive measures or between workload and the application of preventive measures.
ConclusionsNurses’ knowledge of VAP prevention measures is not necessarily applied in daily practice. Failure to follow these measures is not subject to lack of knowledge or to increased workload, but presumably to contextual factors.
Analizar si el cumplimiento de las medidas no farmacológicas para la prevención de la neumonía asociada a la ventilación mecánica (NAV) se asocia a la carga de trabajo de las enfermeras.
MétodoEstudio observacional prospectivo llevado a cabo en una UCI médico-quirúrgica. Se evaluó a las enfermeras a cargo de pacientes con soporte ventilatorio. Variables: cuestionario de conocimiento, aplicación de las medidas no farmacológicas de prevención de la NAV, carga de trabajo medida mediante el Nine Equivalents of Nursing Manpower Use Score. Fases: 1) las enfermeras realizaron un programa educativo, basado en conferencias de 60min sobre medidas no farmacológicas para la prevención de NAV, completando al finalizar un cuestionario de conocimiento; 2) periodo de observaciones; 3) cuestionario de conocimiento.
ResultadosDe un total de 67 enfermeras de UCI, 54 completaron el programa formativo y fueron incluidos en el estudio. Se llevaron a cabo un total de 160 observaciones de 49 enfermeros/as. El correcto conocimiento de las medidas de prevención se confirmó tanto en el cuestionario inicial como final. La aplicación de las medidas de prevención varió desde el 11% para el lavado de manos preaspiración hasta el 97% para el uso de sonda de aspiración estéril. La puntuación del Nine Equivalents of Nursing Manpower Use Score fue de 50±13. No se observaron asociaciones significativas entre el grado de conocimiento y la aplicación de medidas de prevención, ni entre la carga de trabajo y la aplicación de dichas medidas.
ConclusionesEl conocimiento de las enfermeras de las medidas de prevención de la NAV no se traslada necesariamente a la práctica diaria. En la población estudiada, la falta de aplicación de estas medidas no está sujeta a la falta de conocimiento ni a la carga de trabajo, sino probablemente a los factores contextuales.
Ventilator-associated pneumonia (VAP) is a serious adverse event and nurses play a fundamental role in its prevention as they are directly responsible for the application of preventive non-pharmacological measures. Nurses’ deficient compliance with guidelines to avoid VAP is partly attributable to their lack of knowledge and workload.
The present study shows that poor adherence to non-pharmacological measures to prevent VAP is not necessarily associated with nurses’ lack of knowledge or increased workload, but rather to contextual factors. While numerous published studies assess nurses’ workload based on the nurse-patient ratio, we used a specific scoring system. Likewise, the level of compliance with preventive measures was assessed by direct observation, unlike most studies that use self-administered questionnaires. This provides a more objective view of care practice.
Implications of the studyIn order to guarantee adequate adherence to non-pharmacological measures to prevent VAP, in addition to continuous training, strategies should be applied that take into consideration contextual factors such as professionals’ attitudes and behaviours.
Ventilator-associated pneumonia (VAP) is one of the most prevalent and serious adverse events (AE) in critically ill patients.1–3 Its occurrence is associated with increased mortality rates, prolonged Intensive Care Unit (ICU) and hospital length of stay, and increased healthcare costs.4,5 In developed countries, VAP incidence ranges from 1.2 to 38 episodes per 1000 days of mechanical ventilation3,6 and mortality rates vary from 24 to 50% or higher, depending on the main diagnosis or the presence of multi-resistant microorganisms.4,7 The variability observed in the incidence, and morbi-mortality might depend not only on the baseline characteristics of the patients, but also on the variations in the preventive measures applied in the different ICU.4,8,9
Considering that VAP is a serious AE that can be prevented to some extent, clinical practice guidelines and recommendations have been proposed taking into account both pharmacological preventive measures (PPMs) and non-pharmacological preventive measures (NPPMs).9,10 Recently, in Spain, a national programme aimed at decreasing nosocomial pneumonia has been launched: the “Zero-VAP (ZV)” project.11 The purpose of the project is to apply a package of specific measures for NAV prevention, including PPMs and NPPMs. The project has been endorsed by the Spanish Health Ministry (Agencia de Calidad del Ministerio de Sanidad, MSSSI), and lead by the Spanish Societies of Critical Care Medicine (Sociedad Española de Medicina Intensiva Crítica y Unidades Coronarias – SEMICYUC –, and Sociedad Española de Enfermería Intensiva y Unidades coronarias – SEEIUC).
