Verruciform xanthoma (VX) is an uncommon benign lesion of unclear etiology which has only been reported twice before in the esophagus. We describe a 70-year-old male who presented an exophytic esophageal lesion incidentally found upon endoscopy 2.7 years following radiation therapy for unresectable squamous cell carcinoma of the tracheal carina. Histologically, the lesion showed a papillary surface change with numerous foamy histiocytes within the lamina propia papillae. Xanthoma cells were strongly positive for vimentin and CD68 (KP1). Polymerase chain reaction did not demonstrate human papillomavirus (HPV) infection. Our results indicate that esophageal VX is not an HPV-induced lesion and suggest a causal relationship between VX and radiotherapy, as previously noted. Histological differential diagnosis is discussed and emphasis is placed on obtaining adequate biopsy material for accurate diagnosis.
El xantoma verruciforme (XV) es una lesión benigna poco frecuente y de etiología desconocida que se ha documentado solo dos veces en el esófago. Se describe a un varón de 70 años de edad que presentaba una lesión exofítica de esófago, descubierta de forma incidental durante una endoscopia 2,7 años después de recibir radioterapia por un carcinoma escamoso en la carina traqueal sin posibilidad de resección. Histológicamente, la lesión mostraba una superficie papilar, con numerosos histiocitos espumosos dentro de las papilas de la lámina propia. Las células xantomatosas resultaron positivas para vimentina y CD68 (KP1). La reacción en cadena de la polimerasa no detectó la presencia del virus del papiloma humano (VPH). Nuestros resultados indican que el XV esofágico no es una lesión inducida por el VPH, y sugieren una relación causal entre el XV y la radioterapia, como ya se ha señalado con anterioridad. Se realiza el diagnóstico diferencial histológico y se hace hincapié en la obtención de material de biopsia adecuado para llevar a cabo un diagnóstico preciso.
Verruciform xanthoma (VX) is a rare asymptomatic lesion that occurs predominantly in the oral mucosa,1–6 although extra-oral involvement has also been reported mainly in the anogenital region.7–10 Their occurrence in the esophagus is extremely rare,11,12 probably related to local irritation or trauma such as caused by radiation therapy. We report herein the third case of esophageal VX reported in the literature, the second one related to prior radiotherapy.
Case reportThe patient is a 70-year-old man who had a medical history of longstanding hypertension, primary hemochromatosis and chronic hepatitis C infection. He had been a smoker for several years. In March 2004, he was subjected to total laryngectomy and bilateral neck dissection without radiation therapy for a squamous cell carcinoma of the glottis. Follow-up imaging for liver disease discovered a 5cm tumor in the segment VI of the right hepatic lobe, consistent with liver cell carcinoma, which was excised by partial right hepatectomy in December 2006. In October 2007, the patient presented with hemoptysis and bronchoscopy demonstrated an ulcerated lesion suspicious of malignancy on the tracheal carina. Biopsy revealed an squamous cell carcinoma. The patient received external beam 3D radiotherapy, with a total dose of 60Gy. A total of 30 sessions with a fractionation of 5×200cGy were administered. Concomitant chemotherapy was given, with weekly paclitaxel (60mg/m2) and carboplatin (AUC 2). 33 months after last session of radiotherapy, routine esophagogastroduodenoscopy revealed an elevated, hyperkeratotic white-yellowish mucosal lesion, 2cm in diameter, in the upper third of the esophagus at 20cm from dental arcade. The endoscopical diagnosis was concordant with cicatricial mucosal changes following radiotherapy and a biopsy was taken.
