Since ancient times the increase of size and hardness sometimes presented by the abdominal structure known as the pancreas has attracted attention. Portal was the first to describe the clinical signs of chronic pancreatitis in 1803. In 1815, Fleischman speculated about the potential role of excessive alcohol consumption. Comfort coined the term “chronic relapsing pancreatitis” in 1946 and described hereditary pancreatitis 6 years later. Zuidema defined tropical pancreatitis in 1959 and 2 years later Sarles described another form of pancreatitis to which Yoshida gave the name autoimmune pancreatitis in 1995. Groove pancreatitis was described by Potet in 1970. Obstructive pancreatitis was defined in 1984 and Ammann identified idiopathic pancreatitis 3 years later. This article gives a historical account of the pioneers who developed the knowledge of how to assess the characteristics that allowed the different forms of chronic pancreatitis to be defined.
Desde la antigüedad había llamado la atención el aumento de tamaño y dureza que, en ocasiones, presentaba la estructura abdominal que recibió el nombre de páncreas. Portal en 1803 describió por primera vez los signos clínicos de la pancreatitis crónica. En 1815 Fleischman especuló sobre el posible papel del consumo exagerado de alcohol. Comfort en 1946 acuñó el término «pancreatitis crónica recidivante» y 6 años más tarde refirió lo que se llamaría pancreatitis hereditaria. Zuidema en 1959 definió la pancreatitis tropical y 2 años después Sarles puntualizó sobre otra forma de pancreatitis que en 1995 Yoshida denominaría pancreatitis autoinmune. La pancreatitis del surco era descrita en 1970 por Potet. En 1984 se definió la pancreatitis obstructiva y en 1987 Ammann refirió la pancreatitis idiopática. En este artículo se hace un recuerdo histórico de los pioneros que supieron valorar determinadas características que permitieron definir diferentes formas de pancreatitis crónicas.
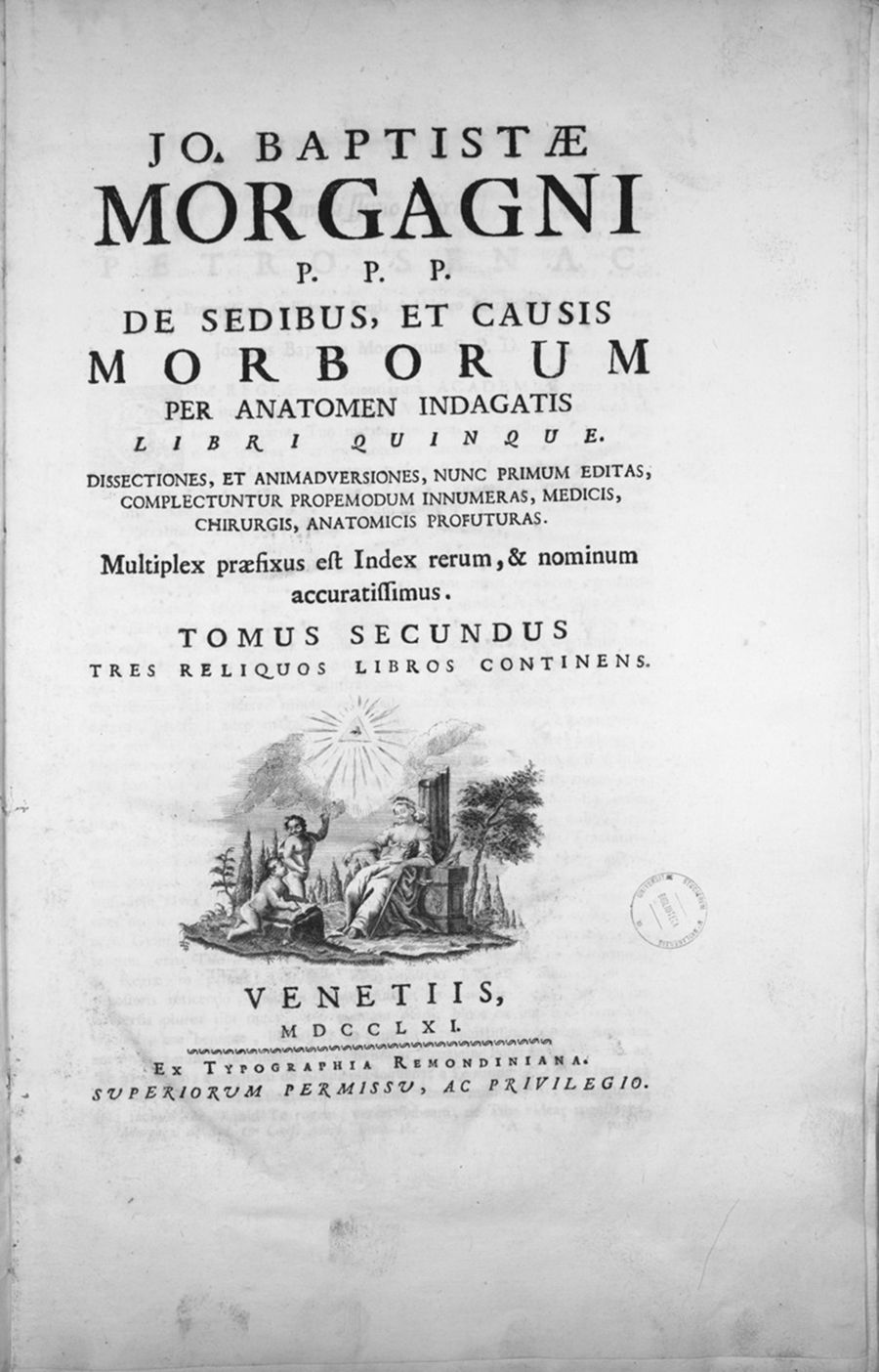
Back in Ancient Greece, some scholars had observed that in certain cases the pancreas – given its name at the end of the 1st century by Rufus of Ephesus – had a hardened consistency or tumour-like appearance, and thus described it with the word skirros. However, they made no reference to any specific disease, since they were also unaware of the role played by the organ. It was not until 1679 that pathologist Théophile Bonet (Geneva, Switzerland, 1620–1689) observed pancreatic calculi while performing a post-mortem on a jaundiced patient. This finding was described in his book