Developmental abnormalities of the gallbladder are relatively rare. Although often asymptomatic, agenesis of the gallbladder can present symptoms, such as dyspepsia, abdominal pain, nausea and vomiting, intolerance to fatty foods, and so on. It has been reported to be associated with gastrointestinal, cardiovascular, genitourinary, and skeletal malformations.
We report a case of a patient who was a candidate for cholecystectomy for suspected sclerotic and atrophic gallbladder. During laparoscopy it was diagnosed as hypoplasia/agenesis of the gallbladder.
Isolated agenesis of the gallbladder is a rare congenital anomaly that results from failure of the cystic bud to develop in utero. Since its first description by Lemery in 1701, a number of cases have been published, with a reported incidence of 0.01–0.06%.1
Combined with the rarity of the condition, the diagnosis is infrequently made preoperatively, and so the patient undergoes unnecessary operative intervention. Intraoperatively, the risk of iatrogenic injury is higher, and so the associated morbidity of the procedure is greater.2
Case presentationA 53-year-old woman presented us with a history of dyspeptic syndrome, right upper quadrant abdominal pain, and a history of fatty food intolerance. She denied febrile episodes, and physical examination was unremarkable. On ultrasound examination, performed in another institution, the gallbladder was not visualized, but strong echoes with acoustic shadowing were seen, suggesting a contracted gallbladder or a gallbladder scleroatrophy with possible presence of microlithiasis. The laboratory tests carried out were all normal. The patient was sent to operating room to undergo cholecystectomy.
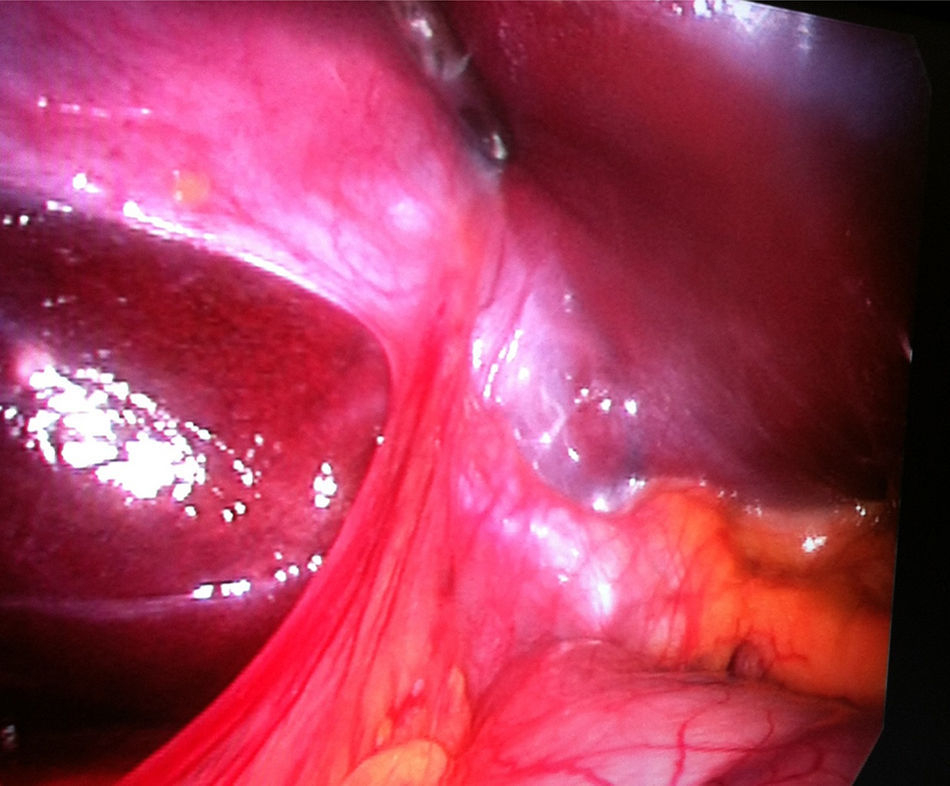
At laparoscopy, a small fibrous remnant was seen in the gallbladder fossa (Fig. 1), but the gallbladder could not be found despite an extensive search of all possible ectopic sites. Small fibrous remnant was resected and common bile duct properly identified.
