It is well known the involvement of the gastrointestinal tract in Epidermolysis Bulhosa (EB) and its consequences on both nutrition and growth. We present a case of a young girl with EB diagnosed soon after birth, admitted to our emergency room with food impactation. The endoscopy revealed a double barrel esophagus. No medical or surgical therapy was started and after 2 months of enteric feeding, spontaneous resolution was observed at endoscopy. Skin biopsy was compatible with EB Simplex. According to the literature EB Simplex is the subtype the least associated with GI tract involvement, presenting with dysphagia in only 2% of the patients, and with the lowest cumulative risk of esophageal stricturing.
ConclusionWe present an unusual case of EB simplex involvement of the esophagus with spontaneous resolution of a false lumen, with clinical improvement of the patient.
La afectación del tracto gastrointestinal en la epidermólisis ampollosa (EA), y sus consecuencias en la nutrición y el crecimiento, es bien conocida. Se presenta el caso de una niña con diagnóstico de EA poco después del nacimiento que ingresó en nuestro servicio de urgencias con impactación de alimentos. La endoscopia reveló un esófago de doble canal. Sin tratamiento médico ni quirúrgico alguno, y tras 2 meses de alimentación entérica, se observó en la endoscopia la resolución espontánea del problema. La biopsia cutánea era compatible con la EA simple. Según las referencias bibliográficas, la EA simple es el subtipo menos asociado con afectación del tracto gastrointestinal, y solo el 2% de los pacientes presentan disfagia; además, presenta el menor riesgo acumulativo de estenosis esofágica.
Conclusiónse presenta un caso de EA simple con afectación inusual del esófago y resolución espontánea de una falsa luz, que condujo a la mejoría clínica de la paciente.
EB encompasses 4 groups of skin diseases: EB Simplex (involves intraepidermal), Junctional EB (involves the lamina lucida of the epidermal basement membrane), and dystrophic EB (involves the undersurface of the dermo-epidermal junction), which can be dominant or recessive.1,2 The dystrophic subtype, associated with a collagen VII mutation, is the most commonly observed in cases of esophageal disease and that with the most striking cumulative risk of stricture complication. The site and specific nature of the underlying mutation determines the clinical phenotype, ranging widely from a relatively mild, localized condition to a severe, generalized, mutilating disease. One of the most common sites of extracutaneous injury in inherited epidermolysis bulhosa, is the gastrointestinal tract. Blisters, erosions and scaring leading to strictures with stenosis