Sepulchretum sive Anatomica Practica ex Cadaveribus Morbo denatis (“Cemetery or Anatomical Studies on Bodies Affected by Disease”), containing almost 3000 post-mortems and their respective medical histories. In the years thereafter, anatomists Prieto Nanni (Bologna) in 1731 and Johann Friedrich Meckel (Wetzlar, Germany, 1724–1774), the first of a line of four physicians and embryologists, in 1764, also described the presence of pancreatic calculi in several post-mortems.1 Giovanni Battista Morgagni (Forli, Italy, 1682–1771), a student of Valsalva and Albertini, detailed in his book, published in Padua in 1761, entitled De sedibus et causis morborum per anatomen indagatis (“On the Seats and Causes of Diseases as Investigated by Anatomy”), more than 700 medical histories with their respective post-mortems, the existence of pancreatic calcifications in some of his dissections2 (Fig. 1).
Later, in 1788, English surgeon and physiologist Thomas Cawley published his post-mortem findings on a 34-year-old diabetic patient whose pancreas was full of calculi.3 Cawley was not able to establish whether the pancreatic lesion observed had led to the onset of diabetes or, put differently, if long-term chronic pancreatitis had caused the patient to develop diabetes as a complication. In 1793, Matthew Baillie (1761–1823), a Scottish physician and pathologist, and nephew of the anatomist John Hunter, published the book The morbid anatomy of some of the most important parts of the human body (considered the first systematised pathology study), in which he described a hard pancreas with distinct lobules and concretions in the ducts and areas of fibrosis.4
In 1803, Antoine Portal (Gaillac, 1742-Paris, France, 1832), who was doctor to Louis XVIII and Charles X, founding president of the Académie Nationale de Médecine in France and the first person to describe gastrointestinal bleeding due to oesophageal varices, reported the clinical signs of chronic pancreatitis. His description was corroborated in 1814 by the doctor to the Prince of Wales, Christopher Robert Pemberton (Cambridgeshire, 1765-Fredville, United Kingdom, 1822).5
One year later, G. Fleischmann described in his work Leichennöffnurgen (“Post-mortems”) the case of a young male with a history of alcoholism who had died after repeated episodes of abdominal pain, nausea and vomiting. During the post-mortem, he observed an incredibly hard pancreas and hypothesised that this might constitute the “chronification” of pancreatitis.6 This may have been the first time alcohol was linked to a chronic pancreatic lesion.
