Aiming to contribute on the investigation of discriminative features of the borderline personality disorder (BPD) and bipolar disorder (BD), we investigated the capacity of specifics pathological traits in discriminating BPD from BD patients. Participants were 258 adults: 30 BPD outpatients, 28 BD outpatients, and 200 non-patients. Through repeated measures ANOVA (with post hoc), contrast ANOVA and regression analyzes, we verified the discriminatory capacity of emotional dependency, emotional instability, impulsiveness and aggressivity traits. As expected, the BPD patients showed higher severity in all traits, but impulsiveness. The most discriminative traits were from emotional instability, specifically Anxious worry and Hopelessness traits.
One meta-analysis study1 reported that comorbid borderline personality disorder (BPD) among patients with bipolar disorder (BD), and vice versa, is common, with about one in five people presenting a BPD-BD comorbid diagnosis. Although comorbidity is typical, and several commonalities are present,2 studies comparing BPD and BD suggest that they are separate and unique.3,4
Empirical studies have found many indicative variables differentiating BPD and BP, including personality traits.2,4–6 Emotional lability (BPD∼ or >BD), impulsiveness (BPD>BD), aggressivity/hostility (> BPD), harm avoidance (> BPD), sensitivity to criticism and rejection (> BPD) are among the most frequently investigated traits.
Following previous recommendations,7 our aim was to investigate the capacity of hypothesized pathological traits in discriminating BPD from BD patients. According to previous empirical evidences, we focused on emotional dependency, emotional instability, impulsiveness,2,6,8–10 and aggressivity/hostility traits.6,8,11
Two main hypotheses were tested: h1: BPD patients should present higher severity in comparison to BD patients,10 so, higher scores should be observed mainly in emotional dependency factors, i.e., Self-devaluation, Avoidance of abandonment, and Insecurity,12 and hostility and impulsiveness factors, i.e., Violence, Impulsiveness and Risk taking factors2,5,6,8,11,12; h2: BPD patients should present similar9 or even higher levels8,10 of emotional instability in comparison to BD patients. Furthermore, as our study included a community sample as a baseline for the other groups, a third peripheral hypothesis was tested (h3): non-patients should present lower means in all factors in comparison to BPD and BD patients.
Materials and methodsSampleParticipants were 258 Brazilian adults, divided in three groups: psychiatric outpatients diagnosed with BPD (BPD patients; n=30), with age between 19 and 56 years old (M=36.7; SD=10.5), mainly women (83.3%), White (70%), and undergraduate students (73.4%); psychiatric outpatients diagnosed with bipolar disorder (n=28; BD patients), aging from 19 to 73 years old (M=41.8; SD=13.1), composed mostly by women (64.3%), White (65%) and undergraduate students (70.3%); and community sample (n=200), with age between 19 and 58 (M=24.1; SD=5.9) also composed mainly by women (55.5%), White (77%) and undergraduate students (95.5%). We included the community sample in the study design as a baseline reference for the other groups. Outpatients were diagnosed by experienced psychiatrists, including administration of standardized tools as the M.I.N.I. Mini International Neuropsychiatric Interview13 and the Structured Interview for DSM-IV-TR axis II.14 For this study, we did not consider comorbid cases of BPD-BD. Although we are aware that the BD group was mainly composed by BD-II patients, as expected,1 a detailed control for BD type was not realized.
InstrumentsDimensional Clinical Personality Inventory 2 (IDCP-2)This self-report inventory for adults, developed in Brazil, was originally based on Millon's personality theory and axis II from DSM-IV-TR,15 and was designed to be used for clinical purposes. In this research, we used a revised version, the IDCP-2,16 which is in accordance to new taxonomic proposals.17 IDCP-2 is composed by 206 items, grouped in 47 factors and 12 broad dimensions (Dependency, Aggressiveness, Mood Instability, Eccentricity, Attention Seeking, Distrust, Grandiosity, Isolation, Criticism Avoidance, Self-sacrifice, Conscientiousness and Inconsequence). For this study we selected the following dimensions and respective factors, according to previous literature6,8,11,12: Dependency (Self-devaluation, Avoidance of abandonment, and Insecurity), Aggressiveness (Antagonism and Violence), Mood Instability (Vulnerability, Anxious worry, and Hopelessness), and Inconsequence (Impulsiveness, Risk taking, and Deceitfulness). Previous studies investigated the psychometric properties of these factors.18–21 For our sample, internal consistency reliability of the dimensions varied from .83 to .91.
ProcedureThe research was approved by a Committee of Ethics in Research. People from the community sample were recruited via online social networks, and the administration were online using Google Forms. The outpatient's groups were invited and consent in participate through a Brazilian University Psychiatry Hospital. All participants received detailed information concerning the aims of the study and signed an informed consent to use the data.
