Hepatitis E virus (HEV) is one of the most common causes of enteric hepatitis worldwide.1 It often presents asymptomatically or with symptoms of acute hepatitis that resolve spontaneously. Chronic hepatitis has been described in immunocompromised patients, and could explain some cases of idiopathic chronic liver disease. The most effective treatment remains unknown. We present a case of chronic hepatitis E in a 61-year-old immunosuppressed woman that responded to ribavirin treatment.
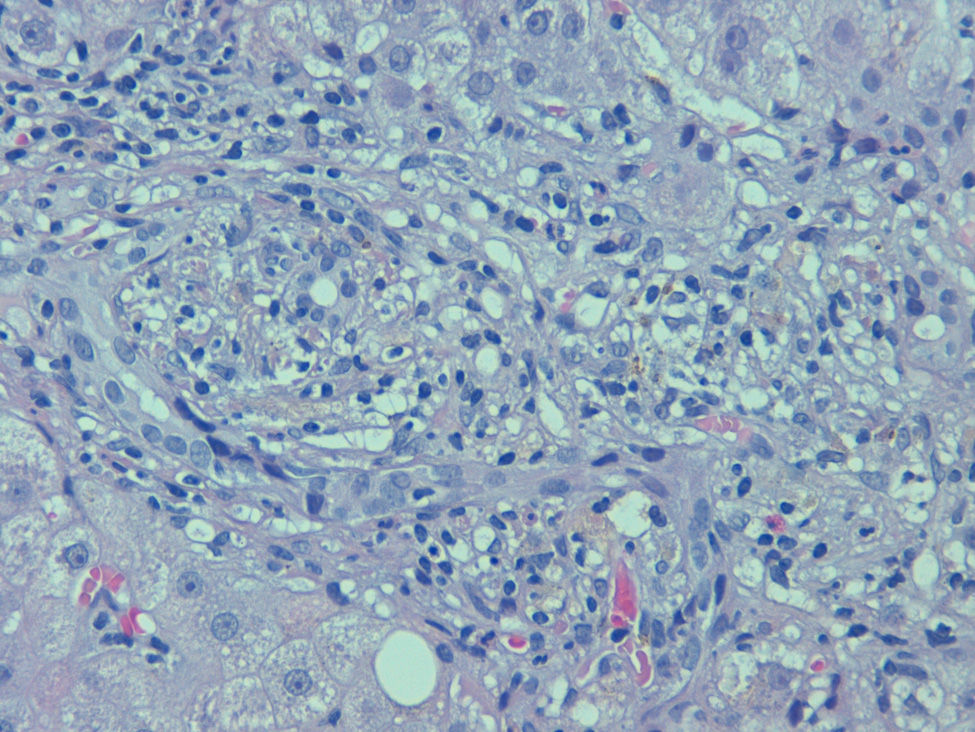
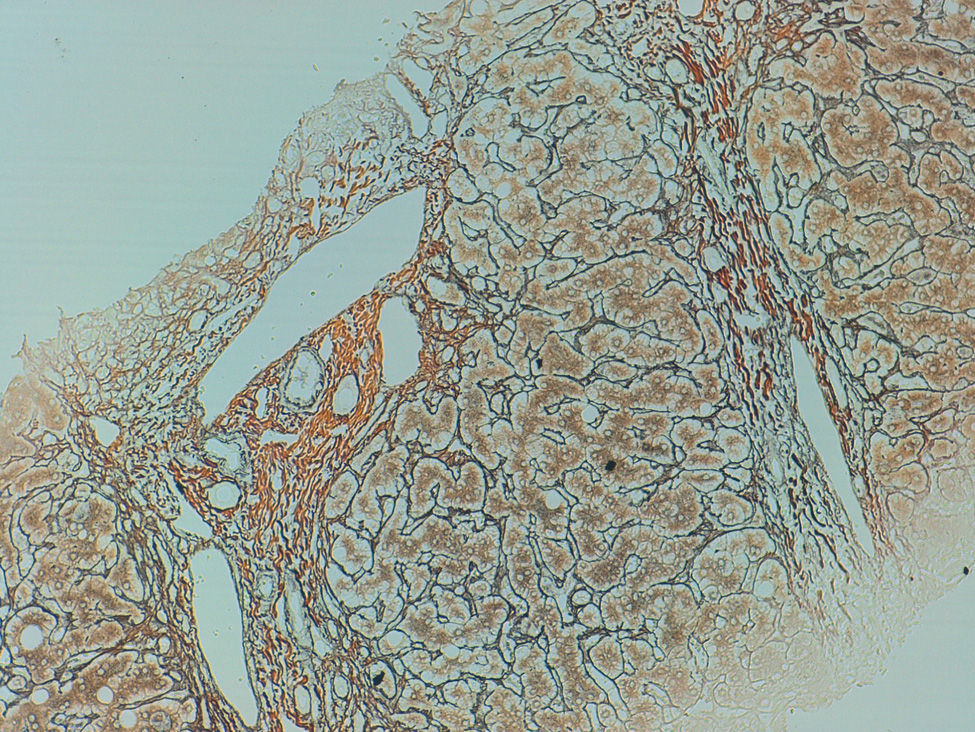
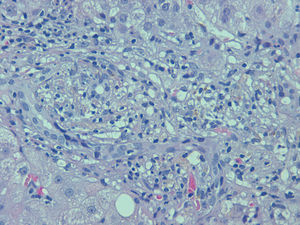
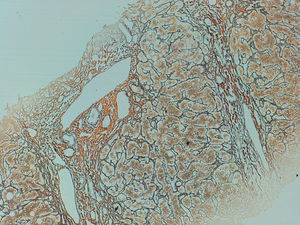
The patient had been diagnosed with non-Hodgkin lymphoma, and was in partial remission following several immunosuppressive treatments (cyclophosphamide, doxorubicin, vincristin and prednisone [CHOP]; fludarabine, mitoxantrone, cyclophosphamide [FMC]); autologous haematopoietic stem cell transplant; galixumab and rituximab. In the previous year she had occasionally presented abnormal liver enzymes, with serology negative for hepatitis A (HAV), hepatitis B (HBV), hepatitis C (HCV) and human immunodeficiency virus (HIV); autoimmunity tests were negative and she had hypogammaglobulinaemia (IgM 9.05mg/dL, IgA 6.13mg/dL and IgG 277mg/dL). Abdominal ultrasound showed a normal-sized liver with findings of diffuse liver disease but no signs of portal hypertension. Percutaneous liver biopsy (Figs. 1 and 2) found duct destruction and disruption of the limiting plate in portal spaces due to periportal necrosis (grade 2) and fibrosis (grade 2). Macrovesicular steatosis (30–40%), necrosis (grade 2), cytoplasmic tumefaction and central and periportal collagenization were also observed, consistent with chronic hepatitis with signs of activity (Ishak fibrosis score of 8).2 Six months after start of follow-up—and despite no findings of advanced liver disease—she presented her first episode of oedematous-ascitic decompensation. Ascitic fluid with a serofibrinous appearance was obtained, with total protein 1.15g/dL, albumin gradient >1.1g/dL, 300 polymorphonuclear cells/μl, and culture positive for Hafnia alvei, which responded to antibiotic treatment with cefuroxime. HEV-RNA testing performed at this stage was positive in blood and stool, with no antibodies.
The patient was diagnosed with chronic hepatitis E and started treatment with ribavirin (RBV) at a dose of 400mg/12h. After 4 weeks treatment, liver biochemistry tests returned to normal and HEV-RNA testing was negative. Liver transaminases remained normal and HEV-RNA testing was negative at the 12, 24 and 48-week follow-ups. Treatment was discontinued after 48 weeks. The patient currently presents findings of chronic liver disease with portal hypertension and small oesophageal varices, but has not required readmission and has maintained a sustained viral response.
Until recently, HEV was believed to cause acute and fulminating hepatitis in selected cases only, with no likelihood of becoming chronic. The prevalence of anti-HEV antibodies in the Spanish general population is estimated to be 2.2%-7.3%. Progression to chronic liver disease has been hitherto unheard of, but recent studies and reported cases suggest otherwise, as happened in our patient.1,3,4 Most patients are immunosuppressed,4 but exceptionally it can affect immunocompetent individuals.5 HEV could explain some of the cases considered as chronic liver disease/cryptogenic cirrhosis,6 although there is insufficient scientific evidence to recommend serology in cases of unknown aetiology.7
