Casos Clínicos en Gastroenterología y Hepatología
Más datosEndoscopic ultrasound (EUS)-guided drainage is the preferred treatment for pancreatic fluid collections (PFCs).1–3 Denser PFCs, like walled-off pancreatic necrosis (WON), may require larger diameter stents (fully covered self-expandable metal stent—FCSEMS-), nasocystic tube placement for continuous lavage or endoscopic necrosectomy.4,5 Sometimes, symptomatic PFCs appear almost collapsed during EUS, hindering drainage. We describe an ancillary technique that may help treat those patients by refilling the PFC under EUS guidance using two cases as examples of this method.
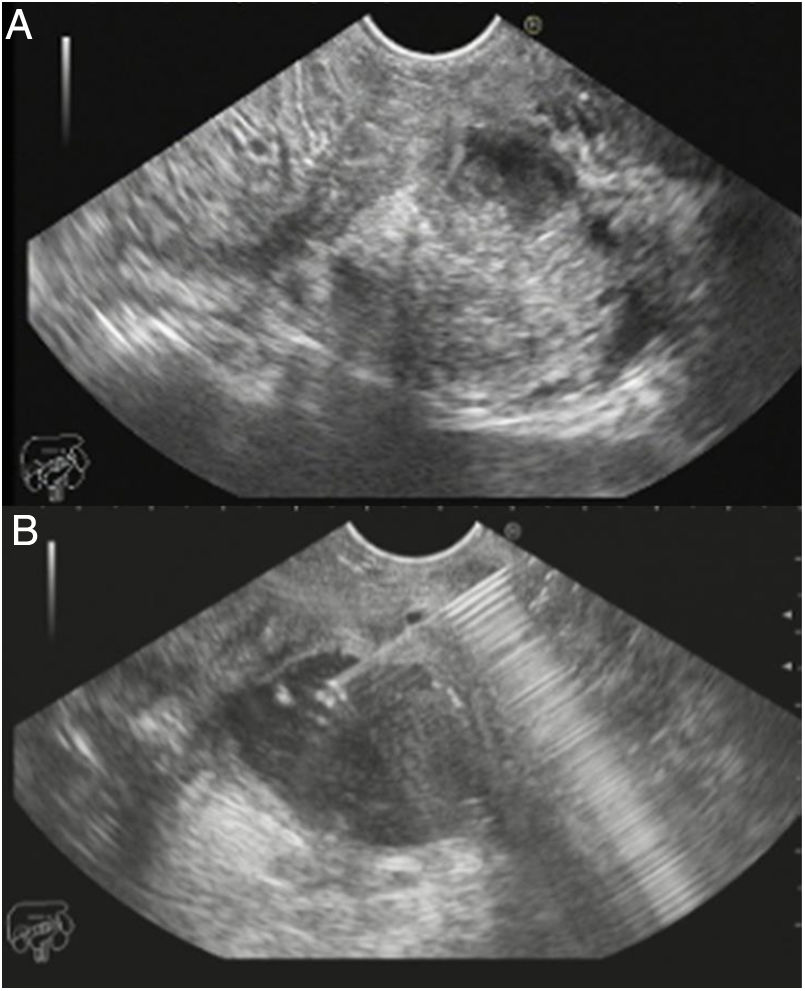
Case 1: A 67-year-old male with prior history of alcohol abuse and recurrent acute pancreatitis presented with abdominal pain and fever. He had been admitted two months before with acute pancreatitis and a 6cm PFC (mixed fluid and necrotic) and was successfully managed conservatively. Abdominal CT-scan revealed a 3cm×4cm infected WON. EUS was performed aiming at collection drainage. Unfortunately, it showed a predominantly necrotic collection with no liquid component, precluding drainage (Fig. 1A). Thus, a modified EUS-guided technique was performed. First of all, WON was punctured with a 19-Gauge needle (Cook®). Aspiration (10mL negative pressure) confirmed that fluid did not flow back. Saline solution was instilled through the needle to refill the WON, which expanded to its original size (Fig. 1B). Fluid volume needed was calculated using the equation for the volume of a sphere (v=4/3 πr3), resulting in a total of 113ml to refill the original 6cm collection. A 0.035-in. guidewire was passed and coiled into the cavity. Cut was performed using a needle-knife sphincterotome since cystotome was not available. The created tract was progressively dilated using trough-the-scope balloons (6, 8 and 10mm). A 10mm×60mm straight biliary FCSEMS (Wallflex™ Biliary Rx stent, Boston Scientifics®) and a 7Fr×7cm coaxial double pig-tail plastic stent were placed to create and fix the cyst-gastrostomy. A 7Fr nasocystic tube for continuous lavage (saline solution 500–2000mL/day) was placed for 10 days. The patient progressed favorably, complete resolution of PFC was documented at 5 months, and stents were removed.
