Ischemic injury to the rectum is rare owing to its rich vascular supply, occurring in <6% of the cases of ischemic colitis.1,2 As in ischemic colitis, a spectrum of severity exists and ranges from superficial mucosal ischemia to full-thickness necrosis with perforation.3 Early recognition of this clinical entity is of vital importance in order to avoid complications.1 The authors report a series of 5 cases of acute ischemic colitis with rectum involvement and present review of the literature.
In this report, 5 patients were included, 4 man and 1 woman, with a median age of 70 year-old. The prevalence of cardiovascular risk factors was high (80%). All cases were admitted for lower gastrointestinal bleeding. None of the patients were taking nonsteroidal anti-inflammatory drugs in the days before presentation. In all patients who presented with bloody diarrhea, stool cultures (including Escherichia coli O157:H7), stool examination for ova (including Entamoeba histolytica) and parasites and Clostridium difficile toxin assay were obtained, and were negative. In 3 cases, a conservative approach was assumed due to their clinical stability and resolved without complications. The remaining 2 cases required a surgical approach and were admitted to an intensive care unit following surgery. One of these cases required multiple surgical procedures for complications. The median duration of hospitalization was 8 (IQR: 62) days, and all patients survived. The clinical features of each case are summarized in Table 1.
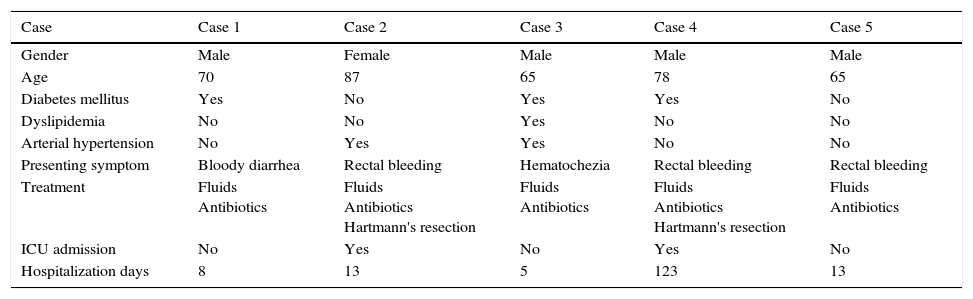
Clinical features of the patients with acute ischemic proctocolitis.
| Case | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 |
|---|---|---|---|---|---|
| Gender | Male | Female | Male | Male | Male |
| Age | 70 | 87 | 65 | 78 | 65 |
| Diabetes mellitus | Yes | No | Yes | Yes | No |
| Dyslipidemia | No | No | Yes | No | No |
| Arterial hypertension | No | Yes | Yes | No | No |
| Presenting symptom | Bloody diarrhea | Rectal bleeding | Hematochezia | Rectal bleeding | Rectal bleeding |
| Treatment | Fluids Antibiotics | Fluids Antibiotics Hartmann's resection | Fluids Antibiotics | Fluids Antibiotics Hartmann's resection | Fluids Antibiotics |
| ICU admission | No | Yes | No | Yes | No |
| Hospitalization days | 8 | 13 | 5 | 123 | 13 |
ICU: intensive care unit.
A report of each case is described below.