Since nurses are directly responsible for applying most of the NPPMs, their role in the VAP-prevention process is fundamental, and therefore, nursing care has a direct impact on patients’ safety. Although nurses have adequate knowledge on VAP prevention measures, there is an unequal adherence in the application of these measures. Indeed, various surveys carried out in different ICUs confirm a limited compliance,12–14 and show that the knowledge, availability and diffusion of evidence-based guidelines do not ensure their adherence. Some factors might influence the lack of application of the recommendations for VAP prevention by the nursing staff: insufficient knowledge of the recommendations made by Scientific Associations, aspects related to practical competence linked to a healthcare activity more based on routine than on evidence, lack of motivation, work overload, and conditions regarding the system and working environment.14–17
Multiple studies have already shown that increasing nurses’ knowledge by means of educational programmes is associated with reductions in the incidence of VAP.17–19 However, some authors have noted that although educational programmes might increase nurses’ knowledge, their adherence to the recommended strategies might be uneven.20 Several groups have showed that there is a discrepancy between knowledge and clinical practice, and the application of the recommendations is far below the actual knowledge.21,22
It should be noted that the evaluation of the knowledge that nurses have on NPPMs and how they apply it in clinical practice has mainly been assessed using self-administered questionnaires, and the results might therefore have suffered an overestimation bias.13,23 Consequently, it is important to consider the direct observation of daily care to assess the real application of NPPMs in clinical practice.
Furthermore, workload is frequently cited as a potential risk factor for the lack of adherence to the recommendations, which might entail the appearance of AE, such as nosocomial infections, among others.24,25 However, most studies analyse the incidence of AE and/or the application of recommendations according to different nurse staffing levels, mainly determined by the nurse-to-patient ratio, and few authors examine it directly measuring the workload of the nurse by means of specific scores.26
The present study was designed to analyse whether workload is significant factor that affect the application of NPPMs for VAP prevention in nursing daily practice.
MethodsDesignA prospective observational study carried out in an adult medical-surgical ICU of 16 beds with a nurse/patient ratio of 1:2, at a university hospital (Hospital Parc Taulí, Sabadell, Barcelona, Spain).
Study populationAll the staff nurses of the ICU (n=67) were eligible to enter the study. Inclusion criteria: being in charge of patients receiving any form of MV and/or spontaneously breathing with artificial airway (endotracheal tube or tracheotomy). Exclusion criteria: not belonging to the usual ICU staff (nurses who sporadically work in the ICU), not having completed the educational programme, or belonging to the research team.
Study phasesThe study was carried out from September 2013 to July 2014.
First phase (training phase—4 months)During this phase, ICU nurses completed an educational programme consisting of 60-min lectures on non-pharmacological measures for VAP prevention. The content of the lectures was adapted from the “Zero-VAP” project,11 and were given by 1 critical care physician and 4 critical care nurses members of the research team, along with 2 nurses from the department of nosocomial infection control and prevention of the same hospital.
Lectures were given during working hours, at different times, to ensure maximum attendance, and all participating nurses were exempted of clinical duties during the lectures. At the end of the educational programme, the nurses completed a questionnaire on VAP prevention. A code was assigned to each nurse and questionnaire.
In addition, during this phase, information posters on NPPMs for VAP prevention were placed in each ICU box.
Second phase (observation phase—6 months)After completing the educational programme, the research team monitored NPPMs fulfilment during a 6-month period. The ICU nurses were not informed of this observation phase, and nurses were not aware of who the observers were.
