McArdle´s disease or glycogenosis type V is a rare disease due to deficiency of muscle myophosphorylase leading to inability to degrade glycogen at this level. Patients have fatigue, pain, and cramps on a regular basis. In addition, after intense exercise or stressful situation, they are exposed to cellular lysis. This can occur in the form of rhabdomyolysis and myoglobinuria, a potentially serious clinical syndrome if not treated quickly.
Case evaluationWe present the care plan of a 38-year-old man with McArdle´s disease and secondary rhabdomyolysis on physical exercise, which required attention in the Emergency Department for 24 h, as well as his subsequent admission to the ward. A nursing evaluation was performed following the care model of Virginia Henderson.
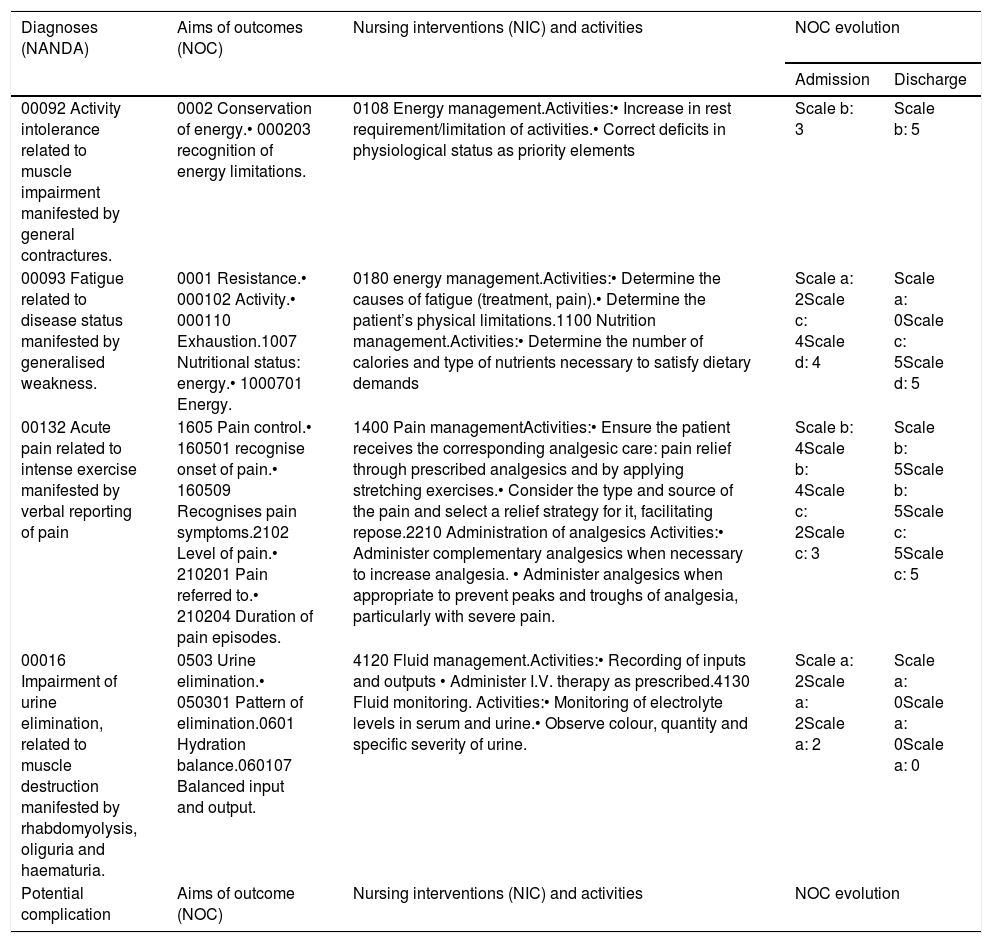
DiagnosisPriority was given to nurse diagnoses: (00016) deterioration of urinary elimination, (00092) activity intolerance, (00093) fatigue and (00132) acute pain; and potential complication: risk of acute renal failure.