Based on this description, Heinrich Claessen in 1842 and Nikolaus Friedreich (Würgburg, 1825-Heidelberg, Germany, 1882), in 1878, speculated that alcohol plays a role in the development of pancreatic inflammation.7,8 In 1899, Étienne Lancerenaux (Brécy-Brières, France, 1829–1910) finally confirmed the relationship between the pancreas and diabetes, coining the term “pancreatic diabetes”.9
The first imaging diagnosis of pancreatic disease was performed in 1927 when calcifications in the pancreatic area were observed on a plain abdominal X-ray. This was possible thanks to the discovery made by Wilhelm Conrad Röntgen (Lennep, Prussia [now Germany], 1845-Munich, Germany, 1923) in 1895, which earned him the Nobel Prize in Physics in 1901.10
In 1946, Mandred W. Comfort (Hillsboro, Texas, USA, 1894–1957), a doctor at the Mayo Clinic in Rochester, Minnesota, established a new clinical and anatomopathological concept on introducing the term “chronic relapsing pancreatitis”.11 Years later, Joseph L. Owens and John M. Howard, surgeons at the Grady Memorial Hospital in Atlanta, made a clear distinction between lithiasic and alcoholic pancreatitis.12 But it was not until 1963, at a meeting held in Marseilles under the watchful eye of the chair Henri Sarles (Ermont, 1922-Marseilles, France, 2017), a renowned gastroenterologist at the Hôpital Sainte Marguerite in Marseilles, where a consensus was reached on the first pancreatitis classification, based primarily on clinical and morphological criteria. This classification distinguishes between acute, acute relapsing, chronic and chronic relapsing pancreatitis.13 In March 1983, a new classification was proposed in the city of Cambridge, under the auspices of the Pancreatic Society of Great Britain and Ireland.14 A year later, a second symposium was held, again in the city of Marseilles. The distinction between acute and chronic pancreatitis was maintained at both meetings.15 Chronic pancreatitis was defined as a disease characterised by irreversible histological changes that can be progressive and lead to a loss of exocrine and endocrine functions, and which are very often associated with abdominal pain. At the last symposium, a special form was defined, chronic obstructive pancreatitis, which is characterised by possible improvement in exocrine function once decompression of the obstructed pancreatic duct has been achieved (see below).
Throughout history, different types of chronic pancreatitis have been described, presenting unique characteristics which allow differentiation between chronic alcoholic pancreatitis, hereditary pancreatitis, tropical pancreatitis, groove pancreatitis, obstructive pancreatitis, idiopathic pancreatitis and a special type known as autoimmune pancreatitis. This article remembers the prominent figures who were able to assess specific clinical, morphological and aetiological characteristics, allowing them to differentiate between these different types of chronic pancreatitis. The characteristics of each are described herein, according to the chronological order in which they appear in the medical literature.
Chronic alcoholic pancreatitisFollowing G. Fleischman's observation in 1815, where he linked morphological pancreatic changes compatible with chronic pancreatitis to his post-mortem patient's history of alcoholism,6 other authors like P.J. Bécourt in 1830,16 Heinrich Claessen in 1842 and Nikolaus Friedreich (who described the ataxic syndrome which bears his name in 1863) in 1878 theorised about the effect of alcohol on the development of pancreatic inflammation.7,8 These authors were the first to highlight what would later be considered one of the main causes of pancreatitis. Nikolaus Friedreich coined the term “drunkard's pancreas”, a term subsequently popularised by Reginald Fitz (Chelsea, Massachusetts, USA, 1843–1913) in 1889, when he documented the signs and symptoms of acute pancreatitis and established the different phases of the process in his article for the Boston Medical and Surgical Journal,17 a journal published from 1828 to 1928 which went on to become the New England Journal of Medicine.