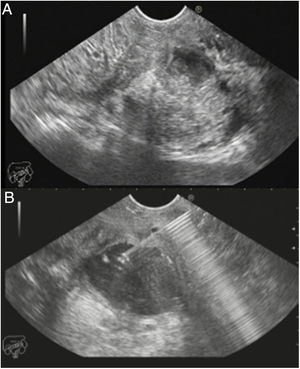
Case 2: A 74-year-old male with a history of acute biliary pancreatitis 9 weeks before and an infected WON was referred for EUS-guided drainage. He presented persistent fever, despite antibiotics, biliary sphincterotomy and common bile duct stones removal. EUS showed a poorly defined 5cm WOPN with little fluid component. Only 1.5mL of pus could be aspirated using a 19G needle. 65ml of saline solution were injected and WON re-expansion was monitored by EUS. Guidewire was then placed and coiled within the WON, and a 10mm×15mm HOT-AXIOS lumen-apposing stent (Boston Scientifics®) was inserted, creating a cyst-gastrostomy, obtaining a good clinical outcome.
EUS-guided drainage of WON may be extremely challenging, as stents may clog and become ineffective, despite necrosectomy or nasocytic lavage. Modifications of the standard EUS-guided technique have been proposed to achieve success for complex WON drainage. Varadarajulu suggested creation of multiple holes/tracts between stomach/duodenum and the WON for continuous irrigation and drainage of the collection, observing an improvement in clinical success (from 52% to 91.7%).4 Other authors proposed debridement using repeated endoscopic water-jet instillation through a 5Fr biliary catheter placed through a FCSEMS.5
We present another modification of the classical technique of PFC drainage that allowed us to successfully create a cyst-gastrostomy. In both two cases, WON was initially almost collapsed, with a minimum amount of liquid component, making it difficult even to aspirate for obtaining material for culture. As the WON was not expanded, neither guidewire, cystotome nor stent could be used to create the cyst-gastrostomy. Liquefaction of the WON by injecting saline solution was performed until enough liquid component was present to allow temporary access and further drainage placing either a FCSEMS or a lumen-apposing stent. Even if this technique might be more useful when using longer stents (metal or plastic stents) as they require more space to be advanced into the collection, in our experience, it helped us in both cases.
The amount of volume instilled was arbitrarily estimated by calculating the volume of the sphere and assuming the initial size of the PFC on CT-scan in order not to overexpand the collection. Whether this is the best method to estimate the amount of saline needed or simply EUS-monitoring during saline instillation is enough warrants further investigation. In both cases, this method allowed us to adequately distend the WON and a successful drainage. We believe this simple modification of the technique may help us treat the small percentage of patients with WON that are not amenable for EUS-guided drainage, especially those of small size and with almost no fluid component prior to drainage stent placement. To our knowledge, this simple modification of the conventional EUS-guided cyst-gastrostomy technique has not been previously reported. As it is not technically demanding, we believe it may be helpful in such difficult cases, not adding any adverse events in our experience. However, prospective and controlled studies are needed to investigate its usefulness before it can be formally recommended.
Conflicts of interestWe wish to confirm that there are no conflicts of interest associated with this publication. There has been no financial support for this work that could have influenced its outcome.