PlanningThe Care Plan is developed following the NANDA-NIC-NOC methodology, with special attention to alterations in the elimination and musculoskeletal system. The diuresis is monitored. Fluid replenishment is performed, and analgesic medication is given.
DiscussionThere is little literature on the nursing care of patients with McArdle’s disease, which has limited the comparison of our results with those of other authors. However, given the good response of the subject through fluid replacement, optimal pain control, rest, they made a rapid recovery.
la enfermedad de McArdle o glucogenosis tipo V es una enfermedad rara debida al déficit de miofosforilasa muscular lo que produce incapacidad para degradar el glucógeno a este nivel. Los pacientes presentan fatiga, dolor y calambres de forma habitual. Además, tras un ejercicio intenso o situación estresante, están expuestos a lisis celular. Esto se puede manifestar en forma de mioglobinuria y rabdomiólisis, síndrome clínico potencialmente grave si no se trata con rapidez.
ValoraciónSe presenta el caso de un varón de 38 años con enfermedad de McArdle y rabdomiólisis secundaria a la realización de ejercicio, que precisó atención en el Servicio de Urgencias durante 24 horas, así como su posterior ingreso en Unidad de Hospitalización. Se realizó una valoración enfermera siguiendo el modelo de cuidados de Virginia Henderson.
DiagnósticoSe priorizaron los diagnósticos enfermeros: (00016) deterioro de la eliminación urinaria, (00092) intolerancia a la actividad, (00093) fatiga y (00132) dolor agudo; y la complicación potencial: riesgo de fallo renal agudo.
PlanificaciónSe elabora Plan de Cuidados siguiendo la metodología NANDA-NIC-NOC, con especial atención a las alteraciones en la eliminación y en el sistema musculoesquelético. Se realiza monitorización de la diuresis. Se realiza reposición de líquidos y se administra medicación analgésica.
DiscusiónExiste escasa literatura sobre los cuidados enfermeros de pacientes con enfermedad de McArdle lo que ha limitado la comparación de nuestros resultados con los de otros autores sin embargo dada la buena respuesta del sujeto mediante reposición de líquidos, un óptimo control del dolor y el reposo demostraron una rápida recuperación del paciente.
McArdle disease is an autosomic recessive hereditary disorder, qualified as a “rare disease” due to its low prevalence, which in the Spanish population is that of 1/167,000 people.1 It is caused by a mutation of the gene PYGM, generated by a deficiency of muscle myophosphorylase which is the enzyme responsible for metabolizing glycogen in the skeletal muscle. This enzyme is not found to be changed in other organs (heart, liver).1
The main symptom of the disease is intolerance to exercise manifested by pain, fatigue, muscular stiffness and weakness.2 When the patients do load-bearing exercises, they initially experience an increase in heart rate, muscle pain and intense fatigue, followed by a phase of symptom improvements after 7−8 min. This is a patognomonic phenomenon called “second wind”, which is due to a higher availability of alternative energy substrates of non muscular origin, such as glucose and free fatty acids,3,4 through secondary mobilization during exercise and increased local blood flow.
Myophosphorylase deficiency causes a change to the metabolism of carbohydrates in muscle cell. Furthermore, it affects the correct functioning of the sodium-possession AT Pase pump, which triggers off an accumulation of intracellular sodium and water. On certain occasions this may provoke the rupture of the cellular membrane (rhabdomyolysis). In this situation, the dissolved products of damaged muscle cells, such as myoglobin or some of the muscle enzymes such as creatine-kinase (CK) are released from blood circulation. This means that the patients with McArdle disease usually present with baseline plasmatic levels above 1,000 U/L, that may increase under certain situations such as highly intense physical activities.4 Myoglobin is harmful for the kidney and may cause acute kidney failure. The severity of its affect on the kidneys and its symptoms vary according to the magnitude of the muscle damage, and it may lead to vomiting, fever, myalgias, changes in urine colour and quantity and even changes to level of consciousness or acute irreversible kidney failure.5
This disorder currently has no cure, and management is based on symptom control. It’s essential pillar is physical exercise, where regular practice of controlled sport improves symptoms4; followed by dietary recommendations which consist of the ingestion of rapid absorption sugars prior to the initiation of exercise to improve tolerance.6 Some authors also recommend a ketogentic diet with which several analytical parameters would improve. However, this is a controversial issue due to the harmful effects on the body in the medium and long term.7 With regard to treatment of the acute metabolic complications, in one study with 45 patients with McArdle disease, in 17 cases myoglobinuria was detected and five presented with severe kidney failure and a need for haemodialysis.5
The lack of publications addressing nursing care in patients with McArdle disease justify the interest in presenting the following clinical case.
