Hepatocellular carcinoma (HCC) is the most common primary liver malignancy and the third cause of death related to cancer. Through the application of surveillance programs the percentage of early diagnosis has increased but the diagnosis is still made at advanced stages in some patients. The presentation of HCC as progressive jaundice secondary to bile duct tumor thrombi is uncommon. In such cases it is extremely difficult to distinguish such biliary lesions from cholangiocarcinoma or even common bile stones. We report a case of a 34-year-old male patient with common bile duct invasion secondary to HCC that mimicked choledocholithiasis. The diagnosis of HCC was confirmed after thrombi extraction during ERCP.
El hepatocarcinoma (HC) es el tumor maligno primario hepático más frecuente y la tercera causa de muerte relacionada con el cáncer. Gracias a los programas de vigilancia, el porcentaje de diagnósticos precoces ha aumentado, pero en algunos pacientes aún se diagnostica en las etapas avanzadas. La presentación de un hepatocarcinoma como una ictericia progresiva secundaria a trombos tumorales en el conducto biliar es poco frecuente. En tales casos, resulta muy difícil distinguir dichas lesiones de un colangiocarcinoma o incluso de los cálculos biliares comunes. Se presenta el caso de un varón de 34 años con invasión de la vía biliar, secundaria a un hepatocarcinoma con apariencia de coledocolitiasis. El diagnóstico de hepatocarcinoma se confirmó tras la extracción de trombos durante una colangiopancreatografía retrógrada endoscópica (CPRE).