Post-operatively, she made an uneventful recovery, and remains symptom free.
DiscussionThe liver, gallbladder, and biliary system begin to develop early in the fourth week of intrauterine life as a ventral outgrowth from the caudal part of the foregut. This hepatic diverticulum divides into two parts as it grows, one representing the primordium of the liver, and the other, the primordium of the gallbladder and cystic duct. By the seventh week, from the pars cystic, a vacuole and a shalk had developed, which respectively represent the gallbladder and the cystic duct. In the first stage, the gallbladder is a hollow organ, even if the proliferation of its epithelium determines a phase in which its cavity is temporarily canceled; subsequently, through the vacuolation of its epithelium, it again becomes a hollow organ.3 Failure of this developmental process at any stage results in agenesis of the gallbladder, whereas inappropriate migration of the gallbladder primordium will result in an ectopic gallbladder. Potential sites of ectopic gallbladder are intra-hepatic, left-sided, beneath the posterior inferior surface of liver, between the leaves of the lesser omentum, within the falciform ligament, retroperitoneal, retrohepatic, or in the retropancreatic and retroduodenal areas.4
Gallbladder agenesis (GA) is a rare congenital anomaly characterized by the absence of the gallbladder in conjunction with a normal bile duct system.5 It can be observed in both children and adults, with a median age of 46 years at the time of diagnosis.
It is almost always an incidental finding of the abdominal surgery or a finding at autopsy. It has a lower incidence in surgical cholecystectomy series (0.007–0.027%) than that in autopsy reports (0.04–0.13%). The prevalence range is 0.007–0.13%.6
GA is often associated with other congenital abnormalities (12.8–30%). It has been reported to be associated with gastrointestinal, cardiovascular, genitourinary, and skeletal malformations, such as duodenal atresia, malrotation of the gut, pancreas divisum, imperforate anus, hypoplasia of the right hepatic lobe, duplication cysts of the hepatic flexure, ventricular septal defect, renal agenesis, undescended testes, and syndactyly.7 In particular, some authors report genitourinary anomalies as most frequently associated with GA.
The occurrence of the pathology is most often sporadic; however, there are reports of families where several members are affected by this condition, and this suggests the possible existence of hereditary forms.3 GA has also been reported in association with congenital syndromes, trisomy 18 and with congenital malformations caused by thalidomide.6
Clinically, three groups of presentation of gallbladder agenesis have been described1: (1) asymptomatic (an incidental finding at laparotomy for another reason) (35%), (2) symptomatic (50%), in children with multiple fetal anomalies (such as tetralogy of Fallot and agenesis of the lungs), and (3) children who die in the perinatal period (15–16%). Common symptoms include: right upper quadrant abdominal pain (90%), nausea and vomiting (66%), fatty food intolerance (37%), dyspepsia (30%), and jaundice (35%).4,6 Moreover, bile duct stones are found in 25–60% of symptomatic patients.3 Most of these symptoms of GA may be explained as being associated with stasis in the bile duct (often dilated and taking on the function of bile storage), which can produce the clinical features of cholecystitis, cholangitis, and choledocholithiasis.5 It has previously been suggested that the pathophysiology of symptoms in gallbladder agenesis is similar to that of the post-cholecystectomy syndrome, and it is thought that the causes of pain include biliary dyskinesia and choledocholithiasis.8
The usual initial investigation for patients presenting right upper quadrant pain is an abdominal ultrasound. It has been suggested that the absence of the ultrasonographic features of the WES triad (visualization of the gallbladder wall, the echo of the stone, and the acoustic shadow) and the double-arc shadow should raise suspicion of gallbladder agenesis as the diagnosis.
