INTRODUCTION
Prevalence rates of chronic diarrhoea in Western population have been reported to be of 4-5% when defined by an excessive stool frequency without the presence of abdominal pain1. The etiologic study of chronic diarrhoea usually includes a detailed anamnesis, routine blood (with acute phase reactants, and thyroid hormones), stool examination and cultures, and serological tests for coeliac disease. Imaging studies are almost always necessary, and colonoscopy is required even to achieve a diagnosis of irritable bowel syndrome. Barium-meal X-ray follow-through is performed only in case of biological abnormalities and normal colonoscopy, or in clinical suspicion of small bowel disease. Although microscopic colitis had been considered a rare gastrointestinal disorder, it is a fairly common cause of chronic watery diarrhoea, particularly in middle-aged and elderly women. Recent epidemiological data report an incidence rate of 4-6/100,000, and a prevalence of 10% among patients with chronic watery diarrhoea, so it is recommended to perform routinely colonic biopsies in patients with these symptoms and normal endoscopic features2,3. We report an uncommon case of collagenous colitis, with duodenal and ileal involvement, transient IgG deficiency, that followed an intestinal Yersinia enterocolitica infection.
CASE REPORT
A 53 year-old Caucasian man was admitted to our hospital for chronic diarrhoea.
He had a past medical history of parotiditis complicated with orchitis. Thyroidectomy had been performed 25 years before the present admission for hyperthyroidism; the patient had been under substitution therapy and remained clinically assymptomatic. He was a current smoker of 10 cigarettes/day.
Two months before, he started with watery diarrhoea (4-5 motions/day) without blood or mucus, but with urgency, tenesmus, and abdominal cramps which relieved with defecation. Although his appetite was unchanged, the patient reported a weight loss of 12 kg. There were no epidemiologic risk factors for infectious diarrhoea. One month prior to hospital admission, Yersinia enterocolitica infection, sensitive to ciprofloxacin, was diagnosed in another hospital by stool culture. The patient completed antibiotic therapy without clinical improvement. Moreover, the patient returned twice to emergency room for dehydration and persistence of symptoms.
On examination, he was apyretic, and appeared healthy. Vital signs were normal. There were no nodes. His chest was clear and his heart sounds were normal. There was a widespread tenderness on pressure in the abdomen. Rectal examination was normal. Blood tests showed normal haematologic parameters, with mild hyperfibrinogenemia of 583 mg/dl, but normal ESR and CRP levels. Liver function tests, renal function, and protein and cholesterol levels were within the normal range. Thyroid hormones were normal and serologic screening for celiac disease was negative. Serum IgA and IgM levels were normal, but a mild IgG deficiency was noticed (476 mg/dl [normal range, 700 to 1,400]). HIV serology was negative. Repeated stool cultures, exam for parasites, and determination of Clostridium difficile toxine were all negative. Small bowel follow-through, abdominal CT scan, gastroduodenoscopy, and colonoscopy were also normal, but aftous mucosal erosions were noticed at ileoscopy. Endoscopic ileal biopsies were performed, demonstrating a mild increase of intraepithelial lymphocytes and a broad and irregular subepithelial, trichrome-positive band of collagen in the superficial lamina propria (fig. 1). Similar findings were seen in mucosal duodenal biopsies that had been taken to rule out celiac sprue. Given the histological findings in ileal biopsies, endoscopic specimens were obtained from the colon (fig. 2).These biopsy samples were diagnostic of collagenous colitis.