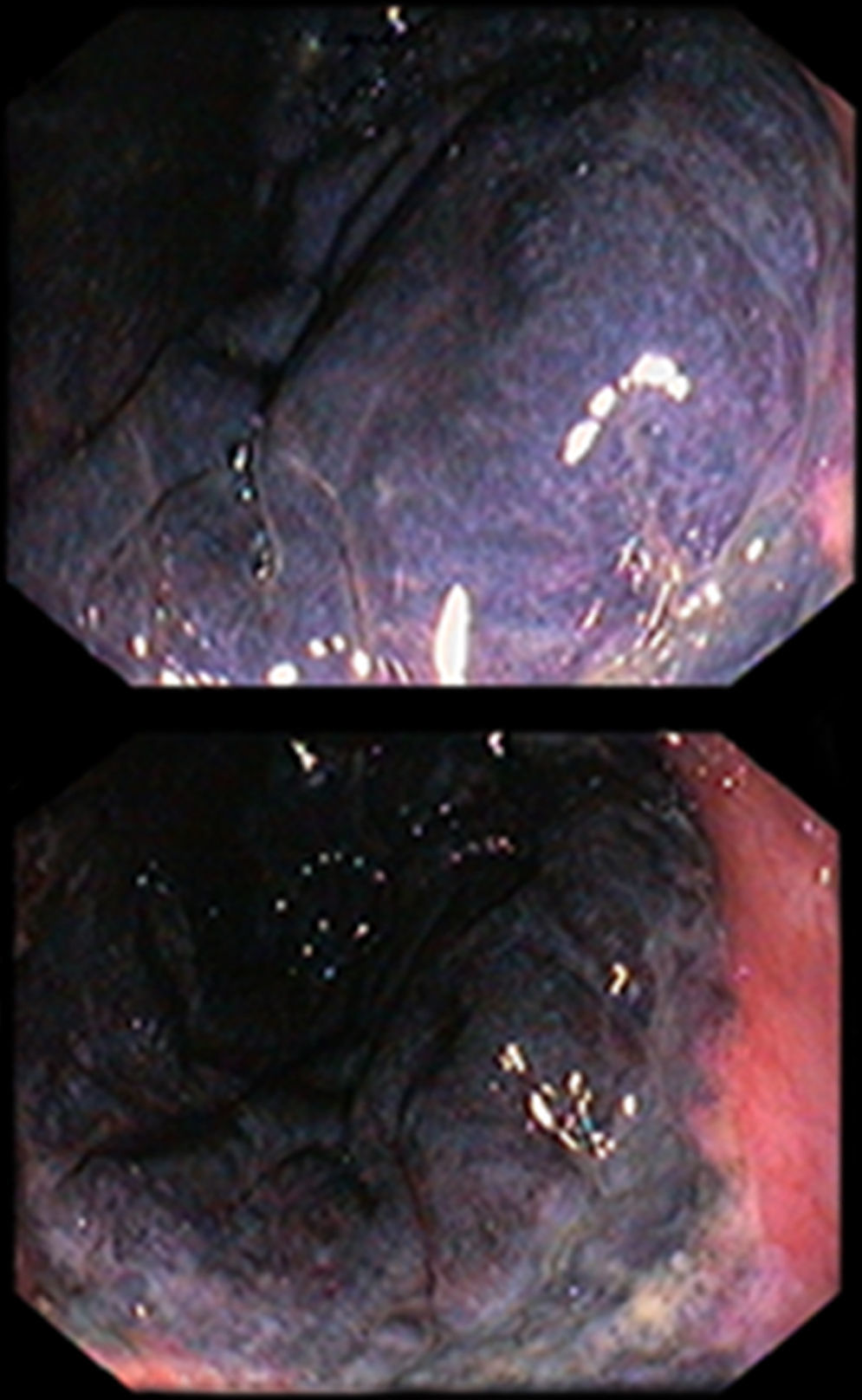
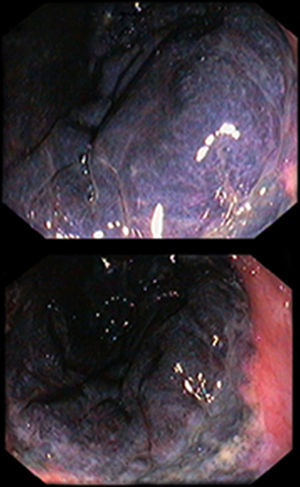
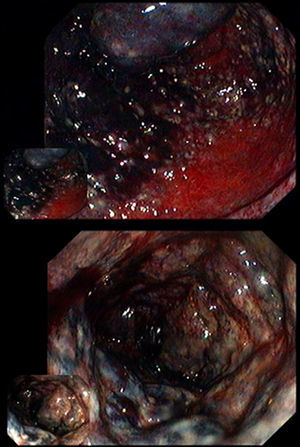
The first case concerns to a 70-year-old man, with a medical history of insulin dependent diabetes mellitus, left hemicolectomy for sigmoid adenocarcinoma (15 years before) and peripheral vascular disease requiring ileo-femoral bypass 4 months before. The patient was admitted for bloody diarrhea, nausea and vomiting. Proctosigmoidoscopy was performed and revealed a purplish black proximal rectal mucosa and edema (Fig. 1) consistent with ischemic proctitis that was confirmed by histological examination. The mucosa of the distal rectum was spared. A computed tomography (CT) scan was performed and showed signs of acute ischemia from the rectum to the transverse colon, with an abnormal opacification of the inferior mesenteric artery. Due to the clinical stable condition, a conservative approach was assumed and the patient started on broad-spectrum antibiotics. He was discharged 8 days after, asymptomatic.
