Patients’ sleep can be disturbed during their stay in an Intensive Care Unit. Many factors can explain this disturbance, both within the ICU environment and caused by patients’ illnesses. There is evidence that patients’ sleep can be improved within ICUs. The aim of this study is to describe patients’ perceptions of a night's sleep and develop a care plan that promotes a night's sleep.
MethodologyA prospective descriptive study was performed in the ICU of a training hospital. The sleep of 125 patients was explored. Sociodemographic and clinical variables were collected from patients’ medical records. The 5-item Richards–Campbell Sleep Questionnaire was utilised to assess patients’ perception of a night's sleep. In addition, an ad-hoc 9-item questionnaire was developed which included factors that can affect sleep according to the literature. Patients had to grade the level of interference of those factors with their night's sleep.
ResultsThe sleep of patients in our Intensive Care Unit was moderately deep, with light arousals and ease in falling sleep again. The average value on the Richards–Campbell Sleep Questionnaire was 52.92mm. The factors that significantly interfered with sleep were: pain (p=.009), worries/anxiety (p=.01), staff voices (p=.033), alarm/medical devices sounds (p=.047) and peripheral intravenous lines (p=.036).
ConclusionsOur patients’ perception of a night's sleep in the ICU was fair. Optimising pain management, answering questions or worries, minimising background noise and voices have the potential to improve sleep quality.
El descanso nocturno de los pacientes ingresados en una Unidad de Cuidados Intensivos puede sufrir interrupciones debido a los múltiples factores presentes en este tipo de unidades, además de las ligadas al propio proceso de enfermedad. Hay evidencia de que el sueño en estas unidades puede mejorar.
El objetivo de este trabajo fue describir las percepciones de los pacientes con relación al sueño nocturno.
MetodologíaEstudio descriptivo prospectivo en una Unidad de Cuidados Intensivos de un hospital universitario de nivel terciario. Se estudió el sueño en 125 pacientes. Se recogieron variables sociodemográficas y datos de la historia clínica. Se utilizó el cuestionario del sueño de Richards-Campbell de 5ítems para valorar la percepción del sueño. Además, se añadió un cuestionario con 9 preguntas sobre factores descritos en la literatura que pueden influir en el sueño para que el paciente graduase la influencia de los mismos.
ResultadosEl patrón de sueño/descanso de los pacientes ingresados en nuestra unidad se caracterizó por ser un sueño de profundidad media, con ligeros despertares, y con facilidad para conciliarlo. El valor medio de la escala de sueño de Richards-Campbell fue de 52,92mm. Los factores que significativamente influyeron en el sueño fueron: el dolor (p=0,009), la preocupación/nerviosismo (p=0,01), las voces del personal (p=0,033), los ruidos de los monitores/alarmas/aparatos (p=0,047) y la vía periférica (p=0,036).
ConclusiónLa percepción del sueño nocturno de nuestros pacientes fue regular. Optimizar la pauta de analgesia, aclarar cualquier duda o preocupación, minimizar el ruido ambiental y el generado por las voces del personal, podría mejorar la calidad del sueño.
The aim of this study was to establish the quality of sleep of patients in our Intensive Care Unit and factors that could be changed. An awareness of the factors that affect sleep will determine the care required to improve its quality.
Sleep is a basic need and is commonly affected in intensive care units, in terms of both quantity and quality. It is characterised as being of poor quality, fragmented, with increased light sleep periods (stage 1 N-REM), reduced deep sleep periods (stage 3 and 4 N-REM) and the REM period, with increased awakenings and frequent interruptions. All of this leads to sleep in intensive care units not being restful. There are many studies that cover the extrinsic and intrinsic factors that affect sleep disturbance, some of which can be improved.
Implications of the studyThis study enabled us to establish the factors that are most significant for our patients with the aim of acting on them. Identifying the main factors that disturb and impede patients’ sleep is the first step towards applying corrective measures, which according to our results should be: explaining the need for and purpose of catheters and for their early removal, optimising analgesic regimens, informing the patient of continuous monitoring and answering all queries and concerns, lowering the level of alarms, and disconnecting those that are not strictly necessary, offering earplugs, closing cubicle doors and ensuring that night staff lower their voices.
A knowledge of the causes for our patients’ sleep being disrupted and how to help their care will enable us to examine in depth the importance of this basic need and its impact on the critical patient. This requires awareness-raising and training among multidisciplinary teams.