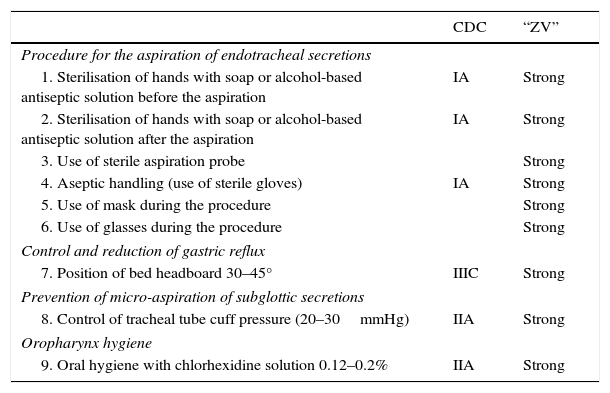
NPPMs application was specifically examined by means of 9 procedures (Table 1). Each nurse and each patient could be observed on more than one occasion. A data collection sheet was designed, where the selected NPPMs for VAP prevention were listed. The measured interventions were chosen in accordance with the grade of recommendation10 of the Spanish Zero-VAP project.11 A total of 6 nurses from the research team were responsible of performing the observations, and were previously trained in order to systematically fulfil the collection sheet.
Non-pharmacological measures for VAP prevention (NPPMs). The nine NPPMs procedures evaluated are listed. The grade of recommendation, according to the 2003 recommendations of the CDC and the Healthcare Infection Control Practices Advisory Committee,10 and according to the “Zero-VAP” project11 are also shown.
| CDC | “ZV” | |
|---|---|---|
| Procedure for the aspiration of endotracheal secretions | ||
| 1. Sterilisation of hands with soap or alcohol-based antiseptic solution before the aspiration | IA | Strong |
| 2. Sterilisation of hands with soap or alcohol-based antiseptic solution after the aspiration | IA | Strong |
| 3. Use of sterile aspiration probe | Strong | |
| 4. Aseptic handling (use of sterile gloves) | IA | Strong |
| 5. Use of mask during the procedure | Strong | |
| 6. Use of glasses during the procedure | Strong | |
| Control and reduction of gastric reflux | ||
| 7. Position of bed headboard 30–45° | IIIC | Strong |
| Prevention of micro-aspiration of subglottic secretions | ||
| 8. Control of tracheal tube cuff pressure (20–30mmHg) | IIA | Strong |
| Oropharynx hygiene | ||
| 9. Oral hygiene with chlorhexidine solution 0.12–0.2% | IIA | Strong |
At the end of Phase two, the same questionnaire was administered again to assess whether knowledge was maintained over time. The studied nurses had 7 days to collect, and complete the second questionnaire. Once completed, the questionnaire was assigned the same code for the nurse as in phase 1, in order to ensure a blind evaluation by the research team.
Measured variables- 1.
Knowledge questionnaire. The questionnaire consisted of 6 questions about NPPMs. Each question had a binary answer, each correct answer was given 1 point, and the maximum score was 6. The questionnaire was based on the already existing evaluation module of the Zero-VAP project, and we selected the questions considered to be more relevant in nurse clinical practice11
- 2.
Non-pharmacological prevention measures. A total of 9 NPPMs were assessed (Table 1).
- •
Endotracheal secretion aspiration procedure. The time for observation was 45min per nursing shift. If in this period of time, the observed nurse did not carry out the procedure, the observation was rescheduled until it was obtained.
- •
The degree of inclination of the headboard was checked through direct observation using the degree indicator system included in the ICU beds (model Hill-Rom TotalCare® P500 Surface).
- •
Compliance with the other NPPMs was assessed by examining the clinical records at the end of each nursing shift.
- •
- 3.
Workload. The average of the Nine Equivalents of Nursing Manpower Use Score (NEMS)27 of the patients corresponding to the observed nurse was calculated. This score is determined using nine items related to the effort of the nursing staff required by critically ill patients. The value of the NEMS was structured into 3 different levels, as previously described by Moreno and Miranda28: a) Level 1 (light workload): NEMS<21; b) Level 2 (moderate workload): NEMS 21–30; and c) Level 3 (intense workload): NEMS>30.
