The application of vaccination programs in patients with inflammatory bowel disease (IBD) is heterogeneous and generally deficient. As a result, adherence in these patients to a predefined vaccination program has not been clearly established. The aim of this study was to estimate adherence to a predefined vaccination program among patients with IBD and to identify the factors that may predict poor adherence.
MethodsAll patients diagnosed with IBD and followed-up between January and March 2012 were referred to the Department of Preventive Medicine for evaluation of their immune status (with serological testing for hepatitis A, B and C viruses, varicella-zoster virus, mumps, rubella and measles), followed by vaccination based on the test results obtained and on the patient's vaccination history. The percentage of adherence to the vaccination program was determined, along with the factors associated with low adherence.
ResultsA total of 153 patients with IBD (ulcerative colitis in 50.3% and Crohn's disease in 49.7%) were included (45.1% men and 54.9% women; mean age 43.30±14.19 years, range 17–83). The vaccination program adherence rate was 84.3%. The factors associated with poor adherence were drugs related to IBD (patients not receiving immunosuppressants and/or biological agents showed lower adherence than those receiving these treatments; p=0.021), adherence to medical treatment (poor adherence to treatment was also associated with poor adherence to vaccination; p=0.016), and marital status (single, divorced or separated patients showed lower adherence than married individuals; p=0.015).
ConclusionAdherence to vaccination is acceptable among patients with IBD. However, specific actions, such as optimization of patient information on the disease and emphasis on the need for adequate vaccination, are to improve adherence.
La implantación de programas de vacunación en pacientes con enfermedad inflamatoria intestinal (EII) es heterogénea y en general, deficiente, por lo que no es bien conocida la adherencia de nuestros pacientes con EII a un programa de vacunación previamente establecido. El objetivo fue determinar la adherencia a un programa de vacunación establecido en nuestro centro en pacientes con diagnóstico de EII y definir qué factores pueden predecir una baja adherencia a dicho programa.
Material y métodosSe derivaron al Servicio de Medicina Preventiva todos los pacientes con diagnóstico de EII revisados en consulta entre enero y marzo de 2012, con el fin de determinar su estado de inmunización (mediante la extracción de analítica con serologías del virus de la hepatitis A, B y C, virus varicela-zoster, parotiditis, rubeola y sarampión) y, posteriormente, ser vacunados teniendo en cuenta sus resultados así como el calendario vacunal previo. Se determinó el porcentaje de adherencia a dicho programa así como los factores relacionados con una baja adherencia.
ResultadosSe incluyeron 153 pacientes (45.1% hombres y 54.9% mujeres, con una edad media de 43.30±14.19 años, rango 17-83) con diagnóstico de EII (50.3% colitis ulcerosa y 49.7% enfermedad de Crohn). La adherencia al programa de vacunación fue del 84.3%. Los factores que se asociaron con una baja adherencia fueron: fármacos en relación con la EII (los pacientes que no tomaban inmunosupresores y/o biológicos presentaron una menor adherencia frente aquellos que sí los recibían, p 0.021), adherencia al tratamiento médico (aquellos con mala adherencia al tratamiento presentaron también baja adherencia a la vacunación, p 0.016), estado civil (solteros, divorciados o separados presentaron menor adherencia respecto a los casados, p 0.015).
ConclusiónLa adherencia a la vacunación no es adecuada en pacientes con EII. Acciones específicas como la optimización de la información que se le proporciona al paciente acerca de su enfermedad y la necesidad de una adecuada vacunación, constituye un pilar fundamental para lograr mejorarla.
Patients with inflammatory bowel disease (IBD) are exposed to the same infections as the general population. The use of drugs such as corticosteroids, immunosuppressants and/or biological agents in patients with IBD can increase the risk of opportunistic infections and infectious complications. In the follow-up of patients with IBD, their immune competence can become immune deficiency if they need immunomodulator therapy to treat a flare-up or complications of IBD. Since these kinds of situations are not predictable, all patients with IBD are candidates for immunization through vaccination programs. Thus, immunization should be performed as soon as possible, and preferably at the time of diagnosis of the disease. Vaccines are generally safe in these patients, and their use is not associated to an increased risk of disease relapse. However, in clinical practice, the implementation of vaccination programs in patients with IBD is heterogeneous and generally deficient. As a result, the adherence of such patients to a predefined vaccination program has not been clearly established.