Sleep is a basic need for health and recovery from disease, and is considered an essential aspect in the body's physical and psychological recovery.1–3 It has 3 fundamental functions: restorative, protective and the functional reorganisation of the neuronal circuits.4
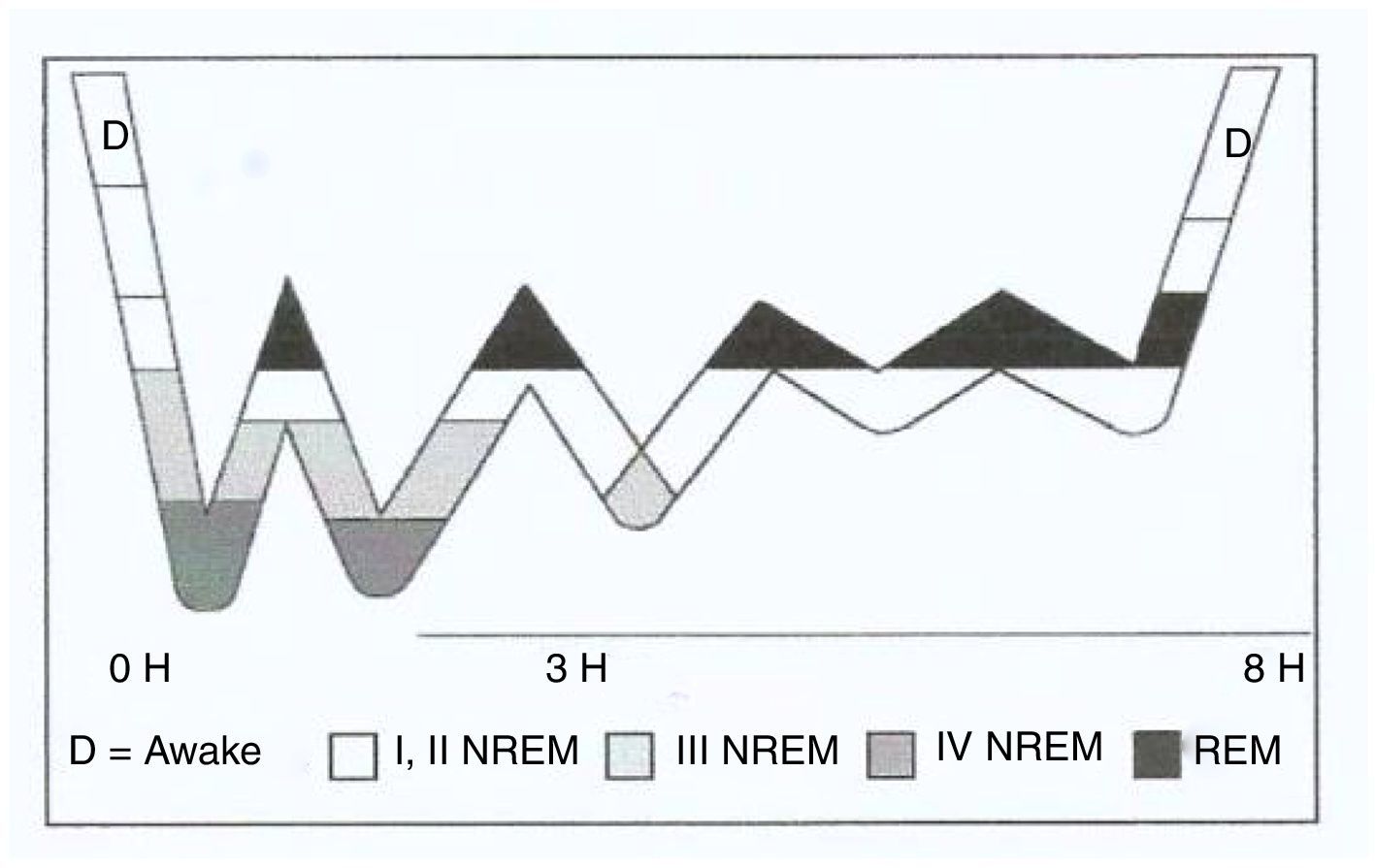
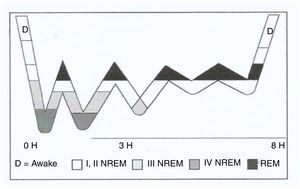
Physiologically, there are two different sleep phases: REM or active sleep, usually 20% of all sleep, and NREM or quiet sleep, the remaining 80%. NREM sleep has 4 stages5–8:
- –
Stage 1: transition between wakefulness and sleep (light sleep).
- –
Stage 2: start of the unequivocal stage of sleep, characterised by an increase in the arousal threshold (intermediate phase).
- –
Stages 3 and 4: deep sleep.
Sleep onset commences in stage 1 NREM until reaching stage 4, it returns to stage 3 and then to stage 2, and subsequently enters REM sleep. This cycle lasts approximately 90min and is repeated twice consecutively; stages 4 and 3 NREM gradually disappear, while the REM period increases (Fig. 1). From 4 to 6 cycles can occur during a disturbed night's sleep of 8h. If the person progresses through all the sleep stages, they are considered to have had a “good sleep”.9
Adult sleep hypnogram.
Source: Nicolás et al.9
We know that peripheral vascular tone is reduced during sleep as well as most of the vegetative functions, thus lowering BP, respiratory rate and baseline metabolism by 10% and 30%, which are crucial in the process of monitoring the critical patient and their recovery.4 Poor quality of sleep is associated with alterations in immunological function, can lead to confusion, reduced energy levels and alters cognitive, respiratory, cardiac and endocrine functions.1,10–12 Moreover, it causes diminished or altered attention span, reduced psychomotor performance, mood change, daytime sleepiness, fatigue, restlessness, disorientation and irritability.7
The need for sleep is a major problem in patients admitted to critical care units. Environmental or extrinsic factors can cause sleep disturbance such as noise (alarms, telephones, conversations), interventions by staff (hourly nursing activities including at night) and environmental light that makes it difficult to distinguish day from night, which causes circadian rhythm dysregulation. Intrinsic factors, such as pain, discomfort and worry,3,10,13–17 can also disrupt sleep.
Sleep in the Intensive Care Unit (ICU) is characterised as being of poor quality, fragmented, with increased light sleep (stage 1 NREM), reduced periods of deep sleep (stage 3 and 4 NREM) and reduced REM period, with an increase in arousals and frequent interruptions.2,8–10,15,16,18 All of which result in sleep that is not restful.