The SPSS V18 package was used for statistical analysis. A descriptive analysis was performed. Quantitative variables are presented as mean±standard deviation, and qualitative variables as absolute and relative frequencies. Comparisons between the different categories of NEMS were made using the Kruskal–Wallis test.
A logistic regression model was used for repeated measurements (multi-level or hierarchical). The aggregation unit was the observed nurse; the explicative variable was the level of workload, and the response variable was the percentage of correct actions. Statistical significance was set at <0.05.
Ethics approvalThe study was approved by the Local Clinical Research Ethics Committee (Comitè Ètic d’Investigació Clínica (CEIC). Reference number 2014622). Waived consent was also approved, due to the observational and blind nature of the study. Clinical records handling was made in accordance with the Organic Law 15/1999 on Personal Data Protection. The study was conducted in accordance with the Declaration of Helsinki.
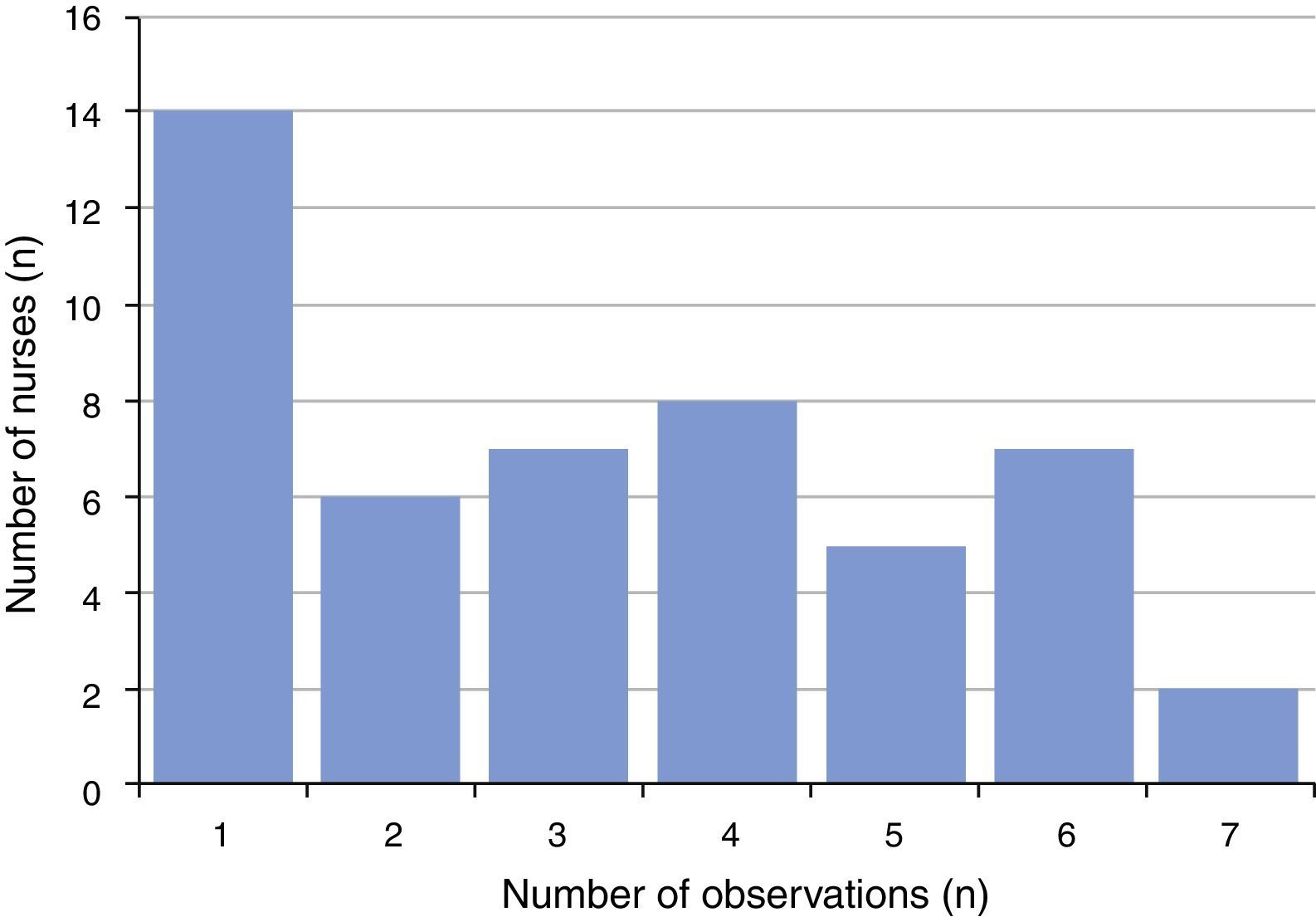
ResultsAmong the 67 nurses of the ICU staff, 54 (81%) completed the educational programme on NPPMs for VAP, and were observed. A total of 160 observations from 49 nurses were made. The five remaining nurses did not carry out any endotracheal secretion aspiration during the assigned observation periods, and therefore were not included in the analysis. Fig. 1 shows the distribution of these observations among the nurses included in the analysis. The observations were made during the three nursing shifts, either in labour days and in the weekend.