AimsThe present study was carried out to determine adherence to a predefined vaccination program among patients with IBD in our center, and to identify the factors that may predict deficient adherence.
Material and methodsA prospective observational study was designed. Initially, a vaccination program was developed along with the Department of Preventive Medicine and the Department of Digestive Diseases of Reina Sofía University Hospital (Córdoba, Spain). The study included patients diagnosed with IBD (ulcerative colitis or Crohn's disease) and followed-up between January and March 2012, consecutively. The patients received a verbal and written explanation (Patient Information Sheet) of the need for vaccination, and informed consent was obtained for inclusion in the program. The inclusion criteria were a recent or established diagnosis of IBD (ulcerative colitis or Crohn's disease) and a patient age of 14 years or older. Patients failing to give informed consent for inclusion in the vaccination program were excluded from the study.
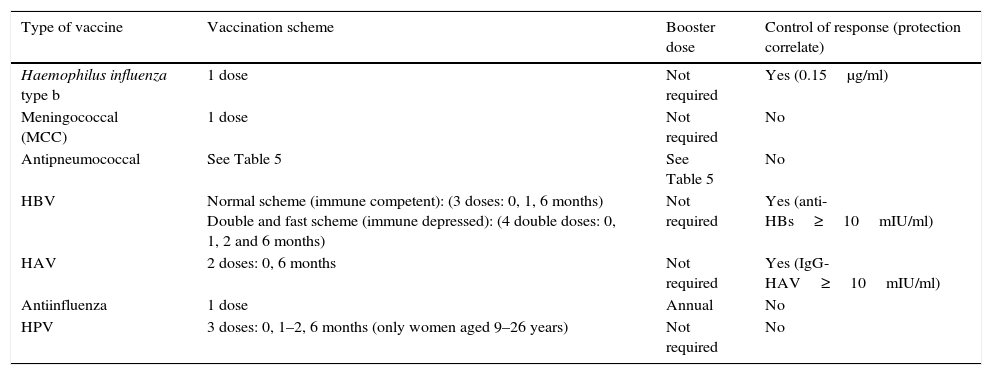
All patients underwent serological testing for hepatitis A, B and C viruses, varicella-zoster virus, mumps, rubella and measles, in order to establish their immunization status. The patients were then evaluated by the specialist in the Department of Preventive Medicine, and the vaccines defined in the program were administered according to the observed immunization status, vaccination history and prescribed drug treatments (Tables 1 and 2).
Vaccination schemes indicated in patients with inflammatory bowel disease.
| Type of vaccine | Vaccination scheme | Booster dose | Control of response (protection correlate) |
|---|---|---|---|
| Haemophilus influenza type b | 1 dose | Not required | Yes (0.15μg/ml) |
| Meningococcal (MCC) | 1 dose | Not required | No |
| Antipneumococcal | See Table 5 | See Table 5 | No |
| HBV | Normal scheme (immune competent): (3 doses: 0, 1, 6 months) Double and fast scheme (immune depressed): (4 double doses: 0, 1, 2 and 6 months) | Not required | Yes (anti-HBs≥10mIU/ml) |
| HAV | 2 doses: 0, 6 months | Not required | Yes (IgG-HAV≥10mIU/ml) |
| Antiinfluenza | 1 dose | Annual | No |
| HPV | 3 doses: 0, 1–2, 6 months (only women aged 9–26 years) | Not required | No |
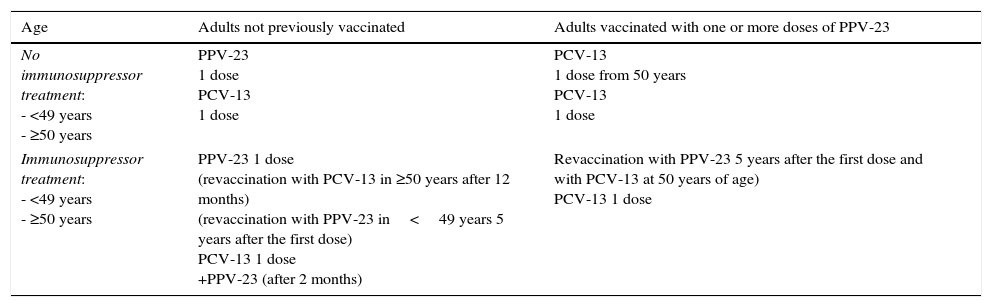
Type of antipneumococcal vaccine and administration schemes in patients with inflammatory bowel disease.