The high prevalence of disordered sleep in ICU has led to the development of instruments to diagnose these types of problems. We can make a distinction between the objective and the subjective assessment of sleep. Polysomnography and actigraphy are part of the objective assessment; however, they are very costly techniques and require trained personnel who are qualified to interpret the results. And then there is the subjective assessment of the night nurse recorded daily in the care plan, and that of the patient him/herself using scales such as the Richards–Campbell sleep scale, that measures patients’ perception of how they slept.19
It is important to be aware of the factors that interrupt sleep and help to reduce them. Therefore, as healthcare professionals we must facilitate and improve patients’ quality of life and amount of sleep to promote their wellbeing.
ObjectiveTo describe the perception of patients admitted to the ICU of a night's sleep.
MethodologyThis descriptive prospective and observational study was performed in a polyvalent 12-bedded ICU, where 1000–1200 patients are admitted annually, around 80% of whom are surgical. The types of surgery that most frequently result in admission to the unit are: cardiac and vascular, abdominal, thoracic and neurosurgical. This ICU belongs to a private, tertiary level university hospital with 300 beds. The study was performed between November 2016 and February 2017.
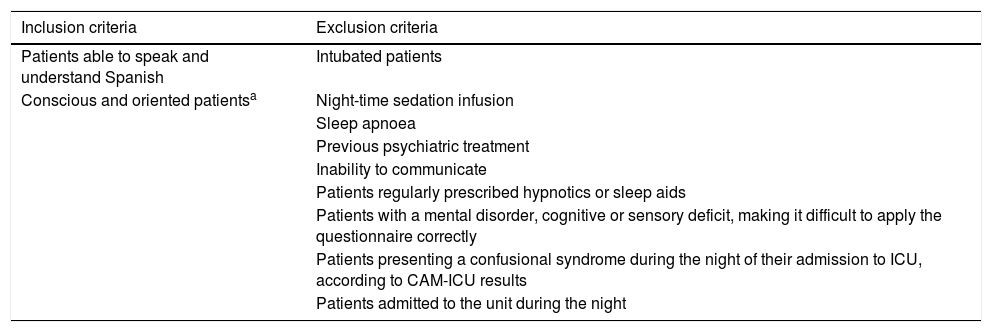
The convenience sample comprised 125 patients. The inclusion and exclusion criteria for selecting the sample are shown in Table 1.
Inclusion and exclusion criteria.
| Inclusion criteria | Exclusion criteria |
|---|---|
| Patients able to speak and understand Spanish | Intubated patients |
| Conscious and oriented patientsa | Night-time sedation infusion |
| Sleep apnoea | |
| Previous psychiatric treatment | |
| Inability to communicate | |
| Patients regularly prescribed hypnotics or sleep aids | |
| Patients with a mental disorder, cognitive or sensory deficit, making it difficult to apply the questionnaire correctly | |
| Patients presenting a confusional syndrome during the night of their admission to ICU, according to CAM-ICU results | |
| Patients admitted to the unit during the night |
CAM-ICU: Confusion Assessment Method for the Intensive Care Unit; ICU: Intensive Care Unit.
The period of night's sleep was considered to be from 23h to 7h the following morning. This time was determined because all the patients had care, such as respiratory physiotherapy, measures to ensure their comfort and wellbeing, etc. scheduled at 22h.
The unit comprises 12 beds in individual glass cubicles with automatic doors and windows to the outside that provide natural light during the day, fluorescent lighting is used when there is insufficient natural light and in the other areas of the unit. There are open visiting times for the family (from 11h to 14h and from 17h to 21h) and 24-h telephone contact.
Instruments used for data collectionThe research team prepared a document with 3 sections:
- 1.
Data on the patient's clinical history and computerised care plan.
- •
Age, sex, days of ICU stay, reason for admission.
- •
Presence of catheters, drains, tubes, oxygen therapy, wounds, pneumatic compression stockings, immobilisation systems, continuous dialysis, circulatory assistance (intra-aortic balloon counter-pulsation, extracorporeal membrane oxygenation), tracheostomy (suctioning of secretions).
- •
Care provided during the night, either scheduled or requested by the patient, and its frequency. The care recorded was: position changes, care of wounds, ulcers and drains, non-invasive blood pressure measurements, capillary glucose readings, nasogastric tube or urinary catheter placement and vascular cannulation.
- •
Night-time medication (sleeping aids, hypnotic agents and muscle relaxants that were not administered by continuous infusion, to prevent response biases, and analgesics of all types).
- •
- 2.