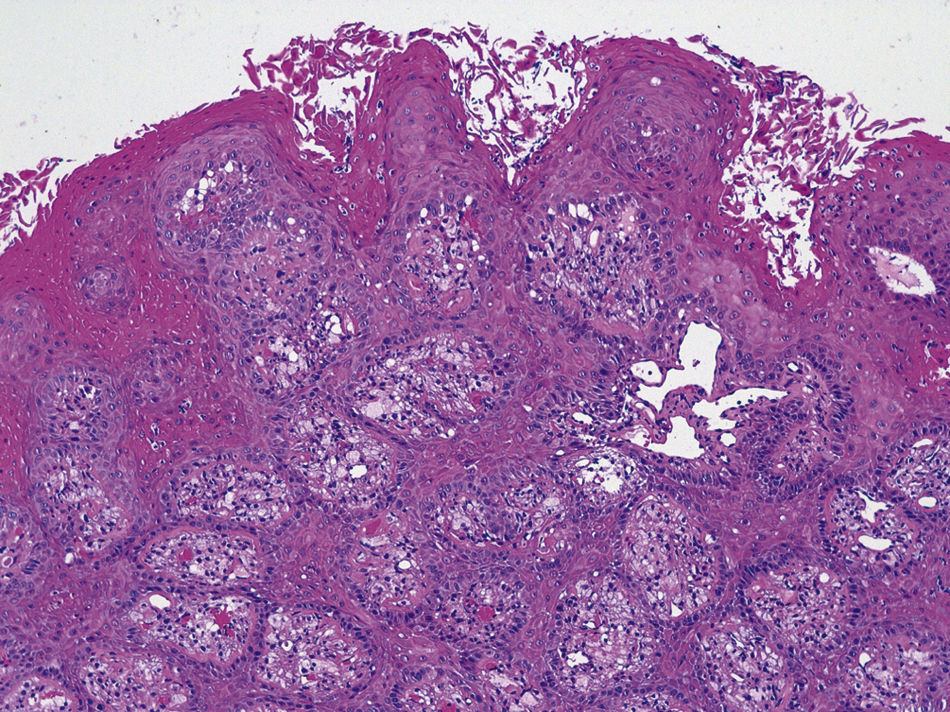
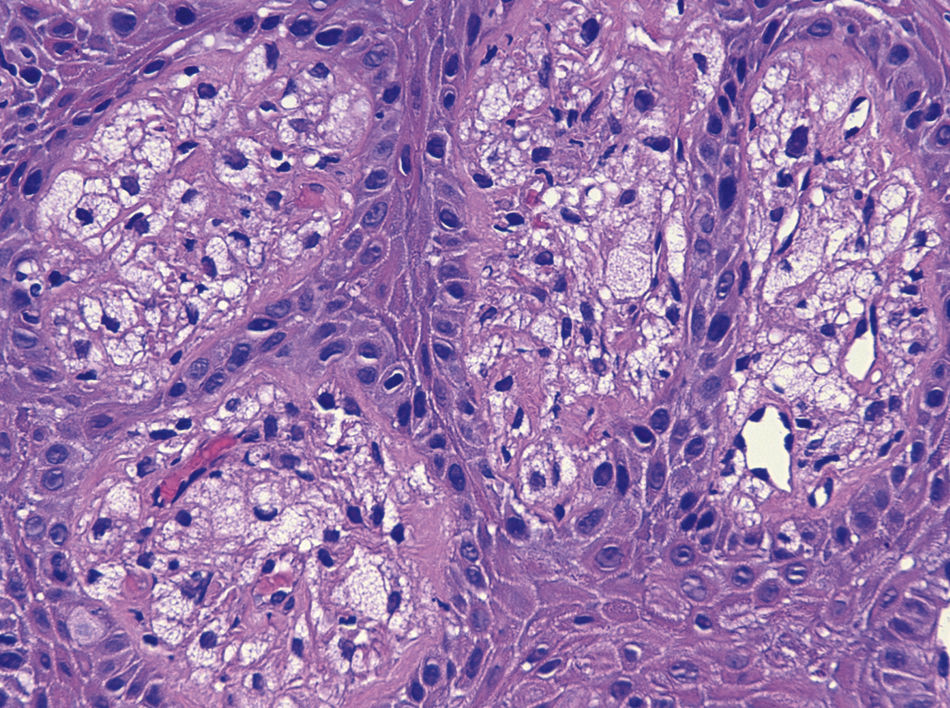
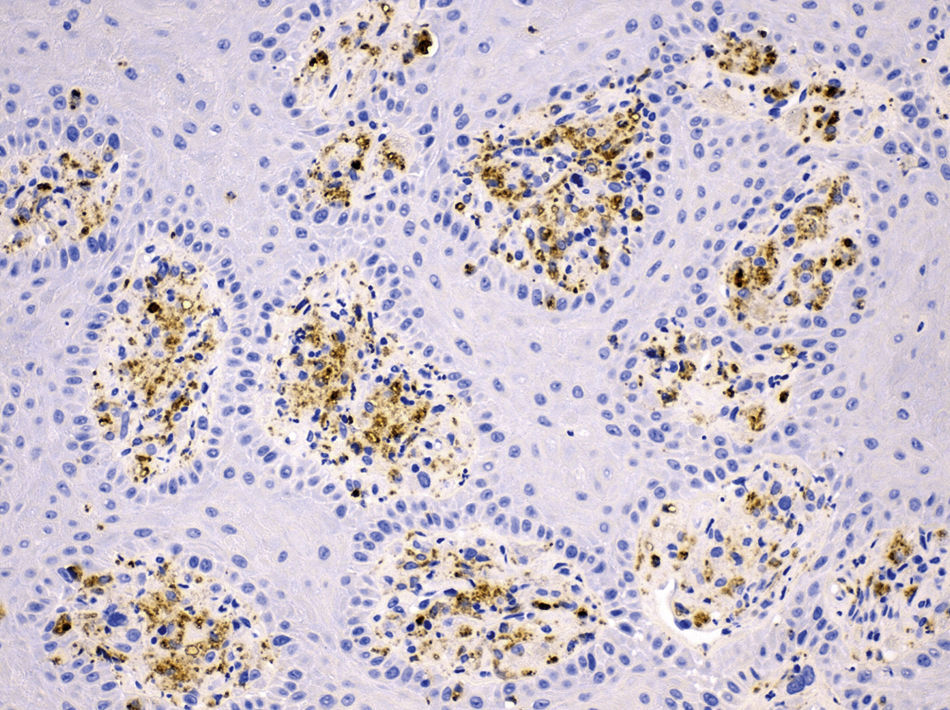
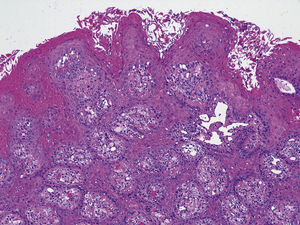
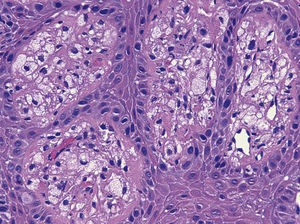
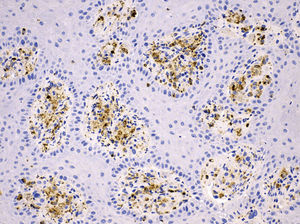
The entire biopsy specimen was routinely fixed, processed, and stained with hematoxylin–eosin. Microscopically, the lesion was characterized by an epithelial mucosa with papillomatosis, acanthosis with elongated rete ridges without cellular atypia, hyperkeratosis with a prominently eosinophilic thickened parakeratin layer, and neutrophilic intraepithelial exocytosis. The connective tissue papilla between the epithelial pegs contained large numbers of xanthoma cells with small nuclei with no atypia, and abundant granular cytoplasm which did not stain with the periodic acid–Schiff (PAS) technique. Telangiectatic vessels were also observed focally (Figs. 1 and 2). Immunohistochemically, foam cells were intensely