In 1946, as well as adopting the novel term “chronic relapsing pancreatitis”, establishing clinical and anatomopathological concepts, Mandred W. Comfort outlined the link between chronic pancreatitis and alcohol abuse.11 Later, as described previously, in 1958 Joseph L. Owens and John Howard made a distinction between lithiasic and alcoholic pancreatitis, observing that calcifications were much more common in cases of chronic pancreatitis with a history of excessive alcohol consumption.12
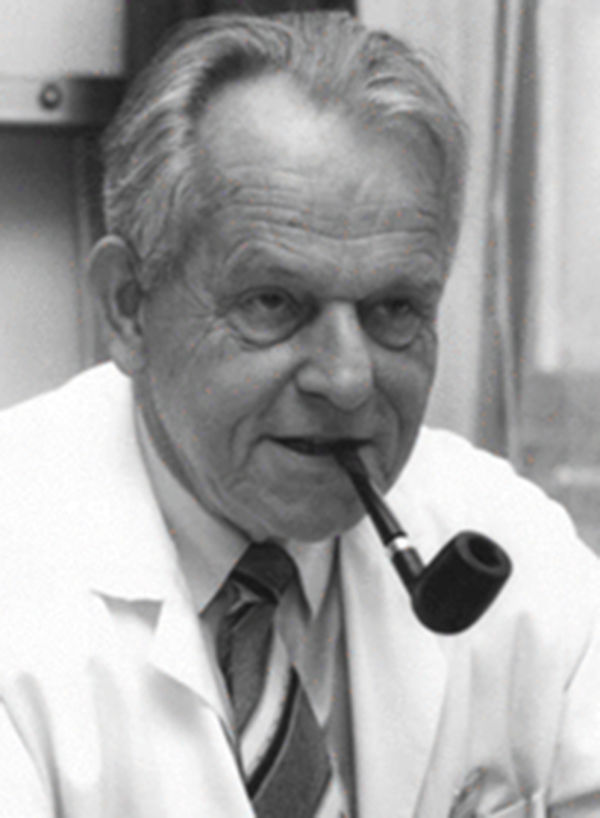
In 1975, Henri Sarles (one of the pioneers of European Pancreatology) published an article where, based on his experiments on dogs and observations in humans, he proposed a series of concepts linking alcohol consumption to chronic pancreatitis (Fig. 2). Sarles observed this occurrence in individuals with an average alcohol consumption of 150ml/day over a period of no less than two years, although it was more common for this time period to range between 6 and 10 years. The disease was seen in the third and fourth decades of the individual's life. He also believed that chronic calcifying pancreatitis developed from the precipitation of proteins secreted by the pancreas, forming plugs which are deposited in the ducts and acini and that later collect calcium, leading to pancreatic calculi. These plugs irritate the duct epithelium which atrophies and then disappears. Periductal connective tissue proliferation appears in its place, along with the obstruction of the ducts, thereby favouring the formation of cysts.18
Nevertheless, years later it was observed that only a proportion of alcoholics develop symptomatic chronic pancreatitis. This has led to the assumption that alcohol is a cofactor that affects susceptible subjects, and that other environmental and/or genetic factors must therefore be involved for the disease to develop. Among the environmental factors, toxic elements have been highlighted, particularly smoking, which was recently shown to be an independent and dose-dependent risk factor for the development of chronic pancreatitis and to accelerate the progression of chronic alcoholic pancreatitis.19,20
It has also been noted that some genetic factors result in a predisposition to the disease. Thus, in 2000, German physician Heiko Witt (1966) and his team described the first mutation (p.N34S) of the PSTI (Pancreatic Secretory Trypsin Inhibitor or SPINK1) gene in children with chronic pancreatitis, which was also later identified in other forms of chronic pancreatitis, as detailed below.21 SPINK1 is a powerful protease inhibitor that deactivates prematurely activated trypsin inside the acinar cell, acting as a defence mechanism.
In relation to chronic alcoholic pancreatitis, Witt and other researchers agree that only 5–6% of patients have some form of SPINK1 mutation and it is not considered to be a determining gene in this type of pancreatitis, despite the fact that the percentage cited is clearly higher than in the control population.22,23 Although uncommon, mutations of the PRSS1 gene (cationic trypsinogen gene) have also been observed in this form of pancreatitis.
Chronic hereditary pancreatitisThe aforementioned Mandred W. Comfort of the Mayo Clinic (Rochester), who was named President of the American Gastroenterological Association in 1957, the year of his death, described in 1952 a family in which four members were suffering from chronic pancreatitis, with another two suspected of having it, leading him to contemplate the hereditary origin of the disease24 (Fig. 3).