In our patient, in whom immunosuppressive treatment could not be adjusted due to the high risk of relapse of the underlying disease, ribavirin treatment was proposed based on published studies.
A study by Kamar et al.8 showed that only 32% of infected patients presented symptoms, and 60% evolved to chronic hepatitis. The main predictors of evolution were immunosuppression with tacrolimus and low platelet count at diagnosis.1,8 Viral clearance was observed in 30% of patients when the immunosuppressive dose was reduced.8
There are no established recommendations regarding the most appropriate treatment for chronic hepatitis E.6 Additionally, few patient reports have been published—which moreover have been very heterogeneous—thus preventing definitive conclusions from being drawn.
Progression to chronic hepatitis is more common the higher the dose of immunosuppressive treatment.6 For this reason, dose reduction of immunosuppressive therapy is recommended as a first therapeutic step, when possible.8,9
The most widely recommended treatment options are pegylated interferon alpha-2a or 2b (Peg-IFN) and ribavirin as mono- or combination therapy,9,10 although neither the optimal dose nor the duration have been clarified. No statistically significant differences are observed when both treatments are compared. Peg-IFN alpha increases the risk of rejection in kidney and heart transplant patients, and should be used with caution in these cases.1 Several studies support the use of ribavirin in chronic hepatitis in solid organ recipients4 and haematologic malignancies, but relapses have been described following discontinuation of treatment.4,9
Mallet et al.10 and Kamar et al.4 presented a series of solid-organ transplant recipients with chronic HEV infection. Patients were treated with ribavirin as monotherapy (12mg/kg/day or 600mg/day for a mean of 3 months) without reducing the immunosuppressive dose. Viral clearance was observed in 95% of the patients and a sustained virologic response in 78%.4 Although the data are limited, these studies show that ribavirin as monotherapy may be useful in chronic HEV infection as a first therapeutic option in patients who are not candidates for immunosuppressive dose reduction. Three months appears to be the appropriate time for maintaining treatment and assessing the virologic responses. In our patient, this therapeutic approach achieved a good outcome. The presence of HEV should be evaluated in patients with chronic liver disease of unknown aetiology, especially in immunosuppressed subjects, although further studies are required before this can be recommended systematically.
Please cite this article as: Mora Soler AM, Velasco-Guardado A, Martín Arribas MI, Acosta Materan R, Revilla Morato C, Pérez Corte D, et al. Hepatitis crónica por virus de la hepatitis E tratada con ribavirina. Gastroenterol Hepatol. 2016;39:597–598.