Despite the high resolution of diagnostic imaging techniques, it has proven to be very difficult to make a correct preoperative diagnosis of GA in symptomatic patients. In fact, lots of “laparoscopic” diagnoses are reported in the literature.2,5 If the diagnosis of GA is made during operation, the surgeon must prove GA by examining the most common sites for ectopic gallbladder and it is suggested to abort the procedure rather than complete further exploration (Fig. 1).
Abdominal ultrasound has a reported sensitivity of 95% in diagnosing gallstones but it is dependent on many factors, including the operator's experience and the examination conditions. Furthermore, shadowy opacities thought to represent gallstones could actually be due to intestinal gas artifact, periportal tissue, or subhepatic peritoneal folds, leading to false-positive findings. Various authors have found ultrasound (US) scan to be misleading in interpreting a contracted and fibrotic gallbladder; therefore, most symptomatic patients are scheduled for surgery with a diagnosis of chronic cholecystitis with a contracted fibrosed gallbladder and a normal biliary tract.9 Effectively a small, contracted (shrunken, scarred, sclerotic, or atrophied) gallbladder associated with stones and chronic cholecystitis will be difficult to visualize and US scan is highly operator-dependent.3,5
Significant progress in radiology and widespread availability of non-invasive imaging techniques such as computed tomography has taken place in the last few years. However, non-visualization of the gallbladder is commonly attributed to an obstructed cystic duct, anatomic variations, or technical errors (as in our case), and agenesis of the gallbladder is considered the least likely explanation.
Magnetic resonance cholangiopancreatography (MRCP) and endoscopic ultrasound (EUS) provide excellent alternatives to open exploration and intra-operative cholangiography,9 but neither are usually used because they are only indicated when suspected diagnosis is not clear. In particular, MRCP is considered the test of choice if there is suspicion, and it is also helpful in demonstrating an ectopic gallbladder along with other possible anomalies of the biliary tract system. Moreover, as it does not require contrast administration to visualize the bile, it is not compromised by biliary stasis.7
If the diagnosis is made pre-operatively or the symptoms continue postoperatively, a possible conservative treatment for this symptomatic group includes smooth muscle relaxants, and if this fails, sphincterotomy.9