| Age | Adults not previously vaccinated | Adults vaccinated with one or more doses of PPV-23 |
|---|---|---|
| No immunosuppressor treatment: - <49 years - ≥50 years | PPV-23 1 dose PCV-13 1 dose | PCV-13 1 dose from 50 years PCV-13 1 dose |
| Immunosuppressor treatment: - <49 years - ≥50 years | PPV-23 1 dose (revaccination with PCV-13 in ≥50 years after 12 months) (revaccination with PPV-23 in<49 years 5 years after the first dose) PCV-13 1 dose +PPV-23 (after 2 months) | Revaccination with PPV-23 5 years after the first dose and with PCV-13 at 50 years of age) PCV-13 1 dose |
In order to avoid numerous hospital visits and possible patient losses, all patients were seen in the Department of Preventive Medicine on the same day as the scheduled follow-up visit to the IBD outpatient.
The sociodemographic features (age, gender, place of residence, educational level, employment status, marital status, smoking habits, offspring and previous vaccinations) were recorded, together with information on the disease (time from diagnosis, type of disorder, location and activity of the disease, presence of perianal disease, extraintestinal manifestations or complications of IBD, comorbidities, need for surgery and treatments received, as well as adherence to therapy) and factors associated to the physician–patient relationship. The concept of adhesion includes active and informed patient participation in the decision to start the vaccination protocol, i.e., reporting to consultation in the Department of Preventive Medicine, with administration of the recommended vaccines. Good adherence means that the patient and physician collaborate with a common purpose, and that patient opinion is taken into account in the medical decisions. The physician–patient relationship was classified as good, acceptable or poor, by a patient interview. Specifically, a good relationship is considered when the patient feels that the physician explains the prescribed treatments and recommendations, and understands and accepts them. An acceptable relationship is defined when the physician explains the prescribed treatments and recommendations, but in such a way that the patient is unable to understand them. In turn, a poor relationship is when the physician fails to explain the prescribed treatments and recommendations.
The sociodemographic data were collected by patient interview (following the obtainment of informed consent) in the IBD clinic. The data related to the bowel disease were obtained from the local ENEIDA database and from medical records. The data regarding to the physician–patient relationship were obtained from a telephone interview with each patient included in the study. This interview was carried out by a nurse unrelated to the study, in order to avoid influencing the patient response.
Adhesion to the vaccination program was assessed by consulting the Diraya (Patients Medical Registry) database to document the patients that had reported to their visits to the Department of Preventive Medicine and had received the recommended vaccines. Patients who failed to report to the visits to the Department of Preventive Medicine were contacted to know the reasons for non-adhesion (forgotten appointment, fear of needles, fear of undesired effects of the vaccines, lack of information, etc.).
A first descriptive analysis was made, reporting the qualitative variables as proportions and frequencies, while quantitative variables were reported as the mean and standard deviation in the case of a normal distribution, and as the median and range in the case of a non-normal distribution. Secondly, a comparative analysis was performed using the appropriate statistical tests for contrasting quantitative and qualitative variables, with the application of nonparametric tests as required. Two-tailed comparative tests were used in all cases, and statistical significance was considered for p<0.05. A multivariate analysis was carried out to determine which parameters were predictive of low adherence to the vaccination program, and for controlling possible confounding variables. The GStat 2 statistical package was used for the analysis of results.
The study was approved by the local Ethics Committee.