stained with vimentin and the monoclonal antimacrophage antibody CD68 (KP1) (Fig. 3), while CKAE1/AE3 and S-100 protein were negative. Based on these findings, the pathologic diagnosis was “verruciform xanthoma of the esophagus”. Polymerase chain reaction (PCR) was performed to amplify a 150bp fragment from the L1 region of human papillomavirus (HPV) DNA using the GP5+/6+ primers set (MD Diagnostics, Hong Kong). Appropriate controls were included. No HPV infection was detected in the biopsy.
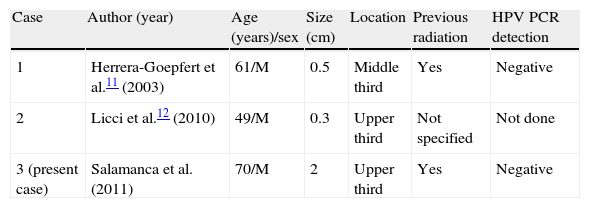
Verruciform xanthoma (VX) is an uncommon benign lesion first described by Shafer in 1971.1 Seventy percent occur primarily on the oral cavity of adults1–6 but lesions on the skin (especially of the anogenital area) and other mucosal sites have also been reported.7–10 However, their occurrence in the esophagus is extremely rare with only two previously published case reports.11,12 Their clinical data are summarized in Table 1.