The second case was an 87-year-old woman with arterial hypertension. She recurred to the emergency department for constipation and sudden crampy abdominal pain. She was treated on antibiotics for a urinary tract infection until 3 days before being admitted. The patient presented rectal bleeding in the emergency department. CT scan showed thickening of the sigmoid colon and rectal wall. She underwent a proctosigmoidoscopy which revealed erythema, edema and ulceration of the rectum, from 5cm proximal to the dentate line. Mild ischemic changes extended up to the splenic flexure. Biopsies were performed and the histopathological exam confirmed the endoscopic suspicion of ischemic proctocolitis. She was treated with fluids and broad-spectrum antibiotics, but on the 5th day of admission, due to clinical deterioration, a near complete proctectomy and Hartman's procedure were performed and she was admitted in an intensive care unit. The patient developed pneumonia with subsequent sepsis that resolved with targeted antibiotic treatment. She was discharged 13 days after.
The third case concerns to a 65-year-old man, with diabetes mellitus, dyslipidemia and arterial hypertension. He recurred to the emergency department for crampy abdominal pain and watery diarrhea followed by hematoquezia. He was tachycardic (116bpm), but normotensive. White blood count and the C-reactive protein were elevated (25,000 and 12.2mg/L, respectively). Patient was resuscitated with fluids and a proctosigmoidoscopy was performed showing marked inflammation with purplish friable mucosa of the rectum and distal sigmoid colon. He was also treated with fluids and broad-spectrum antibiotics and survived.