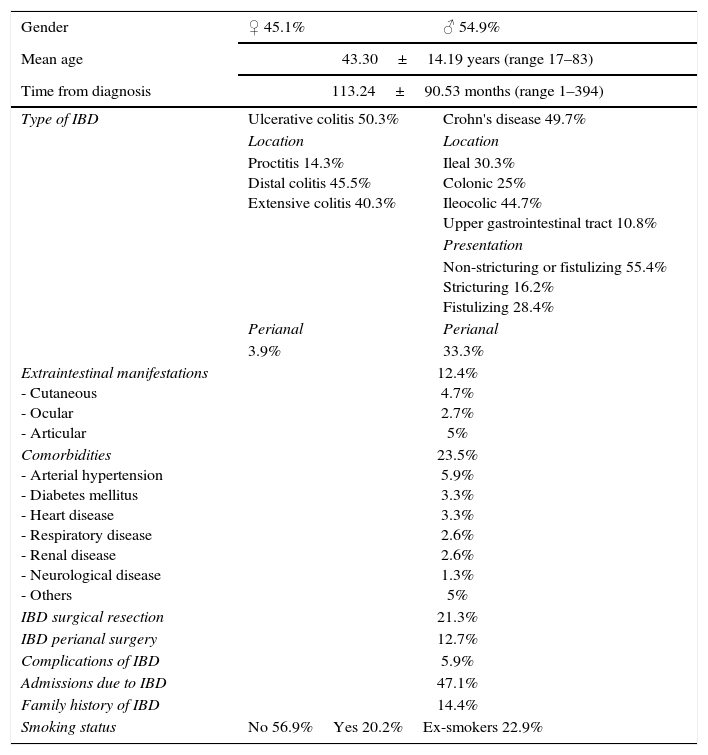
ResultsA total of 153 patients with IBD were included in the study (45.1% males and 54.9% females), with a mean age of 43.30±14.19 years (range 17–83). The mean time from the diagnosis of IBD was 113.24±90.53 months (range 1–394). 50.3% of patients had ulcerative colitis (14.3% ulcerative proctitis, 45.4% distal colitis and 40.3% extensive colitis), while 49.7% had Crohn's disease (30.3% ileal, 25% colonic, 44.7% ileocolic, 10.8% upper digestive tube disease). In turn, 12.4% of the patients had extraintestinal manifestations (particularly joint affections), 23.5% had any comorbidity associated (mean number of comorbidities 1.5±0.81, range 1–4), 5.9% had developed a complication of the disease (being the most common intra-abdominal abscess), and 29.4% had required surgery related to IBD (21.3% surgical resection and 12.7% surgery for perianal disease). A total of 72 patients (47.1%) had required any hospital admission because of the disease. A family history of IBD was present in 14.4% of the patients, and 20.2% were smokers (22.9% ex-smokers and 56.9% non-smokers) (Table 3).
Descriptive analysis.
| Gender | ♀ 45.1% | ♂ 54.9% |
|---|---|---|
| Mean age | 43.30±14.19 years (range 17–83) | |
| Time from diagnosis | 113.24±90.53 months (range 1–394) | |
| Type of IBD | Ulcerative colitis 50.3% | Crohn's disease 49.7% |
| Location | Location | |
| Proctitis 14.3% Distal colitis 45.5% Extensive colitis 40.3% | Ileal 30.3% Colonic 25% Ileocolic 44.7% Upper gastrointestinal tract 10.8% | |
| Presentation | ||
| Non-stricturing or fistulizing 55.4% Stricturing 16.2% Fistulizing 28.4% | ||
| Perianal | Perianal | |
| 3.9% | 33.3% | |
| Extraintestinal manifestations - Cutaneous - Ocular - Articular | 12.4% 4.7% 2.7% 5% | |
| Comorbidities - Arterial hypertension - Diabetes mellitus - Heart disease - Respiratory disease - Renal disease - Neurological disease - Others | 23.5% 5.9% 3.3% 3.3% 2.6% 2.6% 1.3% 5% | |
| IBD surgical resection | 21.3% | |
| IBD perianal surgery | 12.7% | |
| Complications of IBD | 5.9% | |
| Admissions due to IBD | 47.1% | |
| Family history of IBD | 14.4% | |
| Smoking status | No 56.9%Yes 20.2%Ex-smokers 22.9% | |
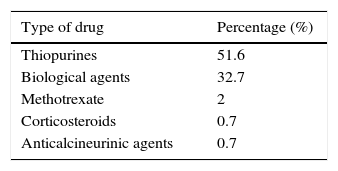
At the time of referral to the Department of Preventive Medicine, 86.3% of the patients were in remission, and 106 (69.3%) presented immune suppression associated to the therapy (51.6% were receiving thiopurine drugs, 32.7% biological agents, 2% methotrexate, 0.7% anticalcineurinic agents and 0.7% corticosteroids at a dose of over 20mg/day) (Table 4).