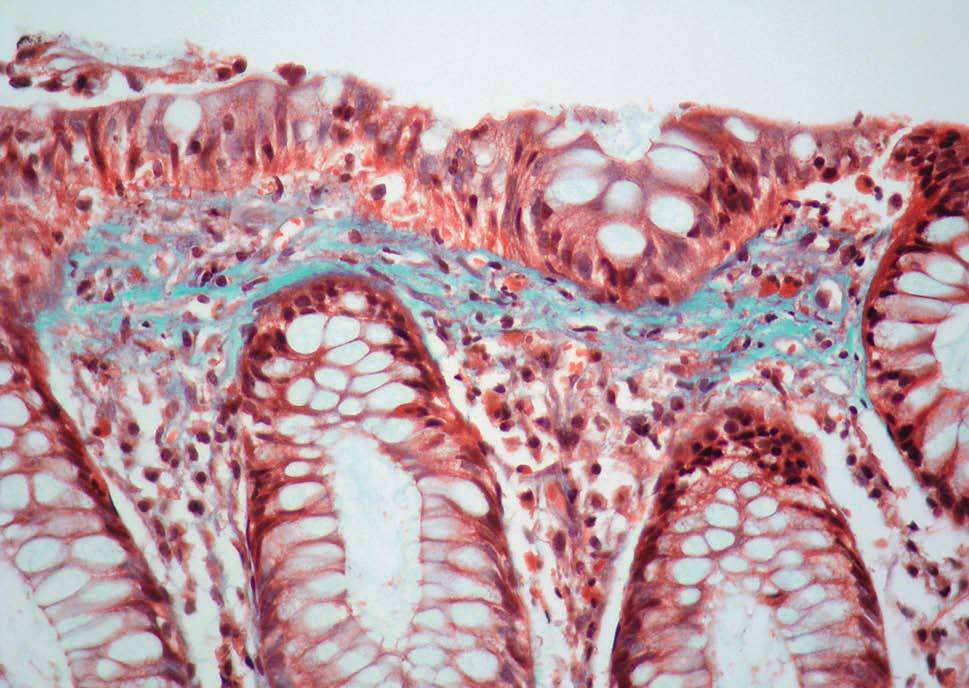
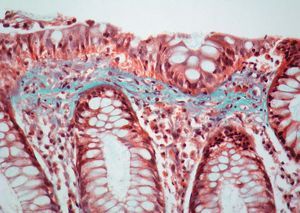
Fig. 1. Colonic biopsy showing a slight increase in intraepithelial lymphocytes and a subepithelial thick band of collagen with an irregular low border entrapping inflammatory cells and small capillaries (trichrome stain3400).
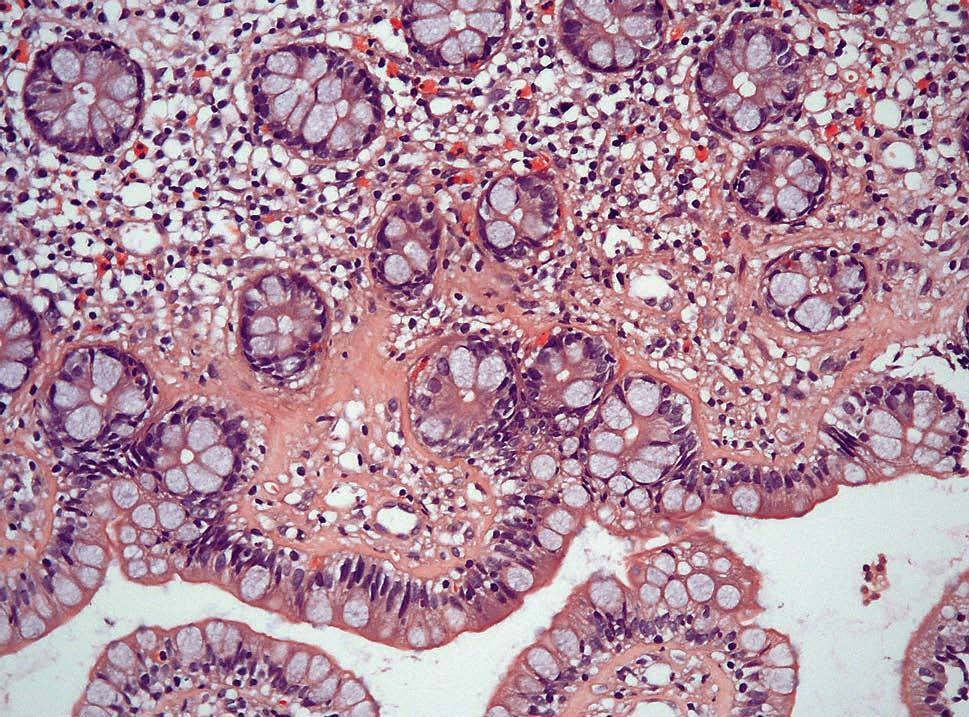
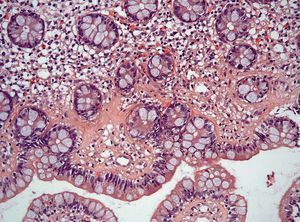
Fig. 2. High power photomicrograph of the ileal biopsy. In spite of the slight tangential sectioning an inflammed lamina propria can be seen, and a irregular collagen table extending down into its upper portion with a spiculated low border. It also contains small capillaries (haematoxylin-eosin3400).