Case descriptionMale aged 38 years (height 1.74 m; weight 73.3 kg), with no known allergies, diagnosed with McArdle disease through a genetic study 20 years ago. He is self-employed (Barthel scale: 100, Lawton-Brody scale: 8) and physically active.
He consulted the emergency unit with an osteomuscular pain in his lower limb from two hours previously and a change in urine colour, after carrying out intense exercise (squats with 50 kg of weight).
Physical examination showed blood pressure of 145/85 mmHg and 96% oxygen saturation. An electrocardiogram (ECG) with sinus rhythm of 88 bpm was performed. A pain intensity of 8 out of 10 presented, according to the visual analogue scale (VAS), in both femoral muscle quadriceps and in the lumbar region muscles.
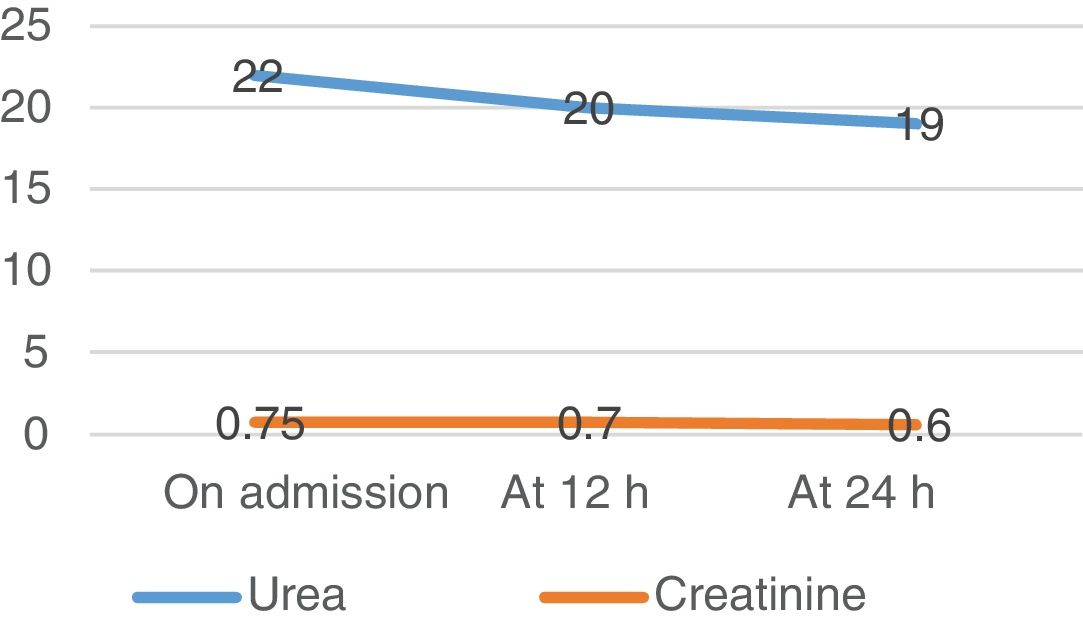
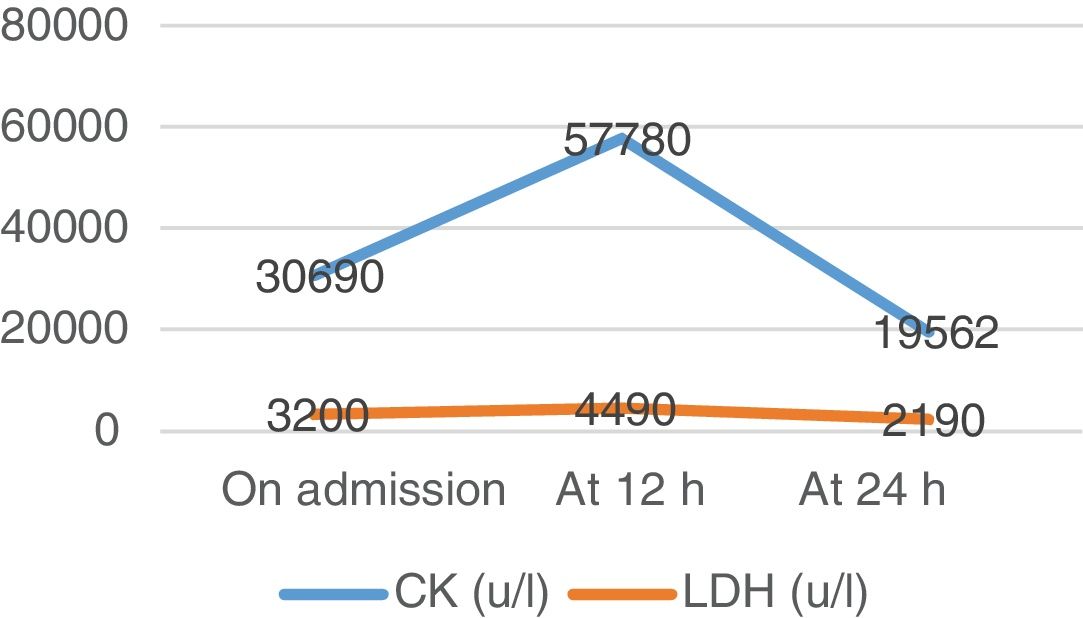
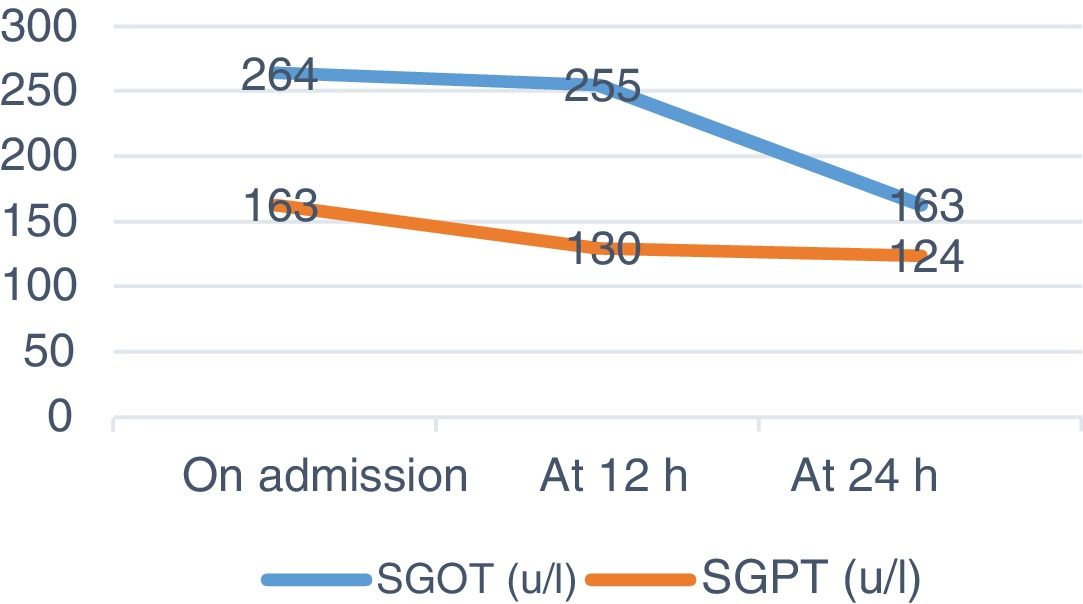
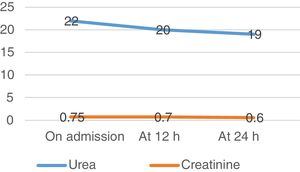
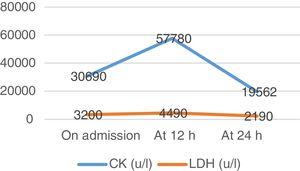
A venous blood test and urine sample test were performed. In the biochemical analysis high levels of CK and other muscle enzymes occurred (Figs. 1–3). Urine was a burgundy colour and the presence of myoglobinuria was detected.