Statistical analysisSome individuals did not answer all IDCP-2 items. At first, we applied the equating procedure22,23 from a dataset with 4871 individuals, allowing the estimation scores of all dimensions and factors to the sample. From this dataset, we selected individuals from the outpatient's groups (nBPD=30; nBD=28) and we randomly selected 200 individuals from the community sample group. Our database was composed by a total of 258 individuals, extracted from the 4871 dataset.
We analyzed data using repeated measures ANOVA, comparing pathological traits profile between groups. Effect size was the ηp2, interpreted according to Cohen, Miles and Shevlin.24 We also computed ANOVA post hoc tests (Tukey), and planned contrast ANOVA. For contrast ANOVA groups were weighted as −1 for non-patient, 0 for BD, and 1 for BPD, according to severity level (i.e., non-patient<BD<BPD). As a measure of the effect size, we calculated the r effect size (r-ES),25 by the formula r-ES=SqRt(t^2/(FBG(dfBG)+dfWG)). Regression analyzes complemented the group comparison tests, as previous suggested in literature.26 For logistic regression analysis, dependent variable was binary, BPD patients and bipolar patients; for linear regression analysis, dependent variable included the three groups. In both cases independent variables were personality factors. Enter method was used. The level of significance adopted was ≤.05. Analyses were performed using SPSS 21.
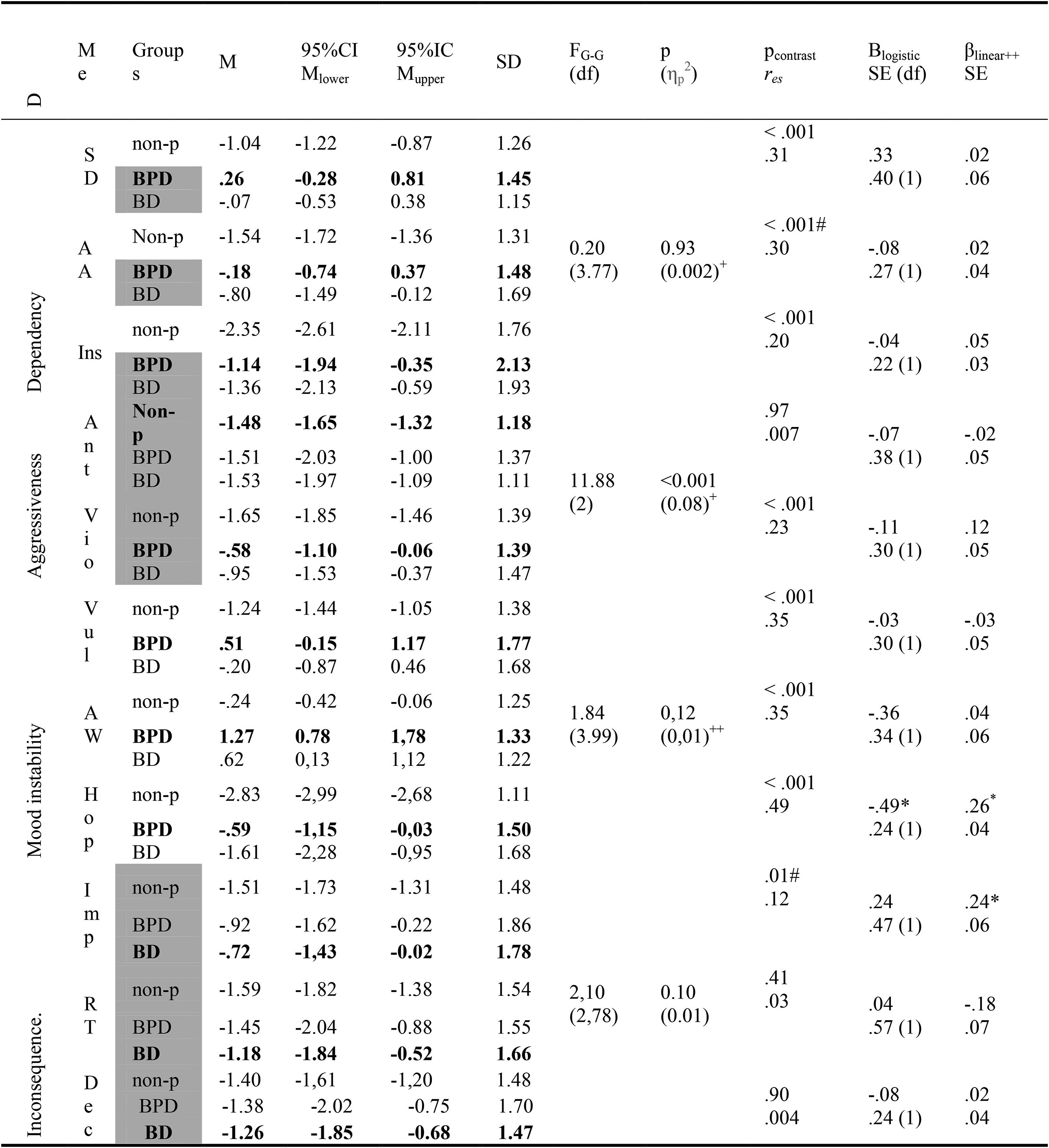
ResultsTable 1 presents groups comparison and predictive tests: IDCP-2 dimensions (column 1), IDCP-2 factors (column 2), groups (column 3), mean, mean confidence interval and standard deviation (columns 4–7), repeated measure ANOVA F's and degrees of freedom (column 8), repeated measures ANOVA's significance and effect size (column 9), contrast ANOVA's significance and effect size (column 10), logistic regression's B, standard error and degree of freedom (column 11), and linear regression's beta and standard error (column 12).