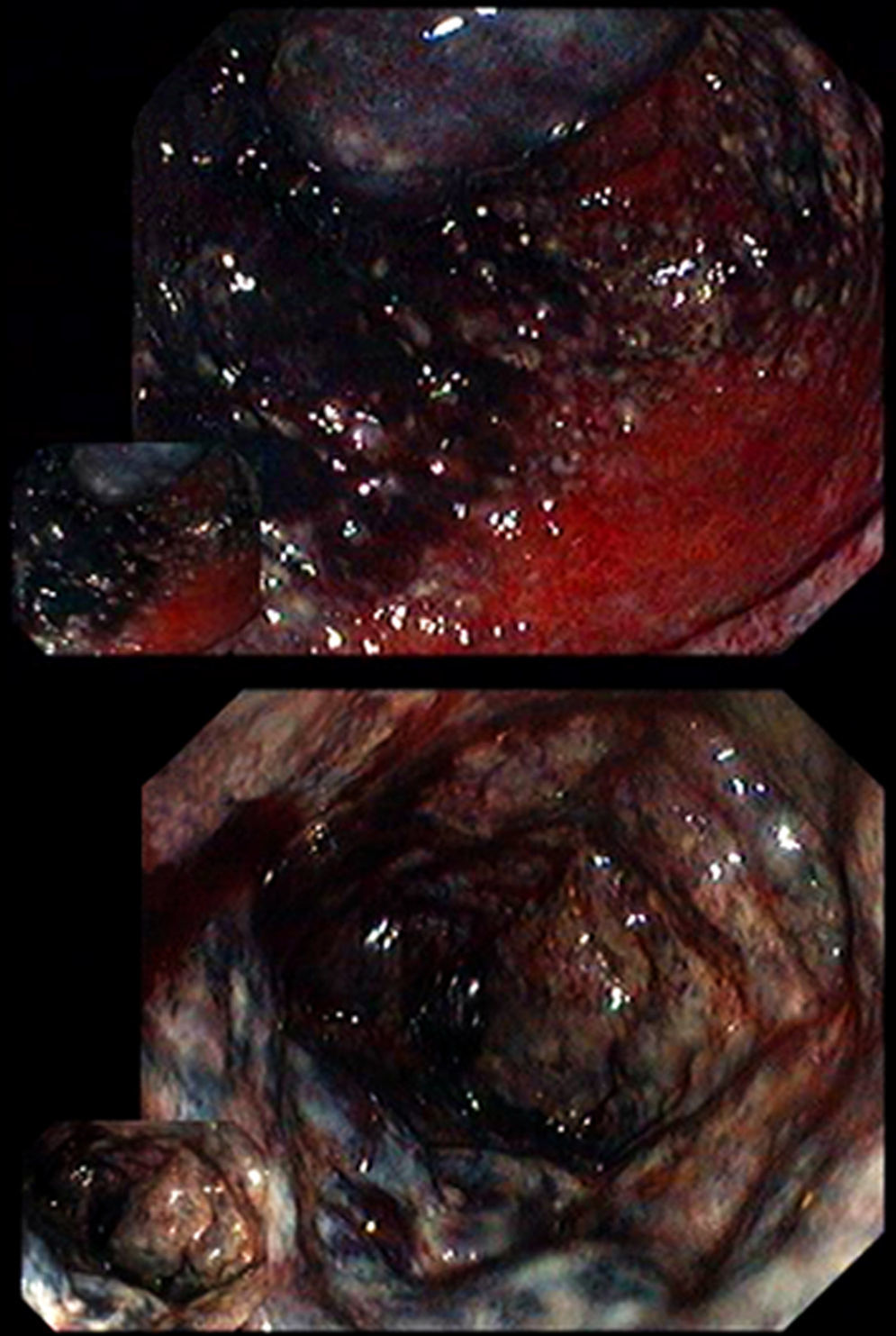
The fourth case relates to a 78-year-old man, with a medical history of ischemic heart disease, diabetes mellitus and a previous major amputation surgery (above-knee amputation of the left lower limb), 6 years before. The patient was admitted with rectal bleeding. A proctosigmoidoscopy revealed extensive proctitis with dark blue friable mucosa from the dentate line to 35cm from the anal verge (Fig. 2), consistent with ischemic proctitis that was confirmed in the histological exam. Due to hemodynamic instability and deterioration, a left hemicolectomy with colostomy, and Hartmann's closure were performed and the patient was admitted in an intensive care unit. After several surgical interventions due to septic complications and a prolonged and slow recovery, he was discharged to a nursing home after four months of hospitalization.
The fifth case relates to a 65-year-old man, with a past medical history of benign prostatic hyperplasia and peptic ulcer disease. He also had a history of smoking and alcohol abuse. He recurred to the emergency department for rectal bleeding, abdominal pain and vomits. White blood count and the C-reactive protein were elevated at 13,000 and 17mg/L, respectively. Proctosigmoidoscopy revealed erythema and superficial mucosa ulceration of the rectum and sigmoid colon mucosa. The histopathological exam of the biopsies performed was consistent with ischemic proctocolitis. He was treated on broad-spectrum antibiotics with subsequent mucosa healing. The patient was discharged 6 days after admission.