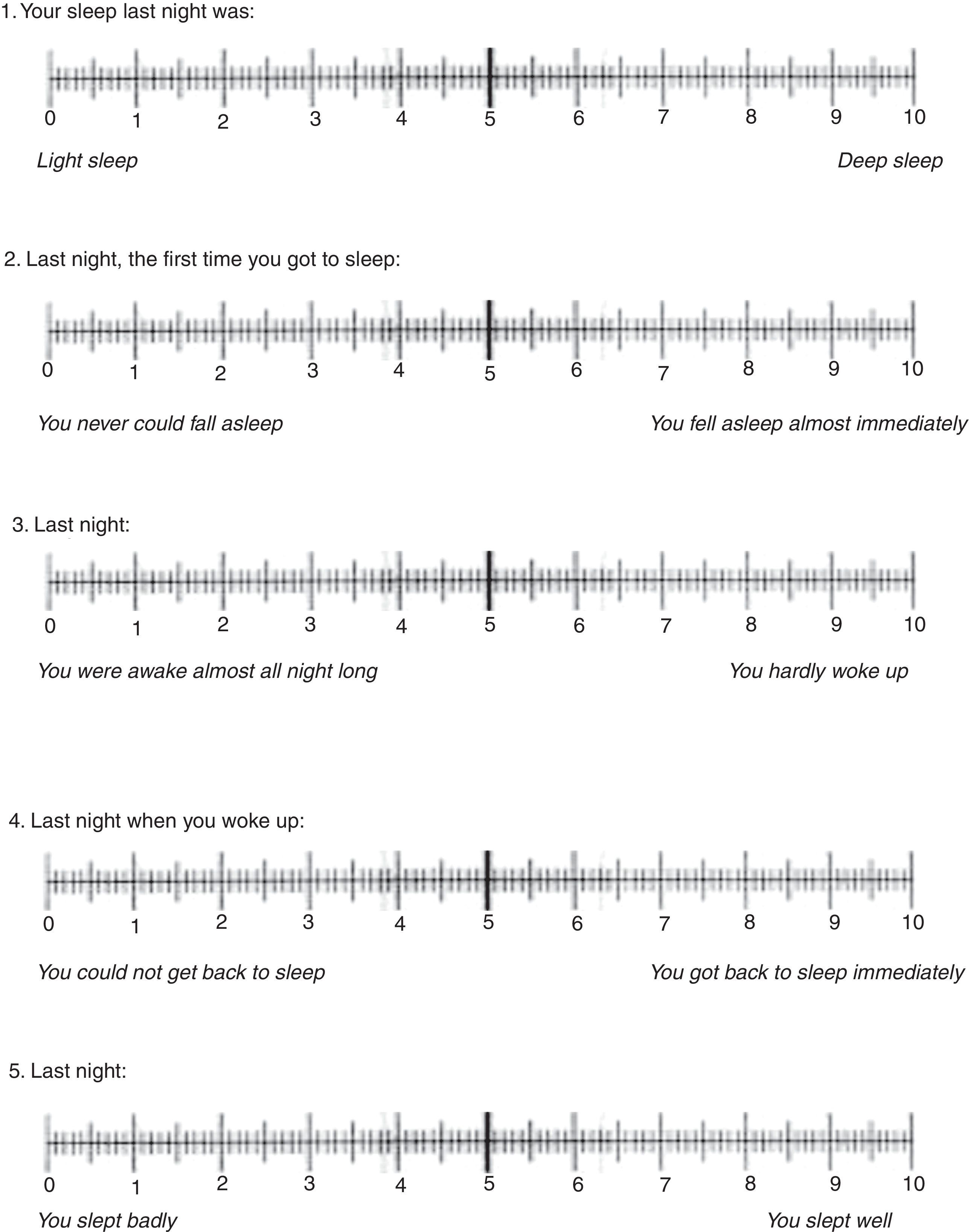
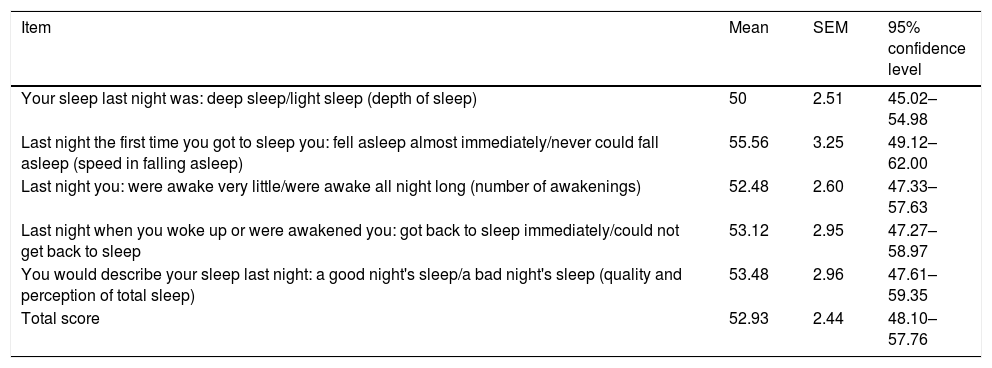
Richards–Campbell Sleep Questionnaire (RCSQ) translated into Spanish9 to learn the patients’ subjective perception of sleep (Fig. 2). The questionnaire contains 5 items constructed on a visual analogue scale. Each of the 5 items of the questionnaire examines an area of sleep of the 5 that are shown on the polysomnography studies (depth, falling asleep, number of awakenings, percentage of time awake and quality and perception of total sleep). The patient gives the scores for each item on a 100mm graduated scale, ranging from 0mm (poor sleep) to 100mm (excellent quality). The total score of the scale is calculated by dividing the sum of the item scores by 5.
This is a validated test with high reliability and internal validity (a Cranach alpha of .90 for both calculations), as the test's author's highlight.19 Its applicability has been proven in the intensive care population, and its usefulness demonstrated.9,19
Like other authors,9,20 we considered that sleep was poor if the patients obtained scores between 0mm and 33mm, fair from 34mm to 66mm and good from 67mm to 100mm.