Mean age of the nurses observed was 39±8 years (25–57), with 13±7 years (1–25) of ICU experience, and 42 were females (86%). Among the nurses studied, 17 (37%) worked during the morning shift (from 7:00h to 14:00h), 18 (39%) during the afternoon shift (from 14:00h to 21:00h), and 11 (24%) during the night shift (from 21:00h to 7:00h).
Regarding knowledge of NPPMs, the score obtained in the questionnaire administered in Phase 1 was 5.73±0.49, and the score once Phase 2 was completed was 5.64±0.50 (p=0.471; Table 2).
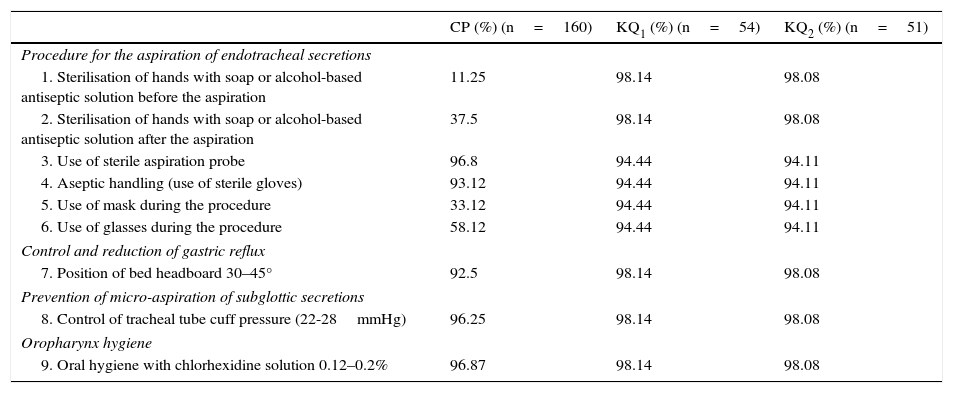
Practical compliance and theoretical knowledge of the non-pharmacological preventative measures for VAP.
| CP (%) (n=160) | KQ1 (%) (n=54) | KQ2 (%) (n=51) | |
|---|---|---|---|
| Procedure for the aspiration of endotracheal secretions | |||
| 1. Sterilisation of hands with soap or alcohol-based antiseptic solution before the aspiration | 11.25 | 98.14 | 98.08 |
| 2. Sterilisation of hands with soap or alcohol-based antiseptic solution after the aspiration | 37.5 | 98.14 | 98.08 |
| 3. Use of sterile aspiration probe | 96.8 | 94.44 | 94.11 |
| 4. Aseptic handling (use of sterile gloves) | 93.12 | 94.44 | 94.11 |
| 5. Use of mask during the procedure | 33.12 | 94.44 | 94.11 |
| 6. Use of glasses during the procedure | 58.12 | 94.44 | 94.11 |
| Control and reduction of gastric reflux | |||
| 7. Position of bed headboard 30–45° | 92.5 | 98.14 | 98.08 |
| Prevention of micro-aspiration of subglottic secretions | |||
| 8. Control of tracheal tube cuff pressure (22-28mmHg) | 96.25 | 98.14 | 98.08 |
| Oropharynx hygiene | |||
| 9. Oral hygiene with chlorhexidine solution 0.12–0.2% | 96.87 | 98.14 | 98.08 |
CP, compliance during clinical practice of the non-pharmacological preventive measures for VAP; KQ1, 1st knowledge questionnaire (Phase 1); KQ2, 2nd knowledge questionnaire (Phase 3).