The patient did not tolerate cholestyramine, and oral mesalazine was started with only a partial clinical improvement. The treatment was then switched to oral budesonide that could be completely withdrawn 6 months later without clinical relapse after two years of follow-up.
DISCUSSION
Collagenous colitis (CC) was first described by Lindstrom in 19764, whereas lymphocytic colitis (LC) was later proposed to emphasize the predominant cell type present in some cases5. Both were then classified as microscopic colitis (MC) to differentiate these entities from other intestinal inflammatory bowel diseases with abnormal imaging techniques6. MC is characterized by chronic watery diarrhoea, normal radiological and endoscopic appearance, and microscopic abnormalities in the colonic mucosa. Main pathologic lesions are a subepithelial collagen band ($ 10 mm) adjacent to the basal membrane in CC, and an increased number of intraepithelial lymphocytes in LC. Both diseases display inflammatory changes in the lamina propria, and superficial epithelial damage. CC and LC share a similar clinical picture, with a benign and sometimes relapsing course7-9.
The aetiology of MC is still unknown, although an immunological origin has been suggested because of its association to autoimmune diseases such as celiac disease or thyroiditis. In addition, the consumption of some drugs (mainly NSAIDs, lansoprazole, venotonic drugs, ticlopidine) has also been associated to the development of MC, and, in these patients, drug withdrawal may be enough to control clinical symptoms8. In the present case, there was a past history of hyperthyrodism and no drug consumption in the previous months was recorded. Despite microbiological studies are usually negative, it has been suggested that some infections may trigger MC onset9-11. Our patient had an intestinal yersioniosis at initial presentation, but adequate antibiotic treatment did not result in diarrhoea resolution. Makinen et al10 reported three cases of CC and Yersinia enterocolitica infection but, as in our case, antibiotic therapy had no effect on their clinical course. Some chronic inflammatory conditions such as autoimmune thyroid disease, ankylosing spondylitis, hemochromatosis, and other HLA-associated autoimmune disorders may predispose to Yersinia enterocolitica infection, and this could be also the case in MC. Bohr et al showed that Yersinia antibodies were more common in collagenous colitis patients than in healthy controls.
Duodenal and ileal involvement was demonstrated in the present case. There is increasing evidence that collagenous inflammatory mucosal disease is a far more extensive pathologic process that concomitantly may involve multiple sites in the gastric and intestinal tract mucosal, as described in several case-reports12-21. However, only two studies have evaluated the involvement of the terminal ileum in MC patients. Padmanabhan et al22 described a significant increase in intraepithelial T lymphocytes compared with the control group in 50% of CC patients and 78% of LC patients; however, thickened subepithelial collagen was observed in only 14% of CC cases. These authors reviewed duodenal biopsies from 8 patients with MC, but subepithelial collagen was present in only one of them. Sapp et al23 studied the histological changes in the terminal ileum from 22 patients with LC and 23 with CC. Although a significant increase in IELs was seen in MC compared with controls or patients with inflammatory bowel disease, the presence of subepithelial collagen was not evaluated.
To our knowledge, only three cases of CC and immunoglobulin deficiency have been reported. Two of them were associated to autoimmune diseases: IgA deficiency, Grave's disease, and chronic autoimmune atrophic gastritis in one24, and IgG deficiency, thyroid node and atrophic gastritis, in the second25. Only one case26 had a common variable immunodeficiency (IgA and IgG deficiency), which is known to be associated with an increased risk of infections, malignancies, and autoimmune conditions. A recent review of gastrointestinal pathology in 43 patients with common variable immunodeficiency did not reveal any cases of CC27. Moreover, IgG deficiency in our patient was transient, and normal levels of IgG were noticed three months after a successful treatment for CC with oral budesonide was started. In turn, immunoglobulin deficiency does not seem to be a common risk factor for MC.