Hepatocellular carcinoma (HCC) is the most common primary liver malignancy and the third cause of cancer related death.1 Through the application of surveillance programs the percentage of early diagnosis has increased, but in a high proportion of patients the diagnosis is still established at an advanced stage. Presentation of HCC as progressive jaundice secondary to bile duct tumor thrombi is uncommon.2 In patients with concomitant gallstones the differential diagnosis with cholangiocarcinoma or even common bile duct stones may be difficult to establish. We report a case of common bile duct invasion (thrombi) secondary to HCC that mimicked choledocholithiasis.
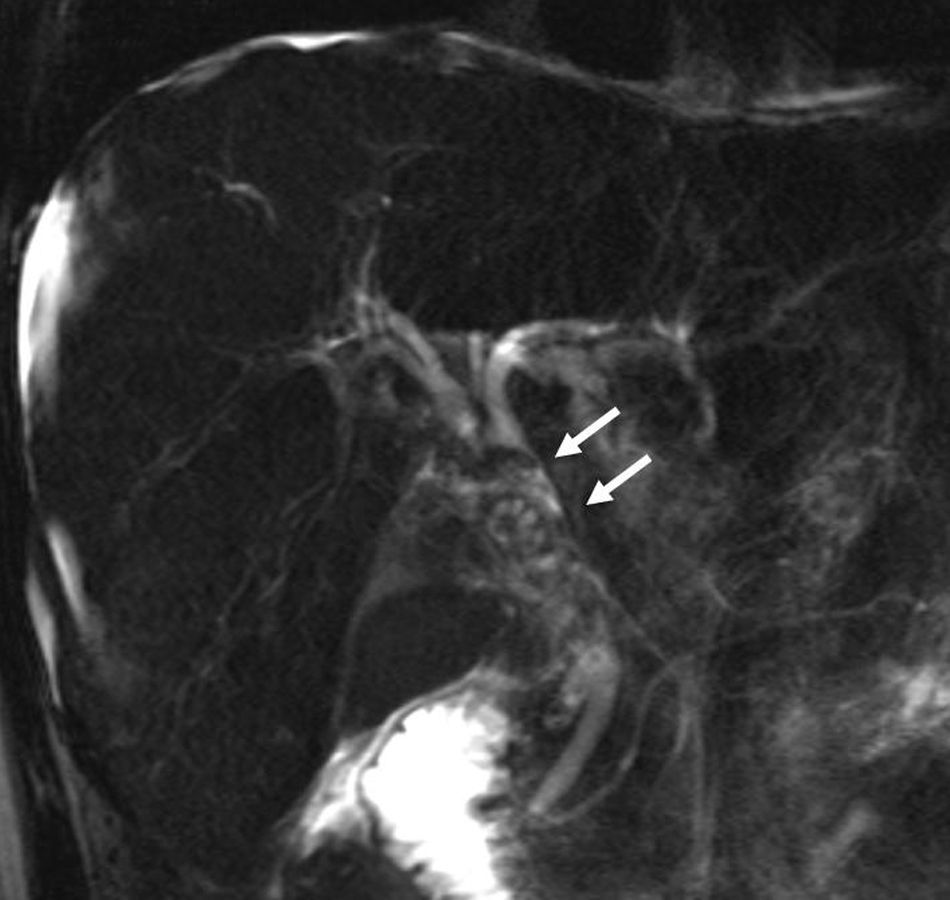
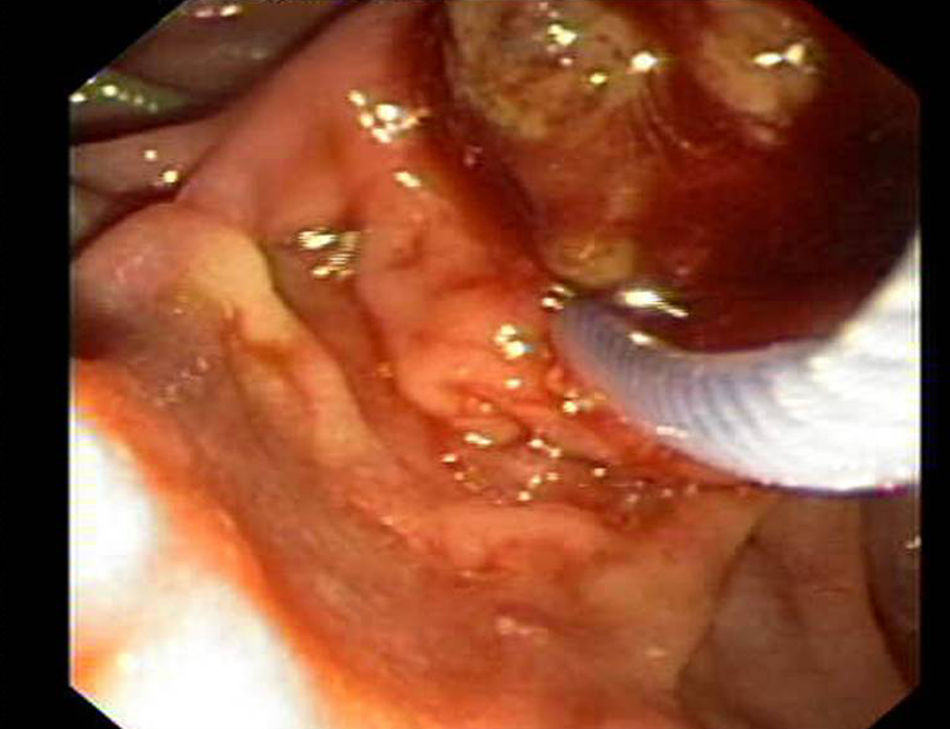
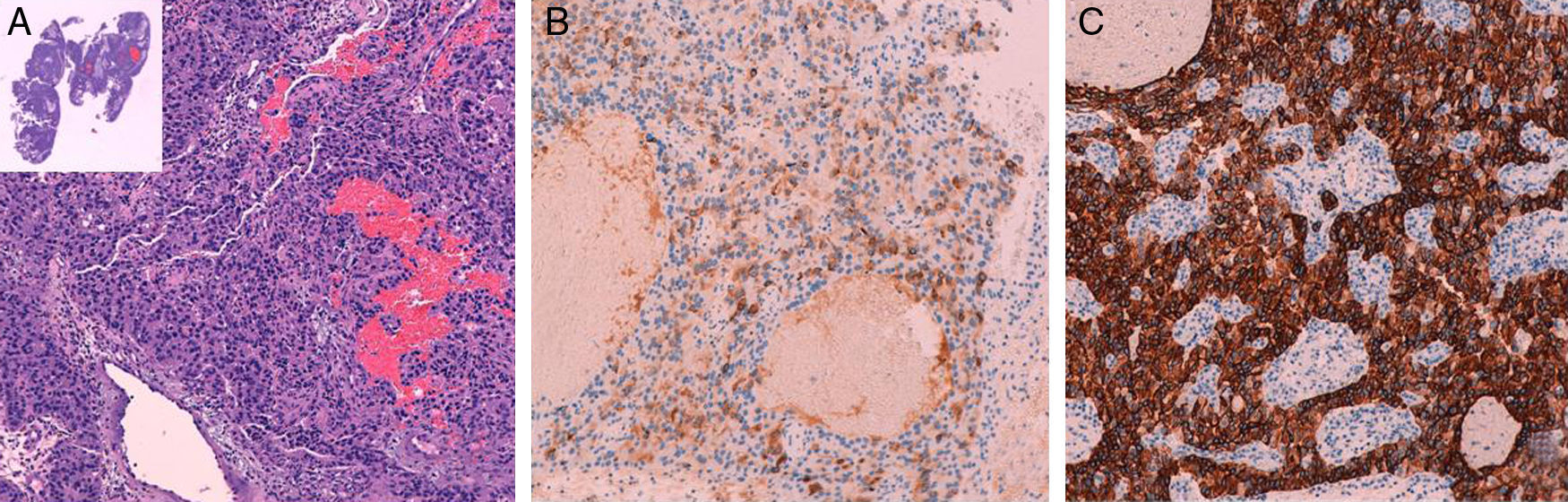
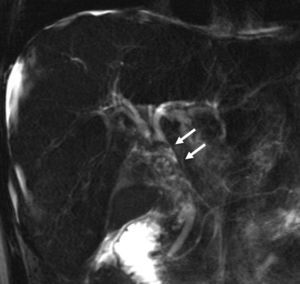
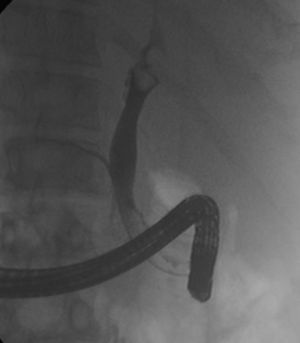
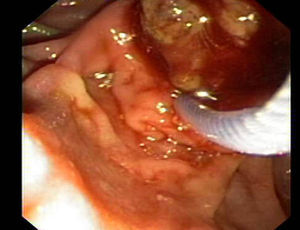
Clinical observationA 34-year-old male patient with history of untreated hepatitis B virus (HBV) infection was admitted for recurrent colicky right upper quadrant abdominal pain and jaundice. On exam, the patient was in mild distress, he had jaundice and there was mild tenderness in his right upper quadrant without rebound tenderness. The laboratory test showed a serum bilirubin 7mg/dL, alkaline phosphatase 573IU/L, gamma-glutamyl transpeptidase 226IU/L, INR 1.49, albumin 28g/L and high levels of alpha fetoprotein (10,861ng/ml). An