The contributions of the authors were as follows: JO: conception, design, and supervision of the study; RM: general design, medical examination, manuscript preparation, and data interpretation; FJDB: Pathologist to study the biopsies; BS: contributed to the experimental design; MG: general design, statistical analysis, and manuscript preparation. All authors agreed on the final version of the manuscript. Authors had no conflict of interest.
¿ INTRODUCTION
Electrical excision of cervical lesions was first used in the nineteenth century. Hunner (1906) was the first reporting the use of therapeutic electrocauterization.1 Rene Cartier in 1981 adapted a small loop electrode using low voltage and in 1989 Walter Prendiville for the first time introduced radio frequencies to perform the excision of the cervical transformation zone using a large loop (LLETZ).2,3 This technique has become widely used and offers the advantages of obtaining a large specimen for histopathological diagnosis, it is well tolerated by patients when performed under local anesthesia on an outpatient basis, has few complications and side effects, and has a relatively low cost;4 in addition, it allows to correlate colposcopic impression with the histology, and micro-invasion can be ruled-out.5 Also, fertility is preserved. Disadvantages include post-treatment cervical stenosis,6 infections, bleeding,7 and thermal damage of the margins that may preclude an adequate study of the margins.4
LLETZ is an effective treatment of cervical intraepithelial neoplasia (CIN) and thus avoids the progression to invasive carcinoma.
The persistence or recurrence of CIN following LLETZ is related to several factors such as degree of the disease,8 positive endocervical curettage,9 diagnosis of positive margins of the specimen.9-11 Ghaem-Maghami demonstrated that after incomplete resection, the relative risk (RR) of having a recurrence of disease of any degree was 5.47 (confidence interval [CI] 95% 4.37-6.83).12 Tan et al. report that only positive margins after LLETZ are an independent risk factor (p <0.05, odds ratio [OR] = 4.20)13 and Livasy comments on the presence of involved endocervical glands as a factor.14
Chien-Hsing points out the usefulness of clinical indicators such as positive endocervical margins, age over 50, and disease in multiple quadrants as having a positive predictive value of 40%, 31.4% and 21.9%, respectively.15 The management of patients with residual lesions post LLETZ is still controversial. Incomplete resection is ignored on many occasions when patients are followed. Follow-up is also done by cytology, a second loop excision, and even hysterectomy. There are no reports in the literature on endocervical brushing of the cervix immediately post LLETZ with histological study of the specimen vs. endocervical brushing in cases with positive margins as a predictor of residual disease.
¿ OBJECTIVES
To study the concordance of positive predictive value of endocervical brushing performed immediately following LLETZ and histological results of cervical cones with positive endocervical margins, as predictors of residual disease.
¿ METHODS
A prospective study including 1817 patients referred with abnormal cytology and treated by LEETZ was undertaken at the Colposcopy Clinic, General Hospital of Pachuca, Hidalgo, Mexico.
The Ethics and Research Committee from the same hospital approved the protocol; informed consent was obtained from all patients.
Demographic data included age, educational level, marital status; reproductive data included number of pregnancies and children, age at sexual debut, number of sexual partners, and method of contraception; clinical data included previous cytological results, index cytology, Reid index,16 and Campion's level.17
These 1877 patients underwent endocervical brushing of the remaining endocervical canal immediately after removing the specimen; 344 patients had a high grade intraepithelial lesion on cytology, histology, and colposcopy. In 62 patients margins were positive on histology and the endocervical brushing was also positive. These 62 patients underwent a new treatment (LEETZ or hysterectomy) within 6 (± 2) months.
All 1877 patients were referred to the Colposcopy Clinic due to an abnormal cytology. On the first visit, colposcopy was performed and recorded using the modified Reid Colposcopic Index. Colposcopy-directed biopsies were obtained and sent for histo-pathological studies. On a second visit, a LLETZ was performed under local anesthesia. Each specimen was marked at 12 o'clock and reported by a single Pathologist. A second expert pathologist reviewed all 62 cases blinded to the previous results. An excellent concordance between both pathologists was reported (kappa = 0.95). All margins were considered acceptable for evaluation.
Statistical analysis was performed on SPSS for Windows (version 10.00; SPSS Inc. Chicago, Ill.). Continuous variables were expressed as means and standard deviation; dichotomy variables as frequencies and percentages. To study group comparisons student´s t test for independent samples . A significant value was expressed using a two-tail p value <0.05.