Chronic hereditary pancreatitis is a disease transmitted in an autosomal dominant pattern which represents 2–3% of chronic pancreatitis cases. The diagnosis thereof requires the existence of recurrent pancreatitis outbreaks in at least two first-degree relatives, or three or more second-degree relatives, across two or more generations, with no evidence of other precipitating factors. The disease generally manifests before 20 years of age, with no gender predominance. If these criteria are not met, but more than one relative has chronic pancreatitis, with no dominant inheritance pattern, the disease is classified as familial pancreatitis. In this case, mutations of the SPINK1 gene have been observed (60–80% of patients).23
In 1996, a team from the University of Pittsburgh led by David C. Whitcomb was able to link hereditary pancreatitis to a p.R122H mutation of the cationic trypsinogen gene (PRSS1).25 This mutation was identified in all of the members of five families with hereditary pancreatitis, but in none of the 141 control subjects. Since then, over 20 mutations have been identified in this gene. In addition to the aforementioned p.R122H mutation, notable mutations include p.N29I and p.A16V, which are present in 80% of hereditary pancreatitis cases.26 The cationic trypsinogen gene plays a fundamental role in activating the remaining pancreatic proenzymes and its premature activation thus leads to autodigestion and pancreatitis. Recurrent pancreatitis outbreaks lead to the development of chronic pancreatitis. During the evolution of this condition, endocrine and exocrine insufficiency occur, along with an increased risk of developing pancreatic cancer. According to a study by the International Hereditary Pancreatitis Study Group, said risk is 50 times higher than in the general population.27 Moreover, according to the European Registry of Hereditary Pancreatitis and Pancreatic Cancer, there is an even greater risk of these patients developing pancreatic cancer after 50 years of age, regardless of genotype.28 For this reason, in 2003 experts at the IV International Symposium of Inherited Diseases of the Pancreas recommended that such patients be subjected to a pancreatic cancer screening programme.29
Chronic tropical pancreatitisIn 1959, P.J. Zuidema (1908–1996), a Dutch physician and tropical diseases specialist, described what is known as chronic tropical pancreatitis. Having worked at Bethesda Hospital (Yogyakarta, Island of Java, Indonesia) for 20 years (1938–1958), Zuidema reported 45 cases of young patients presenting pancreatic calcifications and diabetes30; 22 years prior, in 1937, Mangalore Gopal Kini (Mangalore, Karnataka, India, 1893–1952), a prominent orthopaedic surgeon, had described the first case of pancreatic calculi observed in India.31 This publication was followed by others detailing the existence of pancreatic calculi observed post-mortem in individuals from the Vellore district in the south of the country.32 After Zuidema's publication, P.J. Geevarghese, a pioneer in the field, documented one of the largest series of tropical pancreatitis in the state of Kerala, in the far southwest of India.33 Later, studies were also published in various other countries, including Bangladesh, Sri Lanka, Nigeria and Uganda, etc., the populations of which share common nutritional deficiencies. More recently, a high prevalence of the disease was discovered in the Kerala region (1/793 inhabitants).34 Chronic tropical pancreatitis is characterised by symptoms of abdominal pain, steatorrhoea, diabetes and pancreatic calculi. It affects populations with a low socioeconomic status in tropical and subtropical countries who have diets low in protein and fat. Found to be responsible was a diet rich in cassava, a tuber containing toxic cyanogens such as linamarin and lotaustralin, which are converted into prussic acid (hydrogen cyanide) by the linamarase enzyme, also present in the tuber. However, recent epidemiological and experimental studies have questioned this hypothesis35 (Fig. 4).