The application of NPPMs is described in Table 2. Overall compliance with NPPMs was 77±17%, although compliance with the measures was extremely variable, ranging from 11% for hand washing previous to secretion aspiration to 97% for other procedures such as use of sterile aspiration probe or oral hygiene with chlorhexidine solution.
When evaluating the possible association between knowledge and the application of NPPMs by a logistic regression model, the results showed no statistically significant relationship (p=0.7).
WorkloadThe observed NEMS score was 50±13. When exploring the categories of workload, the representativeness of each level was 2.5% (n=4) for level I (NEMS<21); 9.4% (n=15) for level II (NEMS 21–30); and 88% (n=141) for level III (NEMS>30). No differences in compliance with NPPMs were observed among the three categories of NEMS (p=0.8).
The logistic regression model exploring the relationship between the workload of the nurse (determined using the three pre-defined levels in the NEMS score) and the application of NPPMs showed no statistically significant associations (p=0.7).
DiscussionIn addition to confirming that educational programmes alone are not enough to ensure the application of NPPMs for VAP prevention, the main result of the present study is the observation that the application of such measures does not depend on the workload of the nurse in charge of the patient.
Although an educational programme was designed to further strengthen the knowledge on NPPMs to prevent VAP, as demonstrated by the two knowledge questionnaires used in the study, it did not ensure an adequate level of NPPMs application in clinical practice. This fact has already been reflected in some studies that show that knowledge of the guidelines does not ensure adherence to the recommended strategies.4,21,22 Furthermore, some studies have shown that carrying out training activities that might improve knowledge does not imply a sufficient change in the skills, attitudes and behaviours of professionals.20,29 On that behalf, several authors have stated that the nurses’ attitude is of vital importance for the application of the guidelines on VAP prevention measures.30–32 In fact, our data further reinforces the idea that some factors other than knowledge and even workload might be responsible for the inadequate application of NPPMs.
Although our study failed to find any relationship between workload and the application of NPPMs for VAP, some other studies did relate nursing staff levels with the incidence of VAP, observing a trend between a higher level of nursing staff and reductions in VAP incidence.15,24 However, these studies evaluated nursing workload from a general point of view, using the nurse staffing level, but did not make an individual evaluation of the actual workload the nurse in charge of the patient had, as we did. To our knowledge, no previous publications have linked workload, measured by the NEMS scale, with the application of NPPMs. Daud-Gallotti et al.26 assessed the workload of the nursing staff, using the Nursing Activities Score (NAS),33 and suggested it could be a risk factor for the appearance of AE, although they did not analyse the application of NPPMs for VAP specifically. At any rate, the results obtained in this study are backed by other studies that establish that workload (patient/nurse ratio) does not appear to be related to the AE or to the perception of patient safety.34 McGahan et al.35 reviewed the published literature examining the relationship between nurse staffing levels and AE incidence, and no association was detected.
The fact that no relationship has been found between workload and the lack of application of NPPMs reinforces the idea that other aspects influence nursing clinical practice, such as emotional exhaustion or job dissatisfaction, among others, as already suggested by some authors.34,35
Overall compliance with NPPMs for VAP preventionIndependently from adequate knowledge and workload, compliance with NPPMs in our study was very similar to that reported in the literature.