The patient was admitted to the Emergency Observation unit where peripheral venous catheterisation was performed. On admission a nursing assessment was made following the basic need care model of Virginia Henderson, with changes to the elimination system and mobility standing out.
Respiration: Normal breathing pattern, resting respiratory rate of 14 rpm. Smoker of 10 cigarettes per day. Blood pressure of 120/67 mmHg and heart rate of 90 bpm. Normal auscultation. ECG without changes. Takes 100 mg levothyroxine for hypothyroidism.
Nutrition and hydration: Independent. Drinks 2–3 litres of water per day and combines a ketogenic diet with a Mediterranean one. He stated that he makes better use of his energy with the Ketosis and the CK in tests improved, but it is almost impossible to carry out a diet without carbohydrates. That day he had eaten rice and a protein shake after exercise.
Waste elimination: Independent, no oedemas. Burgundy coloured urine from probable rhabdomyolysis of recent onset. Urine analysis revealed +++ haematuria. He had drunk over 2 L of water in the previous two hours but oliguria was present.
Mobility and posture maintenance: Independent. He exercises daily which is important to improve the symptoms of the disease. At the time of assessment, contracture and myalgias in the lumbar region, quadriceps and calves were detected, which impeded normal mobility. He referred to a loss of strength in his limbs due to the contractures.
Sleep and relaxation: No changes to sleep pattern.
Dressing and undressing: Autonomous. Good general appearance.
Body temperature: Lives alone in a well-conditioned home. Temperature of 37.5 °C.
Hygiene and skin integrity: Appropriate hygiene. Hydrated skin.
Dangers: Oriented, no risk of falling.
Communication: No sensory impairments.
Living according to beliefs and values: No changes.
Self-realisation and self-esteem: Nurse for 10 years. Professionally accomplished.
Participation in recreational activities: Active social life. His favourite hobby is travelling.
Learning: University qualifications.
Physiological saline solution infusion at 0,9% to 1,000 mL/h initiated, with strict control of liquid ingestion and diuresis. During the first hour, he presented with oliguria with a diuresis of 20 mL/h, burgundy colour. From the second hour, polyuria of 200 mL/h. After four hours the urine was normal in colour.
The patient presented with muscle contractures at lumbar and lower limb level. To control the pain he was administered non opioids analgesics, avoiding the use of non steroid anti-inflammatories due to the risk of impairing renal function. Due to the low analgesic response (7/10 on the VAS after medication administration) he was administered minor opioids reducing the perceived pain by the patient (2/10 on the VAS).
Twelve hours after admission CK levels rose, and saline solution therapy was maintained for 12 h at a rhythm of 250 mL/h. Water intake was increased up to 3 L per day. Urine presented with normal colour and characteristics. After 24 h new analysis was performed where CK levels dropped and changes to renal parameters were absent (urea and creatinine).
The patient was transferred to the Internal Medicine Unit until he was discharged after 72 h, following complete clinical recovery.