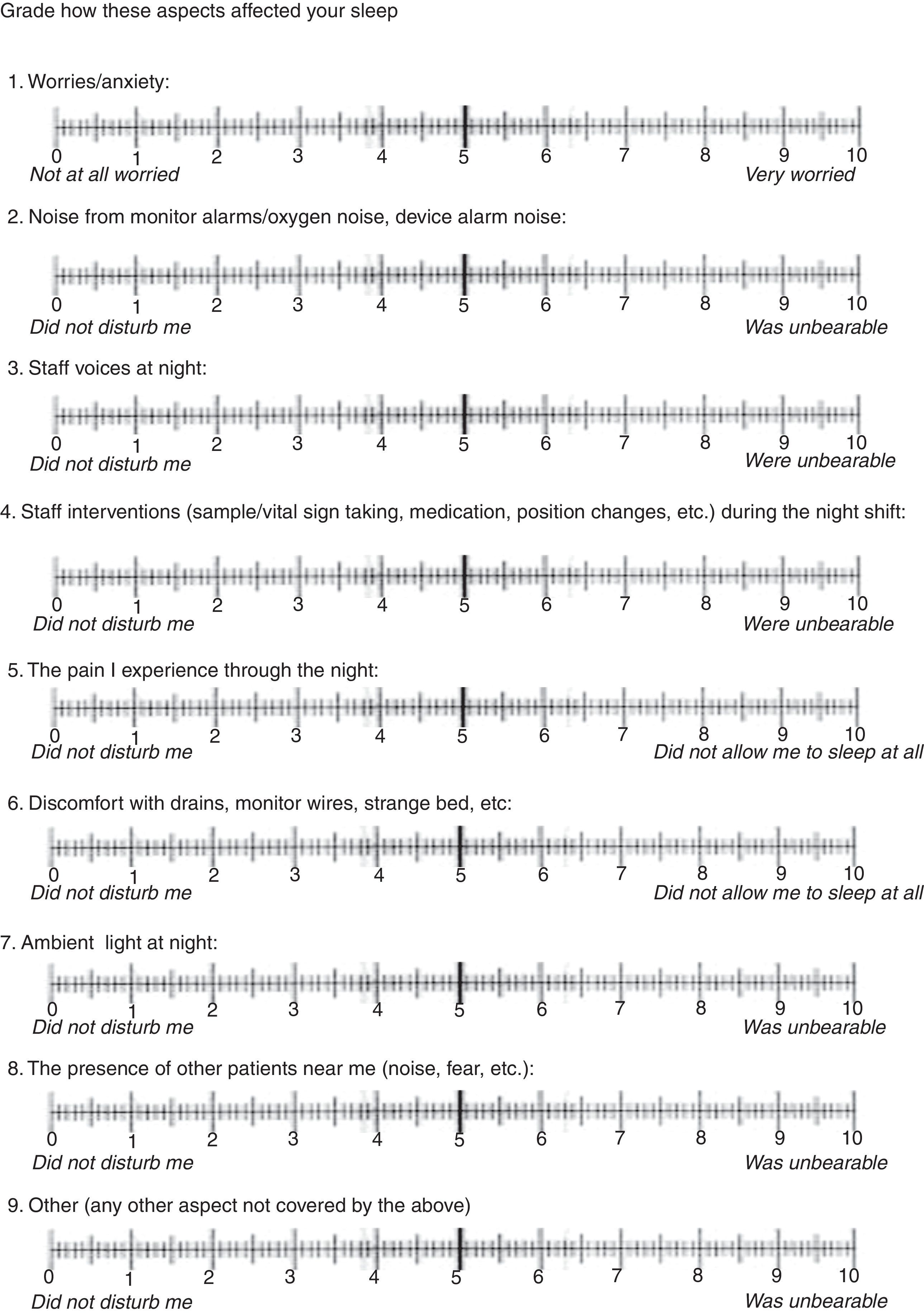
- 3.
Self-administered questionnaire with 9 questions on factors described in the literature that most influence sleep (Fig. 3). The patient graded each factor on a scale from 0mm to 100mm, 0 being the value that least affected their sleep and100mm that with the most impact.
When the score was obtained, it was distributed in numerical ranges to be associated with qualitative interpretations so that scores from 0mm to 33mm showed that the factor studied had little influence on sleep, above 33mm and up to 66mm showed that it had medium impact and scores above 66mm we considered to be of maximum impact.
The data was collected by the research team over 4 months with each of the included patients and during their entire stay in ICU. They were explained the aim and importance of the study and asked to participate. If they gave their consent freely, a member of the research team collected the data from the computerised care plan, filled in the RCSQ with the patient and the 9-item questionnaire, ensuring that each item or question had been correctly understood. The entire process was carried out in the early hours of the morning (from 8h to 10h), so that the patient did not lose their objectivity of their night's sleep.
Data analysisDescriptive and inferential statistics were used to analyse the quantitative data. The values were expressed as mean±standard error of the mean (SEM), 95% confidence interval, and the categorical variables as absolute frequencies. In order to analyse the differences between 2 groups, the Student's t-test was used for unpaired samples, provided normality was demonstrated (Shapiro–Wilk test); otherwise, a non-parametric test was used (Mann–Whitney U test). The categorical variables were studied using the chi-squared or Fisher's exact test. Statistically significant differences were considered with a p value of less than .05. The statistical analysis was performed using SPSS (version 20.0).
Ethical considerationsAll the participants were ensured anonymity, complete data confidentiality and that the questionnaires would be destroyed at the end of the research study. The patients gave their verbal consent. The hospital's ethics committee gave their approval to undertake the study and authorised access to the patients’ computerised clinical histories, which were used exclusively for this study.