In any case, if the diagnosis is made during surgery, the operative strategy is finalized to exclude an aberrant gallbladder, and the diagnosis should be reconfirmed postoperatively by careful US scan.3
The majority of the patients reported in the literature became asymptomatic after the surgical procedures, even after nontherapeutic surgery. This is probably due to the lysis of the periportal and right hypochondrial adhesions3 even though it remains unclear whether these patients would have had symptom resolution in the absence of exploration.
Importantly, laparotomy is not indicated if this benign condition is diagnosed pre-operatively.
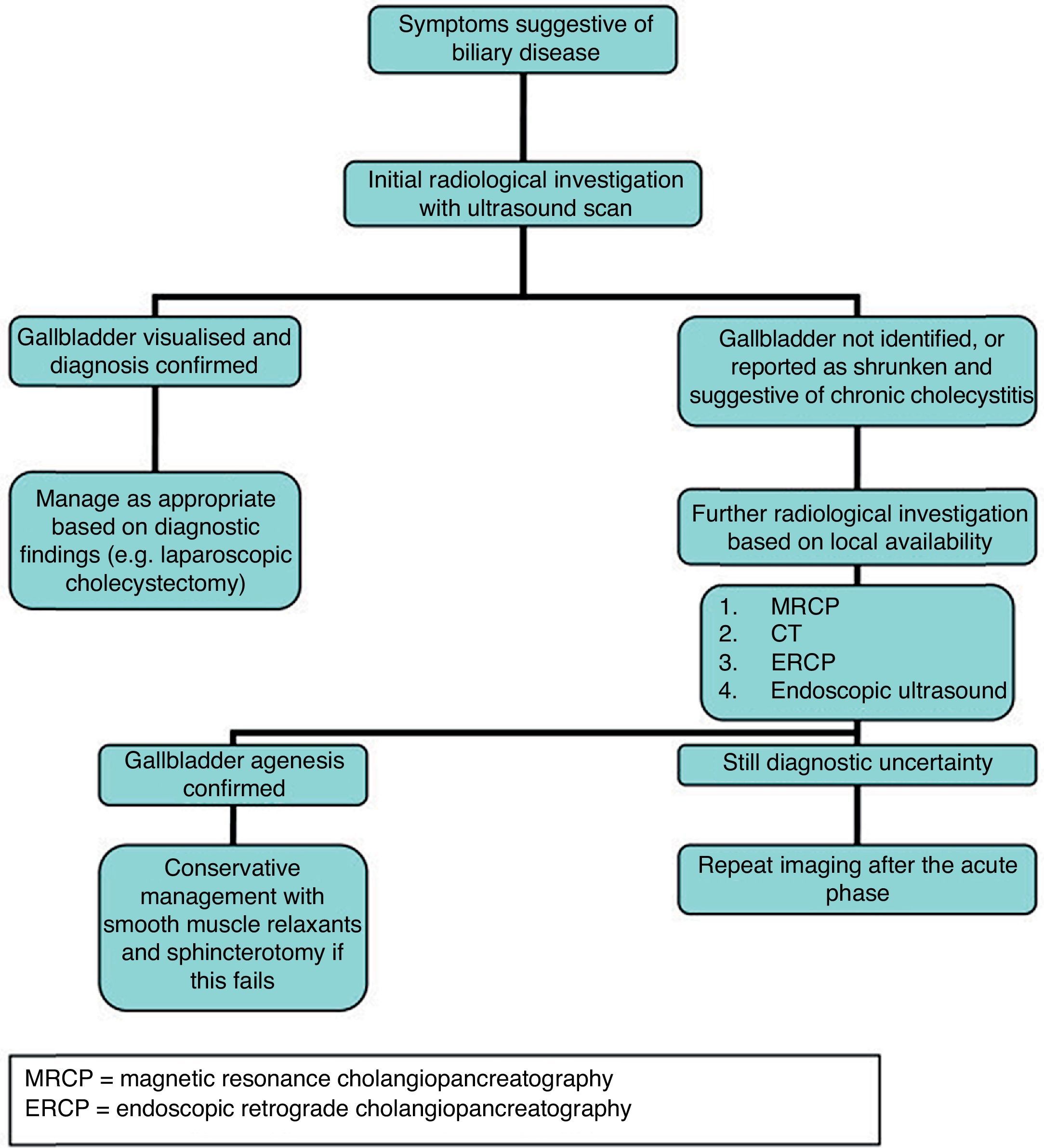
A lack of awareness of this condition among surgical, gastroenterologic, and radiologic staff was the main reason for operative intervention in this case, and the subsequent conversion to an open procedure. Despite a suggestive ultrasound, the diagnosis was still not made, and the patient underwent cholecystectomy for presumed gallstones. This highlights the need for greater appreciation of agenesis of the gallbladder as a cause of biliary symptoms, especially when initial radiologic tests suggest an absent gallbladder. A suggested decisional tree for the investigation of suspected gallbladder agenesis has been devised (Fig. 2) in an attempt to identify this rare condition pre-operatively, thereby preventing the unnecessary operative intervention seen in this case.10
ConclusionIn conclusion, agenesis of the gallbladder is a rare but well-recognized congenital abnormality, and it is a significant diagnostic challenge, with minimum rate of pre-operatory diagnosis. However, clinical and radiologic features mimic those of more common biliary conditions, and so patients frequently undergo unnecessary operative procedures. With the newer minimally invasive radiologic techniques, this situation can largely be avoided if awareness of this condition is improved. Pre-operative MRCP should be considered in cases in which ultrasound suggests non-visualization of the gallbladder, and surgeons should maintain a low threshold for further investigation before any decision to operate. Radiologists and clinicians should keep this entity in mind whenever the gallbladder is improperly visualized in routine imaging methods, in patients with or without biliary-type pain and also in patients with other known abnormalities/agenesis (genitourinary, gastrointestinal, cardiovascular, and others). Surgeons must be conservative in surgical procedures when agenesis of the gallbladder is diagnosed.