Nursing diagnosis, care plan and assessmentNursing diagnoses, both autonomous and collaborative were identified in accordance with the NANDA8 taxonomy and one potential complication, given their relevance. The expected results (NOC)8 and nursing interventions (NIC)8 (Table 1).
NANDA-NOC-NIC care plan, with evolution of the outcome indicators.
| Diagnoses (NANDA) | Aims of outcomes (NOC) | Nursing interventions (NIC) and activities | NOC evolution | |
|---|---|---|---|---|
| Admission | Discharge | |||
| 00092 Activity intolerance related to muscle impairment manifested by general contractures. | 0002 Conservation of energy.• 000203 recognition of energy limitations. | 0108 Energy management.Activities:• Increase in rest requirement/limitation of activities.• Correct deficits in physiological status as priority elements | Scale b: 3 | Scale b: 5 |
| 00093 Fatigue related to disease status manifested by generalised weakness. | 0001 Resistance.• 000102 Activity.• 000110 Exhaustion.1007 Nutritional status: energy.• 1000701 Energy. | 0180 energy management.Activities:• Determine the causes of fatigue (treatment, pain).• Determine the patient’s physical limitations.1100 Nutrition management.Activities:• Determine the number of calories and type of nutrients necessary to satisfy dietary demands | Scale a: 2Scale c: 4Scale d: 4 | Scale a: 0Scale c: 5Scale d: 5 |
| 00132 Acute pain related to intense exercise manifested by verbal reporting of pain | 1605 Pain control.• 160501 recognise onset of pain.• 160509 Recognises pain symptoms.2102 Level of pain.• 210201 Pain referred to.• 210204 Duration of pain episodes. | 1400 Pain managementActivities:• Ensure the patient receives the corresponding analgesic care: pain relief through prescribed analgesics and by applying stretching exercises.• Consider the type and source of the pain and select a relief strategy for it, facilitating repose.2210 Administration of analgesics Activities:• Administer complementary analgesics when necessary to increase analgesia. • Administer analgesics when appropriate to prevent peaks and troughs of analgesia, particularly with severe pain. | Scale b: 4Scale b: 4Scale c: 2Scale c: 3 | Scale b: 5Scale b: 5Scale c: 5Scale c: 5 |
| 00016 Impairment of urine elimination, related to muscle destruction manifested by rhabdomyolysis, oliguria and haematuria. | 0503 Urine elimination.• 050301 Pattern of elimination.0601 Hydration balance.060107 Balanced input and output. | 4120 Fluid management.Activities:• Recording of inputs and outputs • Administer I.V. therapy as prescribed.4130 Fluid monitoring. Activities:• Monitoring of electrolyte levels in serum and urine.• Observe colour, quantity and specific severity of urine. | Scale a: 2Scale a: 2Scale a: 2 | Scale a: 0Scale a: 0Scale a: 0 |
| Potential complication | Aims of outcome (NOC) | Nursing interventions (NIC) and activities | NOC evolution | |
| Admission | Discharge | |||
|---|---|---|---|---|
| Risk of acute kidney failure secondary to muscle destruction. | 0503 Urine elimination.• 050303 Quantity of urine.• 050304 Colour of urine. | 0509 Urine elimination management.Activities:• Timed control of urine elimination, including frequency, density, smell, volume and colour. | Scale a: 2Scale a: 2 | Scale a: 0Scale a: 0 |
Likert scale to assess outcome markers.8 Scale “a”: Not compromised(0), Slightly compromised (1), Moderately compromised (2), Substantially compromised (3), severely compromised (5). Scale “b”: Never demonstrated (1), Rarely demonstrated (2), Sometimes demonstrated (3), Frequently demonstrated (4), Always demonstrated (5). Scale “c”: Severe (1), Substantial (2), Moderate (3), Slight (4), None (5). Scale “d”: Severe deviation from normal range (1), Substantial deviation from normal range (2), Moderate deviation from normal range (3), Slight deviation from normal range (4), No deviation from normal range (5).