Clinical finding and HPV results of current and previously reported cases of verruciform xanthoma of the esophagus.
| Case | Author (year) | Age (years)/sex | Size (cm) | Location | Previous radiation | HPV PCR detection |
| 1 | Herrera-Goepfert et al.11 (2003) | 61/M | 0.5 | Middle third | Yes | Negative |
| 2 | Licci et al.12 (2010) | 49/M | 0.3 | Upper third | Not specified | Not done |
| 3 (present case) | Salamanca et al. (2011) | 70/M | 2 | Upper third | Yes | Negative |
HPV: human papillomavirus: PCR: polymerase chain reaction.
Although its pathogenesis remains unclear, VX may represent an unusual reaction to localized epithelial trauma or damage. In 2003, Herrera-Goepfert et al.11 reported the first case of esophageal VX in a patient who received thoracic radiotherapy for systemic non-Hodgkin lymphoma. The authors speculate that mediastinal irradiation might play a major role in the development of VX of the esophagus. The fact that our patient received radiation therapy during his treatment course also supports this hypothesis. In the esophageal VX reported by Licci et al.12 no information is provided concerning prior history of radiation. The effects of therapeutic treatment for primary head and neck cancer (HNCA) in the esophagus have been well documented. Recently, Farwell et al.13 determined the prevalence of esophageal pathology in 100 patients at least three months after treatment for HNCA. Eighty-five subjects (85%) had radiation therapy at some point in their treatment. The most common findings were peptic esophagitis, esophageal stricture, esophageal candidiasis, Barrett metaplasia, and carcinoma. Although VX was not found in any of patients, we believe that with the increasing use of radiation therapy for head and neck or mediastinal cancer, radiation-associated VX cases could occur more frequently in the future. Other authors have also suggested the possibility that HPV is etiologically related to this condition.14,15 However, our case was negative on PCR screening for HPV, as was the case reported by Herrera-Goepfert et al.11 HPV detection was not performed in the case reported by Licci et al.12 (Table 1).
A verruciform xanthoma clinically manifests itself as an asymptomatic, small, elevated, verrucous pink-yellowish mucosal lesion. It is usually solitary, as found in our case and the other two esophageal cases reported. Histologically, the lesion is characterized by a papillomatous surface with elongate rete processes, a prominently eosinophilic thickened parakeratin layer and an associated neutrophilic infiltrate. The hallmark is the presence of large, vacuolated foam cells (xanthoma cells) in the lamina propia.
In the esophagus, the histological differential diagnosis includes benign lesions such as squamous papilloma and granular cell tumor. Most important is the distinction between VX and malignant tumors such as verrucous carcinoma, papillary squamous cell carcinoma or signet ring cell carcinoma to avoid unnecessary extensive surgical intervention.
Squamous papilloma is the most common benign tumor of the esophagus. Although it may be associated with an inflammatory infiltrate, they do not contain foam cells and may exhibit varying features of HPV infection such as koilocytosis, which are known to be absent in VX.
The gastrointestinal tract is a relatively uncommon site for the development of granular cell tumors (GCTs), but within that organ system, the esophagus is the most common location. Granular histiocyte-like cells of GCT are typically PAS (with diastase) and S100-positive. Although pseudoepitheliomatous hyperplasia can occur, the surface papillary alteration seen in VX is not usually present.
Papillary squamous cell carcinoma can be distinguished from VX by its cellular atypia, atypical mitoses, invasion, and lack of xanthoma cells.
VX and verrucous carcinoma (VC) both share a marked acanthosis with minimal or no atypia. In VC, however, the epidermal downgrowth takes the form of bulbous processes rather than relatively narrow ridges. The recognition of xanthoma cells in VX will effectively rule out VC.
Histiocytes are usually readily distinguished from signet ring cell carcinoma by their lack of nuclear enlargement and atypia on routine H&E staining. In questionable cases, immunohistochemical stains for CD68 and cytokeratin can be performed.
The differential diagnosis is obviously problematic when biopsies are taken too superficially, allowing only evaluation of the epithelium. It is therefore important that at least some lamina propia is present in the biopsy specimen.
In summary, we report the exceptional presentation of a VX in the esophagus of a 70 year-old male. Endoscopists and pathologists should consider the possibility of VX in the differential diagnosis of esophageal exophytic lesions in patients treated with radiotherapy. We emphasized the well-defined pathological features of this lesion and the importance of adequate biopsy material including a good epithelial stromal interface in order not to misdiagnose VX as a malignant tumor to avoid an inappropriate esophaguectomy.
Conflict of interest statementThe authors declare no conflict of interest.