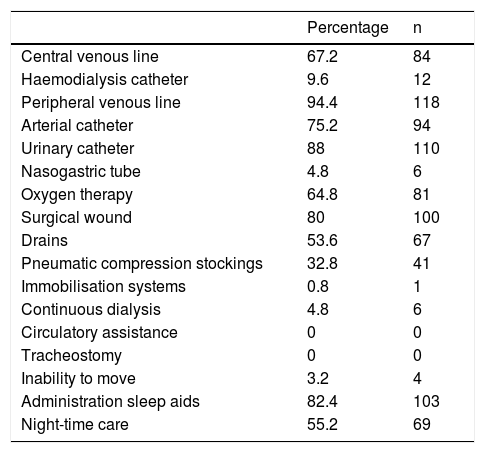
ResultsThe sample comprised 125 patients, 68% were males and 32% females. Seventy-two point eight percent were aged over 60 years, 25.6% between 41 and 59, and 1.6% of the patients were aged between 17 and 40. The stay in the unit was less than 48h for 71.2% of the patients, between 48h and 72h for 13.6% and more than 72h for 15.2%. The admission followed surgical intervention in 77.6% and was of medical cause in 22.4%. The percentage of patients with catheters, drains, wounds and other techniques that might disturb sleep are shown in Table 2.
Distribution of patients according to the presence of catheters, drains, etc. (n=125).
| Percentage | n | |
|---|---|---|
| Central venous line | 67.2 | 84 |
| Haemodialysis catheter | 9.6 | 12 |
| Peripheral venous line | 94.4 | 118 |
| Arterial catheter | 75.2 | 94 |
| Urinary catheter | 88 | 110 |
| Nasogastric tube | 4.8 | 6 |
| Oxygen therapy | 64.8 | 81 |
| Surgical wound | 80 | 100 |
| Drains | 53.6 | 67 |
| Pneumatic compression stockings | 32.8 | 41 |
| Immobilisation systems | 0.8 | 1 |
| Continuous dialysis | 4.8 | 6 |
| Circulatory assistance | 0 | 0 |
| Tracheostomy | 0 | 0 |
| Inability to move | 3.2 | 4 |
| Administration sleep aids | 82.4 | 103 |
| Night-time care | 55.2 | 69 |
The total mean sleep score achieved on the Richards Campbell questionnaire was 52.93mm±2.44. Analysis of each separate item is shown in Table 3. Of the 125 patients, 40% had had a good night's sleep, 35% had had a fair night's sleep and 25% a poor night's sleep.
Richards–Campbell questionnaire scores (n=125).
| Item | Mean | SEM | 95% confidence level |
|---|---|---|---|
| Your sleep last night was: deep sleep/light sleep (depth of sleep) | 50 | 2.51 | 45.02–54.98 |
| Last night the first time you got to sleep you: fell asleep almost immediately/never could fall asleep (speed in falling asleep) | 55.56 | 3.25 | 49.12–62.00 |
| Last night you: were awake very little/were awake all night long (number of awakenings) | 52.48 | 2.60 | 47.33–57.63 |
| Last night when you woke up or were awakened you: got back to sleep immediately/could not get back to sleep | 53.12 | 2.95 | 47.27–58.97 |
| You would describe your sleep last night: a good night's sleep/a bad night's sleep (quality and perception of total sleep) | 53.48 | 2.96 | 47.61–59.35 |
| Total score | 52.93 | 2.44 | 48.10–57.76 |
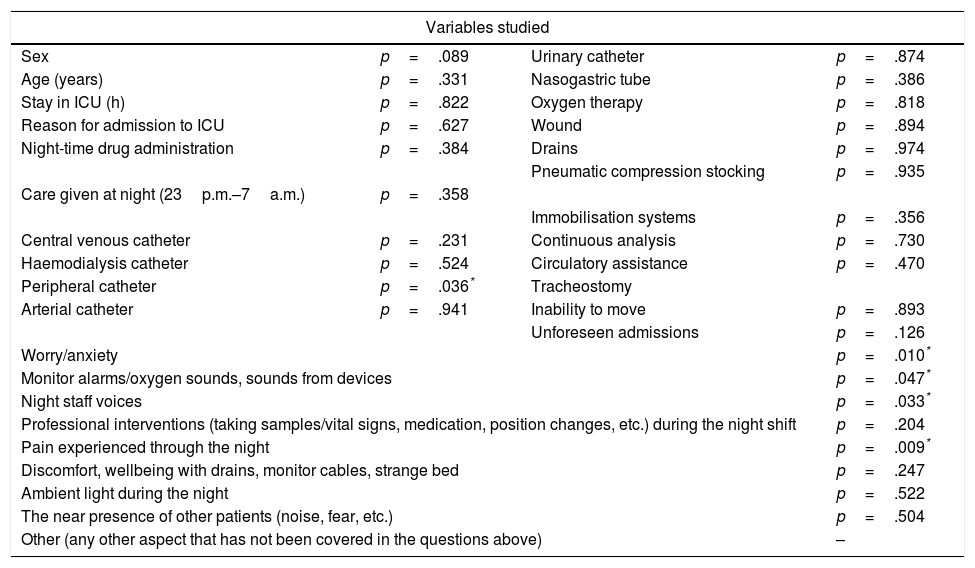
When we compared the patients’ age, sex, days of stay and reason for admission with the scores obtained on the RCSQ, we found no statistically significant differences (Table 4).