In 2002, two studies were published which noted that almost half of tropical pancreatitis patients presented a N34S mutation of the SPINK1 gene, suggesting the potential existence of a genetic predisposition to developing the disease.36,37
Autoimmune pancreatitisAutoimmune pancreatitis was first described by Henri Sarles (Hôpital Sainte-Marguerite, Marseilles) in 1961, when he observed a case of pancreatitis associated with hypogammaglobulinaemia, calling it primary inflammatory pancreatitis.38 The condition was later given the names chronic inflammatory pancreatitis (Marseilles-Rome Meeting, 1988),39 lymphoplasmacytic sclerosing pancreatitis,40 non-alcoholic duct destructive chronic pancreatitis and inflammatory pseudotumour of the pancreas, among others. Finally, in 1995, Kiyotsugu Yoshida of the University of Jikei (Tokyo) proposed the term “chronic autoimmune pancreatitis”, the name by which it is currently known.41
Yoshida believed the disease's defining characteristics to be elevated IgG levels, an increase in pancreas size with fibrosis and diffuse lymphocytic infiltration, an absence of calcifications and pseudocysts, and very few clinical manifestations like pain or pancreatitis outbreaks, but evident cholestasis. In many cases, pancreatic enlargement and cholestasis led to a differential diagnosis with pancreatic cancer, so sometimes diagnosis was only reached after an analysis of the surgical specimen, since the pancreas was excised in light of a neoplasm being suspected in the gland.
Since then, various expert groups have suggested modifications to the diagnostic criteria. Thus, in 2002 the Japan Pancreas Society proposed data obtained from imaging techniques (enlargement of the pancreas and duct narrowing with an irregular wall) as diagnostic criteria, along with laboratory findings (elevated antibodies or IgG4) and/or the histopathological examination of the pancreas (inter-lobular fibrosis and infiltration of lymphocytes and plasma cells).42 Later, in 2006, the South Korean group led by Kyu-Pyo Kim of the University of Ulsan (Seoul, South Korea) added response to steroid therapy to the previous criteria. In order to confirm the diagnosis, one of the three remaining criteria should accompany imaging findings.43 That same year, Suresh T. Chari and his team shared the Mayo Clinic Experience, increasing the diagnostic criteria to 5, having added other organ involvement (hilar/intrahepatic biliary strictures, parotid/lacrimal gland involvement, mediastinal lymphadenopathy and retroperitoneal fibrosis).44 In 2010, during the International Association of Pancreatology Congress held in Fukuoka (Japan), a panel of experts defined autoimmune pancreatitis as a distinct form of pancreatitis that frequently manifests as obstructive jaundice with or without a pancreatic mass that presents with characteristic histological changes consisting of lymphoplasmacytic infiltrate and fibrosis, with an excellent response to corticosteroid treatment.45 Two types of autoimmune pancreatitis are currently accepted, defined by a histopathological analysis of the pancreas: lymphoplasmacytic sclerosing pancreatitis and idiopathic duct-centric pancreatitis. However, given that histological data are not always available, the Honolulu consensus document, published in 2010, introduced the terms type 1 and type 2 autoimmune pancreatitis in order to describe the clinical manifestations associated with lymphoplasmacytic sclerosing pancreatitis and idiopathic duct-centric pancreatitis, respectively.46 Type 1 autoimmune pancreatitis is predominant in Asian countries (Japan and Korea). It is most prominent in males in the sixth decade of life, associated with elevated serum IgG4 levels and other organ involvement. A good response to corticosteroid therapy is one of its main characteristics, although recurrences are common. Type 2 pancreatitis, on the other hand, is more common in Europe and the USA. This form is more typical of individuals in the fifth decade of life, with no gender predominance, IgG4 elevation or other organ involvement, although it may be associated with ulcerative colitis and Crohn's disease. Response to corticosteroid therapy is good and relapses are uncommon.
The most accepted criteria at present are those resulting from the Fukuoka and Honolulu meetings, where the previously defined diagnostic criteria were unified by various societies (Japanese, Korean, Italian, Mayo Clinic and Mannheim).45
Groove pancreatitisGroove pancreatitis is a rare form of chronic pancreatitis, reported for the first time in 1970 by French pathologists François Potet and Nathalie Duclert, who described it as cystic dystrophy on aberrant pancreas tissue.47 The condition has also been given other names, such as paraduodenal pancreatitis, pancreatic hamartoma, myoadenomatosis and paraduodenal wall cyst.48 In 1973, another pathologist, V. Becker, gave it the German name Rinnepankreatitis (“channel pancreatitis”)49 and, in 1982, Mandred Stolte et al. coined the term Groove pancreatitis, the name it is known by today.50 In 1991, V. Becker and U. Mischke made a distinction between two different types of groove pancreatitis: the pure and segmental forms.51 In the former, the scar tissue only affects the pancreatic groove, leaving the duct of Wirsung and pancreatic parenchyma intact. In the segmental form, scar tissue extends to the cranial and dorsal portions of the pancreatic head adjacent to the duodenal wall and stenoses the pancreatic duct.