Thirteen patients (8.5%) developed infectious complications of IBD in the course of the disease. The most frequent were skin infections (53.8%) (5 patients developed herpes simplex virus infection, one presented human papillomavirus infection, and another one suffered skin rash related to measles), followed by respiratory infections (30.8%) (4 subjects were diagnosed with pneumococcal respiratory disease) and urinary infections in two patients (15.4%).
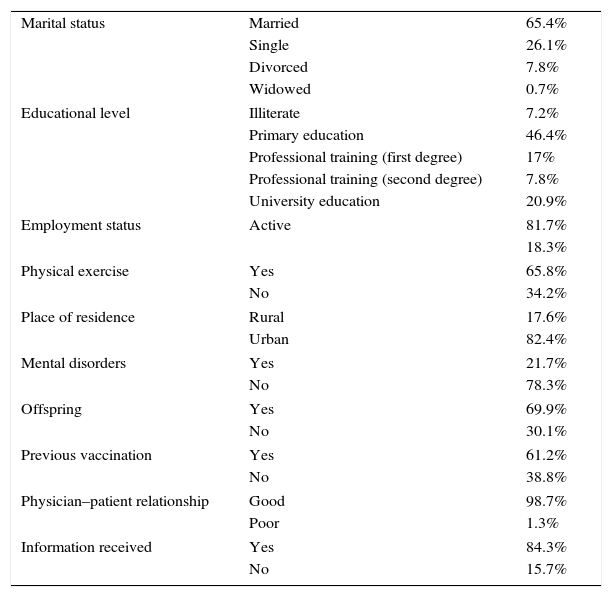
Evaluation of adhesion to the vaccination program showed that 84.3% of the patients had attended to the Department of Preventive Medicine and had received the recommended vaccines. The most frequent reason for non-adherence was a lack of information on vaccination (58.4%), followed by forgotten appointments (20.8%), fear of needles (12.5%), and transport problems among patients living far from the hospital (8.3%). Other sociodemographic factors possibly related to adherence were also evaluated, such as marital status, educational level, employment status, physical exercise, place of residence, history of mental disorders, offspring, previous vaccination, and information received (Table 5).
Patient sociodemographic data.
| Marital status | Married | 65.4% |
| Single | 26.1% | |
| Divorced | 7.8% | |
| Widowed | 0.7% | |
| Educational level | Illiterate | 7.2% |
| Primary education | 46.4% | |
| Professional training (first degree) | 17% | |
| Professional training (second degree) | 7.8% | |
| University education | 20.9% | |
| Employment status | Active | 81.7% |
| 18.3% | ||
| Physical exercise | Yes | 65.8% |
| No | 34.2% | |
| Place of residence | Rural | 17.6% |
| Urban | 82.4% | |
| Mental disorders | Yes | 21.7% |
| No | 78.3% | |
| Offspring | Yes | 69.9% |
| No | 30.1% | |
| Previous vaccination | Yes | 61.2% |
| No | 38.8% | |
| Physician–patient relationship | Good | 98.7% |
| Poor | 1.3% | |
| Information received | Yes | 84.3% |
| No | 15.7% | |
The rate of patient adherence to follow-up in the IBD clinic and to the treatment received was very high (97.4%).