Variables studied and statistical significance.
| Variables studied | |||
|---|---|---|---|
| Sex | p=.089 | Urinary catheter | p=.874 |
| Age (years) | p=.331 | Nasogastric tube | p=.386 |
| Stay in ICU (h) | p=.822 | Oxygen therapy | p=.818 |
| Reason for admission to ICU | p=.627 | Wound | p=.894 |
| Night-time drug administration | p=.384 | Drains | p=.974 |
| Pneumatic compression stocking | p=.935 | ||
| Care given at night (23p.m.–7a.m.) | p=.358 | ||
| Immobilisation systems | p=.356 | ||
| Central venous catheter | p=.231 | Continuous analysis | p=.730 |
| Haemodialysis catheter | p=.524 | Circulatory assistance | p=.470 |
| Peripheral catheter | p=.036* | Tracheostomy | |
| Arterial catheter | p=.941 | Inability to move | p=.893 |
| Unforeseen admissions | p=.126 | ||
| Worry/anxiety | p=.010* | ||
| Monitor alarms/oxygen sounds, sounds from devices | p=.047* | ||
| Night staff voices | p=.033* | ||
| Professional interventions (taking samples/vital signs, medication, position changes, etc.) during the night shift | p=.204 | ||
| Pain experienced through the night | p=.009* | ||
| Discomfort, wellbeing with drains, monitor cables, strange bed | p=.247 | ||
| Ambient light during the night | p=.522 | ||
| The near presence of other patients (noise, fear, etc.) | p=.504 | ||
| Other (any other aspect that has not been covered in the questions above) | – | ||
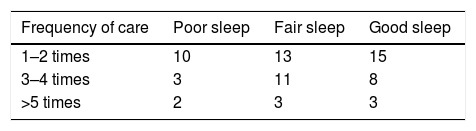
When we studied whether the presence of wounds, drains, catheters, etc., interfered with the quality of sleep, there were no statistically significant differences, except in the case of a peripheral line (p=.036, χ2=6.66) (Table 4). The patients who did not have a peripheral line slept better than those who did. No statistically different differences were found with regard to delivering night-time care either, or with regard to its frequency (Table 5).
When we looked at whether sleep quality was affected whether or not medication was taken to help sleep/improve comfort, patient wellbeing, we found no association between either variable (Table 4), the patients who had been given benzodiazepines (BZP) or opiates achieved the lowest scores on the RCSQ scale. The mean score of the patients who had taken BZP was 49.24mm±4.69 compared to 54.04mm±2.8 of those who had not. The score of the patients who had not received opiates was 54.17mm±2.6 compared to 47.14mm±6.27 for those who had.
Analysis of the items from the questionnaire revealed that the patient's worry/anxiety, their pain, and the environmental noise or staff voices had a significant influence. Whereas 23% of the patients who slept badly reported feeling very worried or anxious, 84% of the patients who slept well did not display worry or anxiety (p=.010, χ2=13.35). Furthermore, 50% of the patients reported that their pain very much affected their sleep, compared to 20% who said it had very little influence (p=.009, χ2=13.57). While 100% of the patients who answered that they were very affected by staff voices slept badly, only 22% of those who said that the voices did not disturb them did not sleep well (p=.033, χ2=10.47). Finally, environmental noise affected quality of sleep, in that 47% of the patients that answered that noise very much affected their sleep slept badly compared to 21% of those who slept badly stated that it affected them very little (p=.047, χ2=9.64). No statistically significant differences were found with staff interventions, discomfort, wellbeing with drains, etc., environmental light and the presence of other patients (Table 4).
DiscussionAfter analysing the results, we were able to confirm that the sleep/rest pattern of the patients admitted to our ICU was characterised by moderately deep sleep, with light arousals and ease in falling asleep again. The mean value of the RCSQ scale was 52.92mm. Nicolás et al.,9 in a previous study performed in the same unit obtained similar scores (51.42mm) except in the frequency of awakenings, which in their case was higher (42.08mm). This might be due to the fact that the structure of the unit was different. In the first study, the cubicles were not individual; they had no door and were only separated by a curtain. Furthermore, the monitoring station was in the middle of the unit and open to the rest of the cubicles, so that alarms, telephones, lights and staff voices were more apparent. Tineo et al. in 20118 obtained similar results, although their frequency of awakenings was higher. Persson Waye et al.,21 in their study to improve environmental noise in an ICU and analyse its affect on sleep, reached similar conclusions, although they used polysomnography as their method. By contrast, Aitken et al.,1 Achury-Saldaña et al.,6 and Frisk and Nordström20 had a lower total RCSQ score (46mm, 41mm and 45.5mm, respectively) and a light sleep pattern with frequent awakenings and difficulty falling asleep again. However a study by Kamdar et al. in 201222 obtained higher scores (57mm). This might be because different interventions were used to improve sleep (dimming the lights, closing doors, etc.) at the time of the study. Iriarte Ramos23 and Richards et al.19 also achieved higher scores (56.85mm and 60.19mm, respectively).
The literature indicates that age has a negative effect on both the amount and the quantity of sleep. As people age, the time taken to fall asleep increases and awakenings are more frequent.24 Our study found no statistical association in relation to age. This is similar to the result of Frisk and Nordström,20 Nicolás et al.,9 Tineo et al.,8 and Iriarte Ramos23 and Gómez.2 By contrast, Achury-Saldaña et al.6 found that older patients slept less well, unlike the result of Bihari et al.,17 who confirmed that patients over the age of 65 slept better in ICU than the young patients.
There is no statistical relationship with regard to the sex of the patients either, as in the literature reviewed,2,6,9,23 apart from Bihari et al.,17 who found women to have a better perception of sleep as they increase in age.
There are no statistical differences in the perception of sleep in relation to days of stay. Our results are similar to those found in the literature.17,23
We found no statistically significant differences in the reason for admission (medical or surgical). This result is similar to that of Iriarte Ramos,23 Bihari et al.17 and Calvete et al.25 Some authors26,27 indicate that, irrespective of the reason for admission, disease involves physiological and emotional stress that have a considerable effect on the amount and quality of sleep, because the person experiences fear and uncertainty, feeling that their life is under threat.