The first aim was to prioritise diagnoses aimed at the prevention of rhabdomyolysis complications, so as to avoid possible kidney failure and impairment of kidney function by intensive fluid replacement and meticulous monitoring of dieresis, with surveillance of volume and appearance. Also using rest so as not to perpetuate muscle damage, balancing the prevention of complications and early health recovery. Improvement of the patient’s well-being was also prioritized, using a comfortable posture and the administration of analgesics. Since McArdle disease has no treatment at this present time, nursing diagnoses which were prioritized were those that ensured the prevention of rhabdomyolysis complications and therefore its advance. Fatigue and intolerance to activity improved with stretching exercises and rest. Recovery was rapid, with improvement of analytical parameters after 24 h (Figs. 1–3) and the NOC result criteria on discharge (Table 1). To ensure optimum care continuous assessment was carried out throughout the care plan. On final assessment of the process, it was demonstrated that stabilization in CK had taken place, with the confirmation of a normal urine colour prior to discharge from the hospital ward. Pain control was also assessed objectively using the VAS scale and promoting rest.
DiscussionMcArdle disease, described for the first time in 1951 by Brian McArdle, is the most frequent muscular glycogenosis and one of the most common genetic myopathies.9 Physical and psychological symptoms lead to a sedentary lifestyle and excess weight which can impair the quality of life of these patients. In most cases, the disease does not affect life expectancy but the activities of these patients may be severely limited. However, in this respect there is major variability between them.7 In this study we describe a process of rhabdomyolysis, which is a common complication in patients with McArdle disease.2 The rapid attention by the multiprofessional team, the putting into place of the nursing process and the good patient response to rehydration avoided complications such as kidney failure and haemodialysis.10 The care plan was based on comprehensive assessment, highlighting strict monitoring of rhabdomyolysis evolution.11 Thanks to this, 100% of nursing diagnoses were resolved on discharge. As reflected in the literature, intravenous fluid therapy, increased hydration, pain control and rest, guarantee an optimum approach to rhabdomyolysis.12 Furthermore, standardized language (NANDA-NICNOC)8 means that care may be planned and assessed. In the clinical case exposed a positive result ensued in the resolution of the whole nursing process. Little literature exists on the nursing care of patients with McArdle disease, which has limited comparison of our results with those of other authors. Treatment of McArdle disease is based on the control of physical activity and dietary measures. Aerobic exercise is recommended in all patients with McArdle disease as cramps are an early sign of alarm to reduce physical intensity.5 The results from small numbers of patients in three non random studies indicate that aerobic training is safe for the patients with McArdle disease. However, no randomised controlled trial proof exists regarding the beneficial therapeutic effects of aerobic exercise.13 It has been demonstrated that regular, moderate physical exercise increases tolerance to exercise in these patients.9 Several authors recommend complementing it with vitamin B6 and B12, although its use has not been related to a clear clinical improvement or reduction in the risk of rhabdomyolysis.6
Results cannot be generalised as this was a single case and had no support from previous publications. However, given the good patient response the following recommendations should be assessed as possible guidelines in addressing the problem: encourage self-care for the patient; prescribe appropriate physical activity; avoid strenuous activity and increase intake of water during exercise to prevent complications.11
ConclusionsMcArdle disease is a myopathy caused by myophosphorylase deficiency. Although no proof exists regarding significant benefits of any specific nutritional or pharmacological treatment for McArdle disease, quality of life may be improved for its patients and rhabdomyolysis and kidney failure avoided. Early care and an appropriate approach to care needs avoid severe complications, promoting rapid patient recovery.
Montserrat Solis-Muñoz,in charge of research into care, Nursing Unit of the University Hospital Puerta de Hierro, Majadahonda.
Please cite this article as: Nafría-Soria H, Moreno-España J, Sánchez-Herrero H, García-Menéndez E, Moreno-Del Castillo C, Fernández-Valle I. Rabdomiólisis en un paciente con enfermedad de McArdle. Enferm Intensiva. 2020. https://doi.org/10.1016/j.enfi.2020.02.006