or web formation may occur within the oral cavity, esophagus, small and large bowel, rectum and anus. Depending on the organ involved patients can experience from dysphagia, phagodynia impairing oral intake, constipation, to chronic protein and blood loss contributing to anemia, hypoalbuminemia, malabsorption and growth retardation.3,4 According to the National Epidermolysis Bullosa Registry of 2008 of the USA at least half of the cases (50 to 78%) involving the esophagus occurred in the upper third. Other esophageal problems, besides strictures, include hiatal hernia, GERD, intramural pseudodiverticula, decreased peristalsis or atony, esophagitis with gastroesophageal reflux disease (GERD) and shortening of the esophagus.5
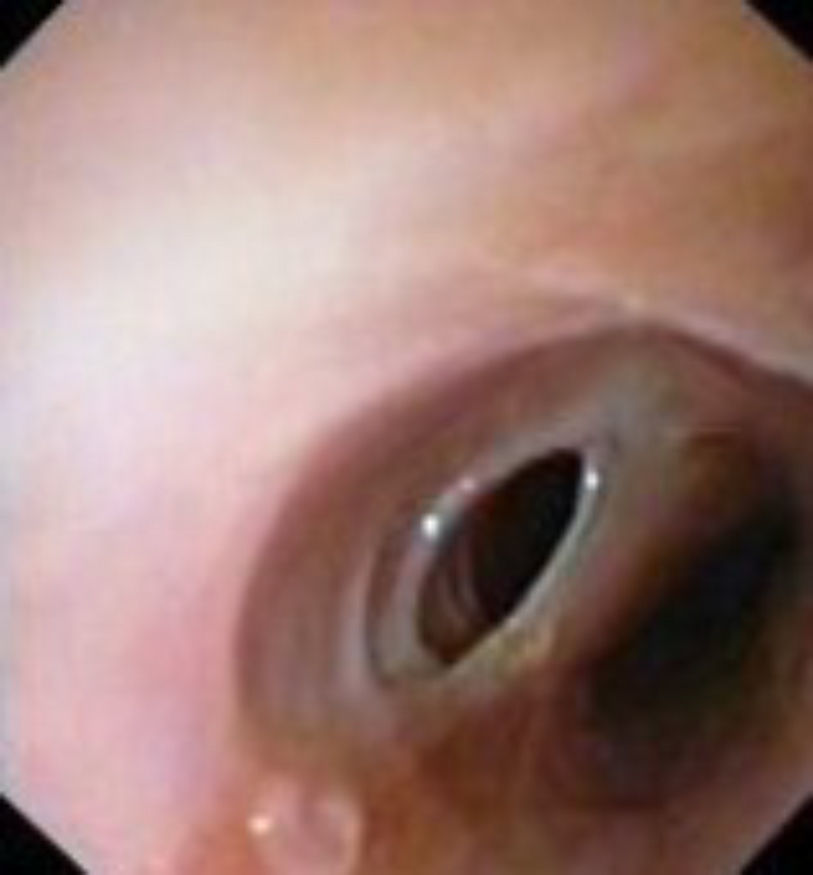
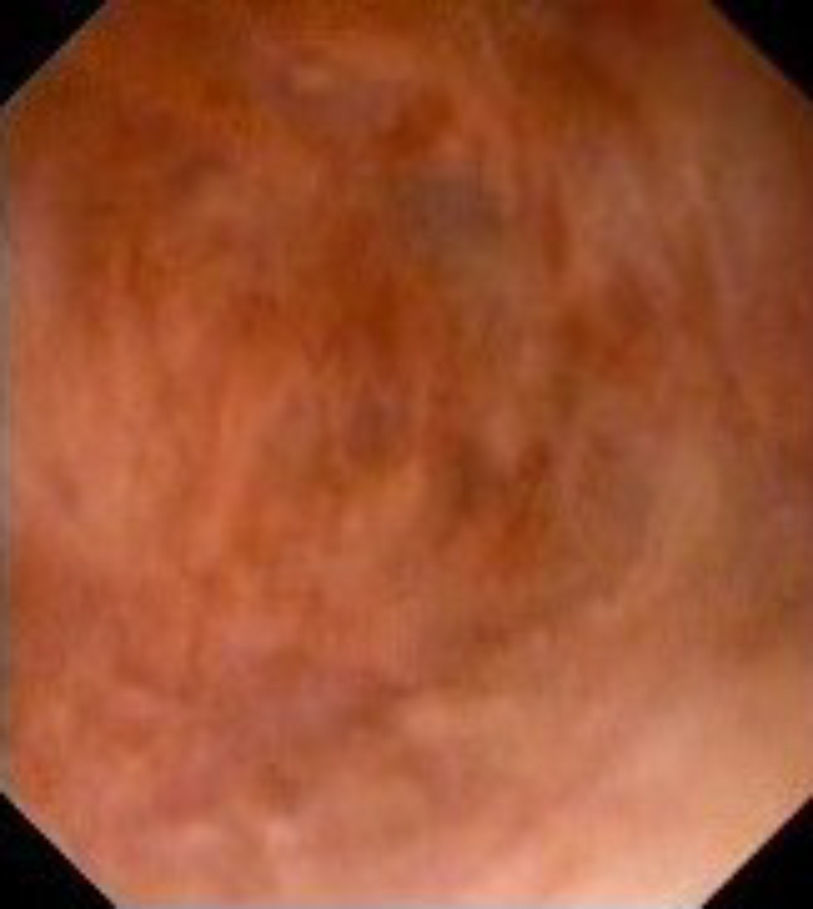
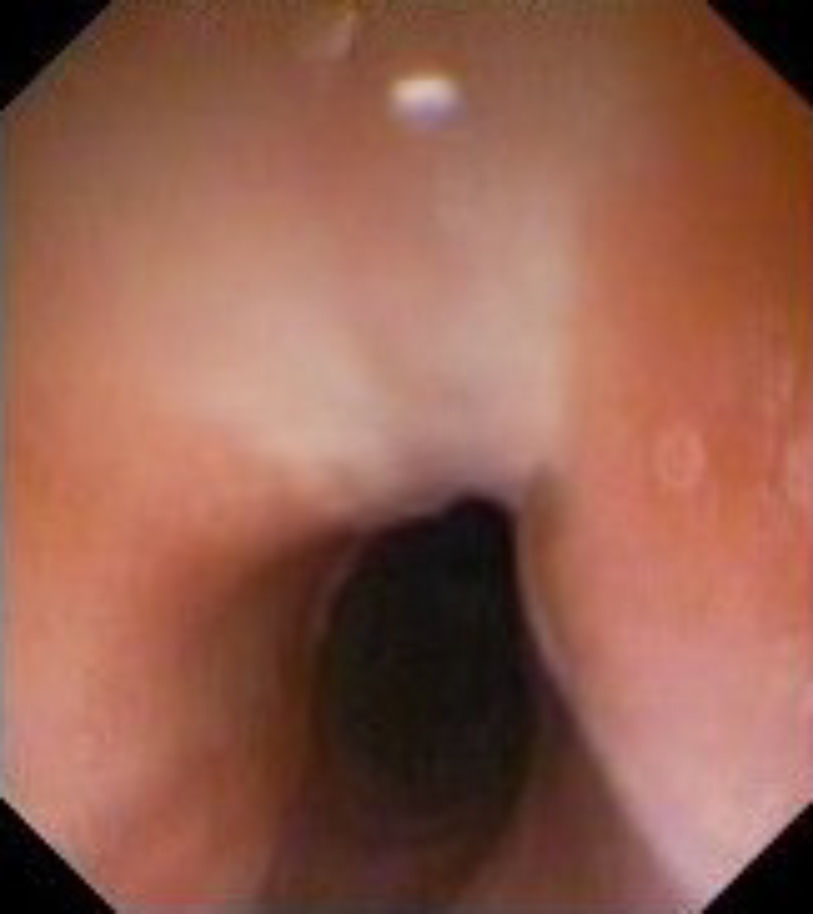
Case reportWe present the case of a 14 year old indian girl admitted to our hospital due to solid food impactation with 48hours of evolution. She had been diagnosed with EB few months after birth, while in India. By the age of ten, she came to Portugal. Parents denied consanguinity. She was under no topic antibiotic treatment. For 4 years she had been experiencing recurrent and self-limited episodes of food impactation (once a month) with occasional dysphagia with solids and early saciety, with no seek for health care services. She had not experienced puberty yet, and had never had neither involvement of the respiratory or urogenital tract, eye, ear nor alopecia. She went to the hospital less than 24hours after impactation, with chest pain not relieved with vomiting nor coughing, with normal breathing. At admission, she was hemodynamically stable with cervical pain, and mild sialorrhea, acyanotic. She presented with poor dental hygiene, mild nail dystrophy, with scars and blisters over bony prominences of the hands and feet, with itchy plaques in the legs and mild deformity of both hands and feet. (Fig. 1). Measured 1,58m and weighted 46kg (pediatric percentile 25 for stature and weight). She had generalized hypertrichosis, and no oedemas. The cervical x-ray showed no findings. A first endoscopy was tried unsuccessfully with the pediatric scope (Olympus GIF160), given major mucosal oedema and hyperaemia at lower pharynx, not overcoming the upper esophageal sphincter. In this setting it was decided to stop the procedure and repeat it 24hours later. During this period, a cervical CT scan was performed showing intraluminal assimetrical fullness localized to the left of the cervical- thoracic esophageal transition, described as food and excluded local complications. A second endoscopy was performed, 24hours later, under general