When relating the presence of lines, drains, wound, etc. to sleep, we only found an association between the patient's quality of sleep and the presence of a peripheral line. This result contrasts with those found in the literature. Iriarte Ramos23 found that the patients’ quality of life was affected by the presence of central lines, arterial lines, nasogastric tube, urinary catheter and chest drains. By contrast, they found no association between peripheral lines and sleep. Calvete et al.25 found significant differences with some techniques and procedures (intravenous catheters and nasogastric tubes) when they compared the perception of patients admitted to different locations within the same unit. Ayllón et al.,28 in their study to discover the environmental factors that trigger stress in ICU patients found that the presence of tubes in the nose or mouth, oxygen mask, limited mobility and care given to other patients were among the 10 factors causing the most stress. The literature states that stress generates changes in the sleep–wake cycle causing poor sleep quality.29 Explaining the need and purpose of catheters required by a patient and their early removal might help night-time rest.23
Although there is no association with the administration of BZP, we found that the patients who took them had lower RCSQ scores, similar to the finding by Frisk and Nordström.20 This finding might be because BZP are given to improve sleep, since they shorten the time taken to fall asleep and disruptions, and increase sleep duration but do not improve its depth, so that the patients’ sleep is more superficial, and their perception of their sleep is therefore worse.
The factors that statistically influenced sleep in our study were: pain, worries/anxiety, staff voices and equipment noises.
With regard to worry and anxiety, Zhang et al.30 found statistically significant differences with sleep. Other authors7,8,10,14,16,20,25 also confirm that they affect sleep, although they do not investigate whether or not there is an association. Nurses play an essential role in improving this state of anxiety/worry. Their continuous presence, the calm that they convey, informing the patient of continuous monitoring from the external monitor and resolving, where possible, all queries and concerns are part of the care that can help to reduce worry and anxiety and promote rest.7
Although not all the studies found statistically significant differences between pain and sleep, the literature considers it to be an influential factor.2,8,13,20,23,25,30 In our study the patients who received opiates to control pain had a lower perception than those who did not. Moreover, opiates are described as being associated with suppression of the REM stage, causing sleep fragmentation5,7,11,13,18 but they do play an important role in the patient's comfort and wellbeing.5 Preventing pain is more effective than treating established pain.7 It is appropriate to optimise pain control to improve the patient's comfort and wellbeing and promote better sleep.31
Different forms of noise (alarms, bells, telephones, noises from devices, etc.), as in studies published by other authors,2,3,5,7–9,13–17,20,32 are a factor to be considered and we can intervene to minimise the negative effects. Lowering the intensity of alarms, disconnecting those that are not strictly necessary,23 offering patients earplugs10,12,14,33 and closing cubicle doors to muffle external noises might be helpful interventions.7,23
Bihari et al.17 and Gómez2 studied the different sources of noise and found staff voices to be the most influential factor. Similarly, Akansel and Kaymakçi34 report that staff conversations were perceived to be one of the most annoying sources of noise, the patients closest to the nursing station were those most affected by disturbed sleep. Aragón et al.16 had the same result, although they did not find significant differences. By contrast, Freedman et al.27 and Bosma and Ranieri35 state that noise is not paramount in sleep disruption in ICU. Similarly in the study by Gómez2 it does not seem to be associated with sleeping well or not, although the patients highlighted it as the most annoying factor. Night staff lowering their voices,8 providing earplugs10,12,14,33 and closing cubicle doors7,23,36 are measures that improved night-time rest.
Although light was not found to be a significant variable, as in the papers by Gómez2 and Elliott et al.,32 the great majority of studies report it as a factor that disrupts sleep.1,3,5,8,10,11,14–17 It is routine practice in our unit to turn out the cubicle lights and dim those in the corridors and the nursing station. Blinds are lowered and we close doors, and thus attempt to create a suitable atmosphere for patients to fall asleep.
This study has methodological limitations. One of these limitations is that it was performed in a single centre, with a homogeneous sample (most of the patients were surgical, aged over 60 and short stay [<48h]). Moreover, given the great variability of the medications used to improve sleep and their combined use, no causal relationship could be established between how a particular drug affected sleep. On the other hand, although the RCSQ is an instrument with high reliability and internal validity, it has not been validated in Spanish. Similarly, the 9-item questionnaire is self-administered and has not been subjected to a process of validation. Both questionnaires are hetero-administered, and might cause bias in the patient if they do not feel free to express certain opinions. Another limitation is that the number of lines or their site was not taken into consideration which might influence quality of sleep since an association was found between the perceived quality of sleep and the presence of peripheral venous lines. Furthermore, although the patient was asked whether their pain affected their sleep and it was mentioned as a significant aspect, the effect that the values obtained on the verbal numerical scale might have had on the perception of sleep was not graded. Both aspects could be examined in future studies, as well as validation of the RCSQ.
ConclusionsOur patients’ perception of night-time sleep in the ICU unit was fair.
The disturbing factors were: peripheral line, worry/anxiety, pain, noise, and staff voices.
Optimising pain management, answering concerns or worries, minimising environmental noise and staff voices would improve sleep quality.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Carrera-Hernández L, Aizpitarte-Pejenaute E, Zugazagoitia-Ciarrusta N, Goñi-Viguria R. Percepción del sueño de los pacientes en una Unidad de Cuidados Intensivos. Enferm Intensiva. 2018;29:53–63.