In our study, the measure with the lowest compliance was hand washing in the procedure for handling the airway for endotracheal secretion aspirations, with the frequency of post-procedure compliance higher than pre-procedure. These data were lower than those reported by other studies where 33.3% is shown for compliance of pre-procedure aspiration,18 although it is line with other publications that report that hand washing frequency by healthcare staff is low, with a suboptimal adherence.36–38
The introduction of alcohol-based solutions is the measure that has most significantly improved adherence to recommendations on hand washing, as it allows a faster and safer disinfection.39 In the case at hand, all the ICU boxes had hand washing basins, soap and paper towels, as well as alcohol-based solutions, which should have led to a higher degree of compliance. Although the procedure is simple, its application is a complex phenomenon that seems difficult to change.30,37,40,41
For the NPPMs regarding the use of the sterile probe and aseptic handling (use of sterile gloves) a high degree of application was obtained, similar to in other studies.42
In relation to the use of glasses and masks, the results obtained in the present study were lower than those reported by other authors studies.42 This may due to the fact that these two measures were more recently introduced in the ICU and accordingly are not integrated in practice.
Nurses’ adherence to maintaining the headboard between 30 and 45°, analysed by cross section observations, was high, in concordance with other studies,18 which is in line with the level of knowledge of the studied nurses. Records of oral hygiene care and tracheal tube cuff pressure had a high compliance, also in accordance with other publications.18,43
Regarding the control of tracheal tube cuff pressure, the pressure levels recorded in all cases were between the recommended values of 20–30cmH2.11 Other authors observed that 20% of tracheal tube cuff pressures measured every 6h were below 20cmH2O, while those that were measured every 8h were 33.7%.43,44 In this study, tracheal tube cuff pressure was checked every 4h, which might have favoured maintaining adequate pressure levels, especially if we consider that tracheal tube cuff pressure starts to lose pressure after 4–5h.45
Overall, the observed application of NPPMs in our studied population does not differ from that described in the literature, suggesting that our ICU nursing staff might be a good reflection of other ICUs. However, multicentre studies would be desirable in order to confirm our results and further analyse contextual and behavioural factors associated to NPPMs compliance, contributing to ensure a more effective implementation of the guidelines and protocols in clinical practice.
Study limitationsAlthough according to the design of the present study, the nurses were blinded to the fact that an observational study was being carried out, the recent educational programme and the presence of research nurses might have changed the ICU nurses’ habitual practices, thereby bringing about a bias known as the Hawthorne effect. This effect modifies the behaviour at a subconscious level, but may cause a positive effect, as better results may be obtained simply by the fact that nurses know they are being observed. However, the negative results regarding compliance with NPPMs suggest that this effect has not occurred in the present study.
Secondly, since this is a single-centre study, the results obtained may only be extrapolated to ICUs of similar characteristics, with the same nurse/patient ratio, and with similar workloads.
Finally, the design of our study does not enable to determine any cause and effect relationship, but rather the possible relationship between the variables of the study. However, the lack of association between workload and the application of NPPMs would exclude workload as a cause of inadequate compliance with VAP prevention guidelines.
ConclusionsNurses are more aware of the prevention measures for VAP than they actually apply in practice. Failure to follow these measures is not subject to a lack of knowledge or to increased workload, but presumably to contextual factors.
The results of this study, whereby non-compliance to NPPMs is not subject to the degree of knowledge or to the workload of the nursing staff, suggests that new interventions should be focused on modifying the attitude of professionals. This provides the impetus for future multicentre studies to be carried out in order to analyse the contextual factors related to the adherence of the NPPMs.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Financial supportThis study was supported by a local research grant.
We wish to thank the Head of the Nursing Medical Department of the Intensive Care Unit, for her support and promotion of nursing research and all the nurses of the Intensive Care Unit for their collaboration and help which made this study possible. The authors also thank Sylva Astrik Torossian for her support to the manuscript edition and translation.
Please cite this article as: Jam R, Hernández O, Mesquida J, Turégano C, Carrillo E, Pedragosa R, et al. Carga de trabajo y cumplimiento por parte de las enfermeras de las medidas no farmacológicas para la prevención de la neumonía asociada a la ventilación mecánica. Estudio piloto. Enferm Intensiva. 2017;28:178–186.