abdominal ultrasound showed an enlarged liver and a heterogeneous area in the right hepatic lobe. Cholelithiasis with bile duct dilatation (14mm) was also observed. Magnetic resonance cholangiopancreatography showed multiple nodules, predominantly in the right hepatic lobe, with contrast enhancement in the arterial phase and venous washout compatible with HCC. It also showed gallstones and a dilated common bile duct with multiple filling defects (Fig. 1). Choledocholithiasis was suspected and endoscopic retrograde cholangiopancreatography (ERCP) was performed. The cholangiogram showed extrahepatic bile duct dilation with multiple nodular filling defects in the common bile duct (Fig. 2). Endoscopic biliary sphincterotomy was performed, and three 1-cm dark greenish and friable lesions were extracted using a Dormia-type basket (Fig. 3). The lesions were thrombi and a confirmation of HCC was obtained with the histopathological examination of the lesions (Fig. 4). The patient had a progressive improvement of the liver tests until complete normalization of the bilirubin levels. Sorafenib therapy was started after normalization of liver function but was interrupted four months later because of progressive deterioration of the general status, ascites, and worsening liver tests. CT-scan showed progressive disease with an increase in the size of liver nodules, vascular thrombosis and appearance of lung metastases. The patient died five months after the diagnosis secondary to variceal bleeding.