anaesthesia with an ultrathin scope from Olympus (GIF 160XP) to minimize the risks and allowing to overcome the proximal oedema at the cricopharingeal muscle and considerable stricture. At 19cm from dental arcade, we observed a mucosal circumferential splitting of the proximal esophagus with a septum, membranous at its superior border. This resulted in a double barrelled esophageal deformity (Figs. 2–4). The right sided entrance led to a “false lumen” (Fig. 5), terminating after 7cm as a blind pouch. Progression was possible through the lumen to the left with the introduction of a nasogastric tube (Fig. 4). Several regular stenosis (Fig. 6) were present along the “true” esophagus, with no hiatal hernia or other blisters present; the stomach and duodenum were normal. On the other hand, during the period between endoscopies, the impactation spontaneously resolved. A nasoenteric feeding tube was left in place. No biopsies were made during this endoscopy, given the risk of complications and the patient already having a diagnosis of EB. We interpreted the false lumen as the result of a probable trauma tear, in a blistered esophageal mucosa leading to superficial dissection. The blind pouch was unlikely to be a congenital esophageal duplication, considering the upper extremity location and the age at diagnosis, since this rare disorder presents in 70 to 90% of the cases before 2 years of age, especially with respiratory symptoms.1,2,6,7 The patient was empirically started on proton pump inhibitors, because GERD is a theoretical complication that could further damage the fragile esophageal mucosa.6,8,9 After 2 months, she had a barium esophagogram done, showing no deformity left. At this time we repeated the endoscopy. In the esophagus, from 12cm to 19cm, a mucosal scar (Figs. 7–9) with some granulation tissue was observed, leading to mild stenosis, amenable with the normal caliber endoscope. Biopsies of the scar tissue revealed inflammatory unspecific infiltrate. The patient started liquid diet, with no new episodes of impact with solid food after 6 months. Skin biopsy with transmission electron microscopy was compatible with EB Simplex. EB Simplex is the subtype the least associated with GI tract involvement, presenting with dysphagia in 2% of the patients and with the lowest cumulative risk of esophageal stricturing (45 by the age of 10).
ConclusionWe presented a case of esophageal involvement by Epidermolysis Bullosa Simplex, with a false lumen created after several traumatic episodes of impactation. Spontaneous resolution with septum and wall apposition occured, developing a scar. Though, care must be taken since new episodes, or other complications, can occur in the future.