Groove pancreatitis is a very uncommon subtype of chronic pancreatitis of unknown origin, though it has been linked to increased alcohol and tobacco consumption, peptic ulcers and a heterotopic pancreas. It usually affects males in the fifth decade of life. It develops in the pancreaticoduodenal groove and also affects the duodenum and common bile duct. Due to its low incidence it has probably been underdiagnosed in the past. The condition manifests with abdominal pain, nausea, recurrent postprandial vomiting and weight loss. Jaundice is uncommon despite the fact it affects the bile duct. A differential diagnosis is made with other duodenal and pancreatic conditions, primarily pancreatic cancer. Endoscopic ultrasound and magnetic resonance cholangiopancreatography are the diagnostic techniques of choice. Microscopic analysis shows normal pancreatic tissue surrounded by large bands of intense fibrosis, Brunner's gland hyperplasia and hyalinised fibrosis of the duodenal submucosa. It is also common to find heterotopic pancreatic tissue in the submucosa and muscularis of the duodenal wall. The treatment of choice is conservative, although surgical intervention is sometimes necessary.52
Chronic obstructive pancreatitisAlthough this type of pancreatitis was defined at the Second Marseilles Symposium in 1984,15 both before and after that date processes that caused pancreatic duct obstruction and led to symptoms of pain and certain histological changes had been described in large and small series.53,54 There are multiple causes of obstruction, such as scarring from severe acute pancreatitis, pancreas divisum, tumours, periampullary lesions and trauma, etc. Duct obstruction generates lesions retrograde to the blockage. These lesions are evenly distributed and show inter- and intra-lobular fibrosis, with marked destruction of the exocrine parenchyma, loss of amylase concentration and the absence of calculi and protein plugs.55 One important characteristic is that both the morphological and functional alterations are reversible to a great extent if the cause of obstruction is suppressed at an early stage.
Chronic idiopathic pancreatitisThis is a heterogeneous pancreatitis group which was first distinguished in 1987 by Swiss physician Rudolf W. Ammann (1926–2015) from the Zurich Medezinische Poliklinik, based on prospective observations dating back to 1963 on 82 patients with chronic pancreatitis of unknown origin56 (Fig. 5). The distribution of age at onset of symptoms has enabled a distinction between two types of chronic idiopathic pancreatitis: one early-onset form that presents during the second decade of life and another late-onset type that manifests around the sixth decade. This differentiates them from chronic alcoholic pancreatitis, which usually appears between the third and fourth decades.56,57 The late-onset form is more common than the early-onset type and is characterised by being less painful, often beginning with signs of advanced endocrine and exocrine insufficiency (steatorrhoea and diabetes), weight loss and asthenia, which sometimes leads to a differential diagnosis with pancreatic cancer. The early-onset type usually develops with pain and follows a slower course that the late-onset form, with complications arising at a later stage.57 In 1998, Nicholas Sharer et al. of the Manchester Royal Infirmary, under the supervision of Indian doctor Joan M. Braganza, proved the existence of CFTR (Cystic Fibrosis Transmembrane Conductance Regulator) gene mutations in 15–45% of idiopathic pancreatitis cases, particularly early-onset types, without any of them showing signs of cystic fibrosis.23,58 More recently, in 2001, 8–40% of late-onset idiopathic pancreatitis cases were found to present the N34S mutation of the PSTI (Pancreatic Secretory Trypsin Inhibitor or SPINK1) gene. However, SPINK1 mutations are currently deemed to be more modifying factors than causes of the disease.23,59
This article does not reference the different techniques used to diagnose pancreatitis (laboratory methods, measurement of exocrine pancreatic function and imaging techniques) nor those for its medical or surgical treatment, since these form the basis of other publications.60,61
Conflict of interestsThe author declares that he has no conflicts of interest.
Please cite this article as: Navarro S. Pancreatitis crónica. Algunos aspectos históricos relevantes. Gastroenterol Hepatol. 2018;41:474.