Regarding the serological findings, 19.9% of the patients presented immunization (IgG) to hepatitis A virus (HAV), 0.7% showed antibodies against hepatitis C virus (HCV) (one patient suffered chronic HCV infection), 1.5% resulted positive for hepatitis B virus (HBV) surface antigen, 55.1% had antibodies against HBV surface antigen, and 9.6% had antibodies against HBV core antigen (2 patients suffered chronic HBV infection). A total of 80.1% of the patients were immunized against mumps, 88.2% against rubella, 92.6% against varicella-zoster virus, and 99.3% against measles (one patient suffered acute measles infection).
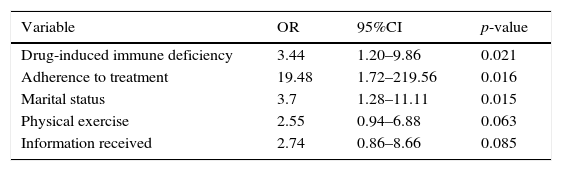
The factors associated to low adherence in the multivariate analysis were the drugs used by the patients (subjects not receiving immunosuppressants and/or biological agents showed lower adherence than those who received such treatments; p=0.021), adherence to medical treatment (poor adherence to treatment was also associated to poor adherence to vaccination; p=0.016), and marital status (single, divorced or separated patients showed lesser adherence than married individuals; p=0.015). Physical exercise and a lack of information reached values close to statistical significance (p=0.063 and p=0.085, respectively) (Table 6).
Multiple logistic regression analysis.
| Variable | OR | 95%CI | p-value |
|---|---|---|---|
| Drug-induced immune deficiency | 3.44 | 1.20–9.86 | 0.021 |
| Adherence to treatment | 19.48 | 1.72–219.56 | 0.016 |
| Marital status | 3.7 | 1.28–11.11 | 0.015 |
| Physical exercise | 2.55 | 0.94–6.88 | 0.063 |
| Information received | 2.74 | 0.86–8.66 | 0.085 |
Likelihood ratio=21.34; p<0.0007; df=5; Nagelkerke R2=0.22.
Patients with inflammatory bowel disease (IBD) are more susceptible to certain infections than the general population, though the true incidence is not known. This lack of information is due to the fact that there are no quality prospective studies in this field offering a global assessment of patients with IBD, independently of the treatment received. Moreover, the available studies are very heterogeneous in terms of the type of infections considered (opportunistic, serious, postoperative, etc.).1–4 In clinical practice is well known that infectious complications are important in these patients, and can adversely affect their quality of life. On the other hand, infections are among the five leading causes of death in patients with IBD.5
The risk of infection appears to be related to addition of several risk factors both specific and nonspecific of IBD.6–7 Among the infection risk factors specific of IBD, mention must be made of a potential alteration in innate immune response to microorganisms, and the prescribed immunomodulator treatment. Furthermore, patient age, comorbidities, malnutrition and exposure to pathogens are some of the factors not specific of IBD. For many years, immunosuppressor treatment was believed to be the only implicated factor. As a result, most studies in the literature focus on drug substances, and pay little attention to other important risk factors.1,8
There are very few specific vaccination recommendations in IBD. In the year 2009, the European Crohn's and Colitis Organization (ECCO) published a consensus document on the prevention of opportunistic infections in IBD.6 On the other hand, different groups in the United States have developed vaccination guidelines in IBD.9–11 For example, the guidelines of Sands et al. and Melmed et al. are focused on immune compromised patients with IBD, while the recommendations of Wasan et al. are referred to the global IBD population. The lack of an unique guide on vaccination in IBD means that no absolute vaccination indications can be established in patients of this kind, and that the guidelines on vaccination applicable to the general adult population must be used as reference.11–13 Despite the existing guidelines and consensus documents on vaccination indications in these patients as a primary prevention strategy, the vaccination coverage rates achieved are low. This is probably because of a lack of perceived infection risk and doubts on vaccine efficacy and safety in these cases.