Ischemic colitis accounts for 1 in 1000 hospitalizations, but its incidence is underestimated because it usually has a mild and transient nature.2 Ischemic colitis is the condition that results when blood flow to the colon is reduced to a level insufficient to maintain cellular metabolic function.4 The degree to which colonic blood flow must diminish before ischemia results varies with the acuteness of the event, the degree of preexisting vascular collateralization, and the length of time the low flow state persists.4 Rectum has an extensive arterial supply network from the inferior mesenteric, internal iliac, internal pudendal arteries and the marginal artery.5 This rich collateral supply explains why colon and splenic flexure is involved in 75% of ischemic colitis but the rectum is involved in only 5% of cases.5 Ischemic proctitis is usually described in elderly patients with significant atherosclerotic disease and cardiac risk factors in the presence of hemodynamic instability.1
Most of the ischemic proctitis reported cases were secondary to previous vascular intervention, aortoiliac surgery, radiotherapy, hypotensive shock or a low flow state.5 These interventions or pathologies can lead to a sudden acute compromise in blood flow in patients with inadequate collateral circulation around the rectum and consequent ischemic damage.1 When ischemia of the rectum does occurs, the pathologic changes are the same as those seen in the colon. Transient ischemia results in mucosal edema and hemorrhage, which is generally reversible, but prolonged ischemia results in mucosal necrosis with ulceration and eventual transmural necrosis with gangrene or perforation in the most severe cases.3
Although the majority of our patients had several cardiovascular risk factors, including diabetes mellitus in 3 cases and peripheral arterial disease in 2 of them, none of the patients had an acute preceding event, like those cases reported by Reinus et al.6 and Azimuddin et al.1 In fact, spontaneous ischemic proctitis is a very rare event, accounting for less than 2% of all cases of ischemic colitis.5
Clinical presentation of patients with ischemic proctitis may be non-specific and often misleading, since they often present with lower abdominal pain, diarrhea with bloody discharge and proctalgia, also commonly seen in other colorectal diseases.5 In this context clinical index of suspicion for this disease is extremely low. Although CT scan can suggest the diagnosis and identify other causes of clinical deterioration, the findings of CT scan are often nonspecific and misleading and cannot determine the severity of the condition.2 Colonoscopy remains the cornerstone for diagnosis and to determine the extension of the ischemic lesion and should be performed within 48h of presentation in suspected cases.4 The histological examination can confirm the diagnosis.1,2 Given the broad differential diagnosis and the inaccuracy of diagnosis based upon clinical presentation, initial evaluation with serology and stool studies, including, stool culture, stool examination for ova and parasites and C. difficile toxin assay, are recommended.4
The clinical presentation of all of our patients was undistinguishable of cases with ischemic colitis without rectum involvement. Only after proctosigmoidoscopy or CT scan had been performed, ischemic proctitis was suspected.
Treatment management is determined by endoscopic findings and the overall clinical parameters. Early restoration of the patient's blood volume and optimization of the cardiac output is of paramount importance in the initial management of these patients.7 Conservative management is normally sufficient for the majority of cases with nongangrenous ischemic proctitis.8 These cases can be managed conservatively with broad-spectrum antibiotics and close observation for signs of sepsis or perforation.1,7
Full thickness bowel wall necrosis or perforation is associated with high mortality and surgical resection becomes necessary in such situations.1,8 In most cases a complete proctectomy is required and, in an emergent situation, this is best accomplished by an abdominal perineal resection. In cases which the lower rectum is spared, like two of our cases, a low anterior resection of the rectum along with a Hartman's procedure may be performed. It is not recommend leaving behind a gangrenous or ischemic segment of the rectum.9
Contrary to other reported series, all the patients here presented survived.3,8 This fact may be explained by a faster approach with fluid resuscitation and institution of broad spectrum antibiotics. In all cases, a bedside proctosigmoidoscopy was performed allowing a correct diagnosis without delays. In addition, none of our patients had an acute preceding event, which can suggest that these patients had less severe comorbidities than other reported cases.
In conclusion, ischemic colitis with rectal involvement is a condition difficult to diagnose clinically because of its rarity and close resemblance in clinical presentation to other pathological conditions. Ischemic proctitis should be investigated in the differential diagnosis of lower-gastrointestinal bleeding, especially for elderly, bedridden patients with atherosclerotic disease. Although all the presented cases survived, in two patients a surgical intervention and admission on a intensive care unit were necessary, which reinforces the potential severity of this condition. Early recognition of this clinical entity is fundamental in order to implement appropriate therapy and avoid potentially fatal complications.
Conflicts of interestNone declared.