Obstructive jaundice secondary to biliary HCC thrombi is a rare presentation of HCC in non-previous cirrhotic patients with an incidence of 0.5–13%.2 Patients with HCC can develop obstructive jaundice secondary to bile duct compression by the tumor or even by lymph node metastasis, but direct bile duct invasion (thrombi) is a less frequent cause. Compared to patients without biliary HCC thrombi, those with biliary HCC thrombi present with advanced stages as determined by a significantly higher rate of pTNM stages III and IV, more frequent macroscopic vascular invasion, and are poorly differentiated tumors.3,4 However, there are some reports where biliary HCC thrombus was diagnosed in patients without obvious intrahepatic tumor.5,6 The great majority of the cases with bile duct HCC thrombi have been described in Asian patients with HBV infection.2
HCC may be derived from different levels of hepatocellular lineage. A recent study that evaluated liver stem cell markers suggests that biliary HCC thrombi may derive from the putative liver stem cells in the terminal bile duct.3 These findings may explain that small HCC could develop biliary invasion without macroscopic or microscopic bile duct infiltration.3 As we mention in the present case, biliary HCC thrombi may be difficult to differentiate from choledocolithiasis when there is evidence cholelithiasis and bile duct dilation. Although imaging methods are sensitive in detecting different causes of biliary tract obstruction, ERCP remains the gold standard diagnostic procedure for imaging the extrahepatic biliary tract. Extraction of bile duct thrombi using a basket may be difficult because friability and fragmentation of the thrombi.7 Furthermore, thrombi tend to be mobile increasing the difficulty of basket capture. In this situation the use of guide-wire and extraction with balloon may be necessary.7 Lesions can be either small or larger. Small lesions are localized in one or two ducts. However, large lesions as the present case can form “biliary duct cast” with distal extension. As is shown in Fig. 2 bile duct dilation with a fusiform shape is present at the site of lesion.2
Histological evaluation is critical when bile duct lesions are found in patients with liver cancer. Differential diagnosis with other causes of bile duct obstruction that may be present in these patients are blood clots (hemobilia secondary to the tumor) or cholangiocarcinoma.2 In both situations anemia may be present as well as other signs of gastrointestinal bleeding.
The presence of common bile duct thrombi in patients with HCC is usually associated with an advanced stage of the disease and for this reason it has a poor short-term prognosis, although the independent value of this finding is unclear. In patients with advanced HCC sorafenib is the first-line treatment.8 There is little information on the operative results of hepatectomy in patients with HCC with biliary HCC thrombi, probably because of the low incidence of this presentation.4 However, a poor operative outcome was shown in recent retrospective series.3,4
In conclusion HCC presenting as bile duct thrombi is rare but can be easily diagnosed with ERCP and thrombi extraction, this not only confirms of the diagnosis by obtaining tissue but also establishes biliary drainage and relief of cholestasis and jaundice in order to consider oral therapy with sorafenib in advanced stages.
Conflict of interest statementThe authors declare no conflict of interest.
The authors thank Carlos Rodriguez de Lope for the critical review of this article.