¿ RESULTS
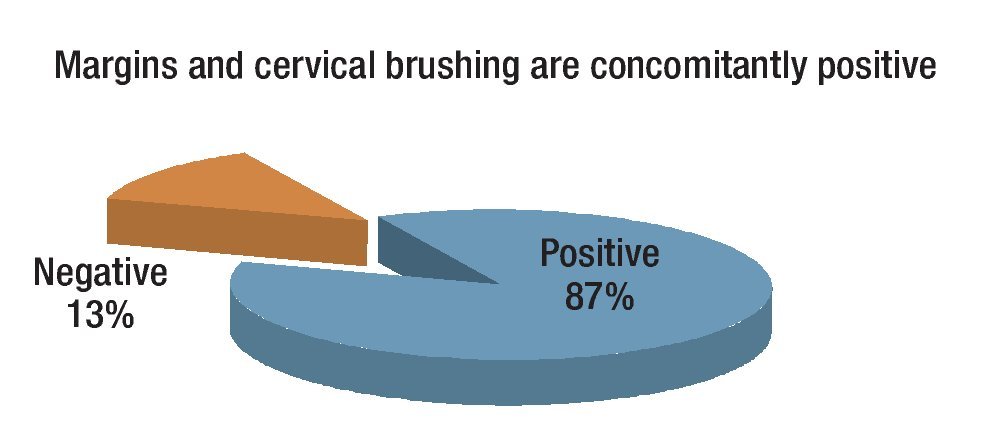
Mean age of the 344 patients with cytological and histological diagnosis of high grade intraepithelial lesion was 42.2 ± 12.5 years (range 20 - 80). The 62 cases with both positive endocervical margins and a positive cytobrush of the remaining canal had a second treatment: 46 hysterectomies and 16 second LLETZ. Findings showed 54 patients (87%) had residual lesion on the second specimen and 8 (13%) had a negative specimen (p <0.05) (Figure 1).
Figure 1. Results in 62 second specimens with both positive endocervical margins and endocervical brushing.
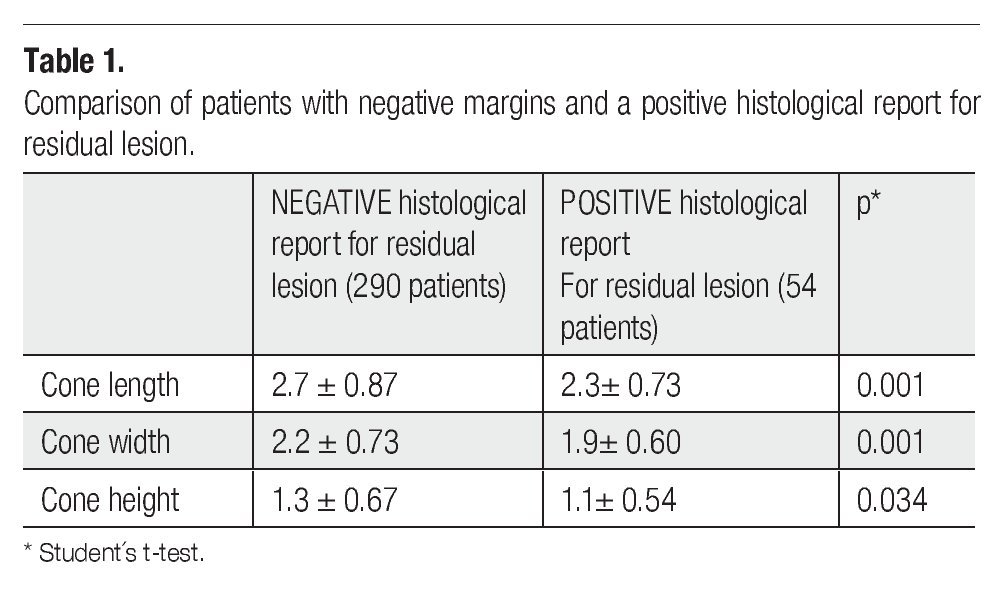
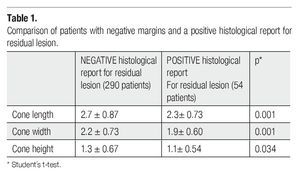
The length, height and width of the cone were significantly different in patients with residual disease when compared with those from patients with negative margins and negative endocervical brushing (Table 1).
There were no significant differences in demographic data, reproductive history, and clinical data between the group of patients with residual disease and the one with both negative margins and endocervical brushing.
¿ DISCUSSION
When the presence of a positive endocervical cytobrush and endocervical margins positive in a cone (LLETZ) specimen were combined, second specimens with residual lesion were obtained in 87% of the cases, i.e., such rate of positive specimens in the future may be predicted (positive predictive value). Residual lesion was seen in 8% of the cases (from 1817 LLETZ specimens). No other studies comparing Mexican rates have been published; however, rates reported in the international literature are quite variable (14% - 31%).18-21
¿ CONCLUSIONS
The positive predictive value of cone specimens with positive endocervical margins and concomitantly positive endocervical cytobrush of the proximal cervix is 87%. This knowledge may in the future allow choosing with reasonable certainty patients requiring a second treatment, and offering better results in the treatment of residual disease when taking into account these elegibility factors.
¿ ACKNOWLEDGMENT
To Fernando Guijon, MD for his commentaries on the manuscript and help in the translation.
Corresponding Author: Jorge Ojeda-Ortiz.
Departamento de Colpos-Departamento de Colposcopia, Hospital General de Pachuca - Carretera Pachuca-Tulancingo S/N Colonia Ciudad de los niños. Pachuca, Hidalgo. 42070, México.
Phone and Fax (52) 77 1718 2500.
Email:jorgeojeda@hotmail.com