In Spain, in the same way as in other European countries and the United States, vaccination against preventable infections in immune compromised adults refers to influenza, tetanus, diphtheria, hepatitis A and B, infection due to Streptococcus pneumoniae, infection due to Neisseria meningitidis C, infection due to Haemophilus influenza type b, varicella, measles and human papillomavirus (HPV) infection.11,14 Vaccines composed of attenuated live microorganisms are contraindicated in immune depressed individuals.
Currently, most groups in IBD agree that all patients with IBD can benefit from immunization. Although immune compromised patients theoretically are most benefited individuals from vaccination, the risk of eventually suffering immune depression even in patients with apparently banal IBD is not negligible.6,9,15 For this reason, whenever possible, vaccination should take place before immune depression is reached, in order to secure a greater serological response. However, at present the implementation of vaccination programs in these patients is heterogeneous and generally deficient, and although there is a tendency to believe that adherence to vaccination among these patients is similar to their adhesion to treatment for IBD (different authors having reported non-adherence rates of 39–72%), the fact is that the true adherence to predefined vaccination programs in patients with IBD is unknown.16–23 For this reason, our study was designed to evaluate adherence to a vaccination program among patients with IBD – the observed adherence rate being about 84%. Different factors are involved in the adherence. On one hand, the patient characteristics (i.e., the type of patient) play a role, in the same way as the characteristics of the disease and the complexity of its treatment. Another important influencing factor is the physician–patient relationship.24 In effect, a good physician–patient relationship stimulates adherence. Such relationships are complex and involve two different people that may have different opinions referred to health matters. A poor physician–patient relationship adversely affects patient satisfaction, thereby worsening adherence and resulting in negative health consequences.
To date, no similar studies have been published on adherence to vaccination in patients with IBD or on the factors associated to low adherence. In our study, deficient adherence was associated to the drugs used by the patient (with improved adherence in patients receiving more complex treatments such as immunosuppressants and/or biological agents), adherence to medical treatment (patients with poor adherence to treatment for IBD also showed poorer adherence to vaccination) and marital status (married patients showed better adherence than single or divorced subjects). Physical exercise almost reached statistical significance (p=0.063) (adherence to vaccination being poorer in the absence of physical exercise), in the same way as the information received (p=0.085) (adherence being poorer among the patients who claimed to have received no information). No studies on adherence to vaccination in IBD are available for comparison purposes, though there are data on adherence to medication among such patients. In this way, Goodhand et al. and Kamperidis et al. found non-adherence to medication in patients with IBD to be associated to factors such as age, low socioeconomic level and depressive states.25–26 In a systematic review published in 2010 by Jackson et al., reported non-adherence to medication in patients with IBD was associated to patient beliefs referred to drug treatment, patient mental condition, and a poor physician–patient relationship.27
A proper knowledge of the factors conditioning low adherence will make it possible to develop educational strategies that optimize the adhesion. Such strategies may include available written information with verbal reinforcement; medical education programs and informative leaflets on IBD; the placing of emphasis on the potential benefits of vaccination (e.g., the prevention of different infections); patient association activities (e.g., participation in meetings or discussions); or recommendation of websites interesting for the patients.
The main limitation of this study is the fact that some data were collected from telephone interviews with the patients. In this regard, patients with low adherence might also be scantly cooperative in conducting these interviews. On the other hand, a letter with the appointment for reporting to the Department of Preventive Medicine was sent to the patients by mail, and some of them may have failed to visit the center because the letter did not reach them or because they simply did not remember the visit. As a result, some patients may have been wrongly classified as showing poor adhesion. However, in order to eliminate this possible source of bias, all patients were contacted by telephone to make sure that they had received the letter and knew the date and time of the visit.
In conclusion, adherence to vaccination is acceptable among patients with IBD but it can be improved by specific actions. Considering the importance of vaccination for preventing infections and therefore for improving patient quality of life, attempts must be made to detect and correct poor adherence. Specific actions, such as the optimization of patient information on the disease and emphasis on the need for adequate vaccination, are crucial in order to improve adherence.
Conflict of interestV García-Sánchez has served as a speaker, a consultant and advisory member for MSD, Abbvie, Ferring and Otsuka Pharmaceutical, and has received research funding from MSD and Abbvie.