Groups comparison non-patient (n=198), BPD (n=30), BD (n=27) and predictive analyzes.
Note. D=Dimensions; Me=Measures; G–G=Greenhouse–Geisser; Post hoc differences are highlighted by grayish cells, showing groups that did not differ; In bold higher means; +=sex was significant as a control variable; ++=age was significant as a control variable; #=homogeneity not observed; *=significant in regression model; --=variable not entered in the regression model; SD=Self-devaluation; AA=Avoidance of abandonment; Ins=Insecurity; Ant=Antagonism; Vio=Violence; Vul=Vulnerability; AW=Anxious worry; Hop=Hopelessness; Imp=Impulsiveness; RT=Risk taking; Dec=Deceitfulness.
BPD patients presented higher means in more than 60% of measures. Although Aggressiveness have showed significant differences and moderate effect in repeated ANOVA,24 the post hoc did not supported these findings. Post hoc test suggested significant differences for the three factors from Mood instability. Fig. 1 presents group profiles according to repeated measures ANOVA. Contrast ANOVA indicated almost all factors as significant, excluding Antagonism, Risk taking, and Deceitfulness, generally with higher scores for BPD and low to moderate effects. One factor was significant in logistic regression model (Hopelessness; r2Cox&Snell=.20; r2Nagelkerke=.26; correct percentage for BPD was 73.3% and 58.3% for bipolar), and two in linear regression model (Hopelessness and Impulsiveness; r2adjusted=.47).
DiscussionResults of our study demonstrate differences between BPD and BD patient's assessments of pathological traits. Relative to our hypothesis, the results showed that (1) BPD patients obtained higher scores in all expected traits, but impulsiveness, totalizing more than 60% of the traits; (2) BPD patients scored higher in emotional instability traits, mostly Anxious worry and Hopelessness; (3) the reference group, i.e., community sample, scored lower than the other groups for all pathological traits.
The first hypothesis of the study, that BPD patients would be higher in traits related to emotional dependency (Self-devaluation, Avoidance of abandonment, and Insecurity), hostility (Violence) and impulsivity (Impulsiveness and Risk taking), was partially supported. Overall, in agreement with previously studies,10 BPD patients presented major severity in the profile outlined by mostly hypothesized traits, except impulsivity. IDCP-2's Impulsiveness and Risk taking factors are related to, respectively, deficiencies in premeditation capacity and the need to intense experiences and feelings,18 resembling factors from other self-report scales, as UPPS2 (Lack of premeditation and Sensation seeking factors, respectively). We conjecture whether the low scores observed for BPD patients in Risk taking are related to the tendency of this individuals to harm avoidance.5 Moreover, the presence of BD-I patients in the BD group could explain these unexpected findings, as this type of BD is typically related to hypomania. Future studies should investigate if similar results are observed for a BD group composed only by BD-II patients.
The second hypothesis stated that BPD patients should present similar or even higher scores of emotional instability, represented in this study by Vulnerability, Anxious worry, and Hopelessness factors21 in comparison to BD patients. Our expectations were mixed, as previous findings disagreed between similar levels and higher levels in these traits for BPD patients. However, our results not only suggested higher scores of emotional instability for BPD patients,8,10 but also that its factors (Vulnerability, Anxious worry, and Hopelessness), were the most discriminative among all the traits presently considered. Specifically, Anxious worry and Hopelessness showed better discriminative capacity, suggesting general anxiety with future events and the pessimistic tendency to think about the future as the main predictors for differentiating BPD from BD patients.
Our last hypothesis, not central according to the scope of the study, but contextualizing the discriminative capacity of the administered measures, anticipated general lower means for the community sample in comparison to BPD and BD samples. This hypothesis was supported and confirms that the psychiatric outpatients’ groups reached pathological levels in general for pathological traits.
Potential limitations of our study include (1) absence of comorbid BPD-BD patients; (2) individuals were volunteers rather than a consecutive series presenting for treatment and thus were not necessarily a representative sample; (3) participants were taking a variety of medicines; (4) the BP group consisted predominantly of BD-II patients. Regarding this last observation, although a weakness of the study, the majority of BD-II in the BD group enables a more clinically relevant comparison group with BPD, as differential diagnostic difficulty is typically for this type and not BD-I (16).
FundingThere was no funding for this work.
Conflict of interestNone.