The duodenum is the most common site of intestinal atresia, with an incidence of one in every 10,000–40,000 births. A duodenal web (type I duodenal atresia) presents in the form of a diaphragm that consists of mucosa and submucosa and causes incomplete endoluminal obstruction. It is usually located at the ampulla of Vater or a few millimeters distal to this structure. More than 30% of cases are associated with Down syndrome, close to 40% present heart defects and up to 70% are associated with intestinal malrotation.
The clinical presentation depends on the size of the stenosis. It typically manifests in neonates, in the first few hours or days of life, in the form of vomiting and abdominal distension. If there is late clinical onset, symptoms may be less obvious and manifest as delayed growth, abdominal distension or recurrent respiratory infections.
The typical treatment for this disease is surgical; usually, a bypass through duodenoduodenostomy is performed. Experience with endoscopic treatment is limited, and few cases involving dilatation and/or incision techniques have been published. The largest case series published consists of 4 neonate patients who underwent pneumatic dilatations through interventionist radiology1.
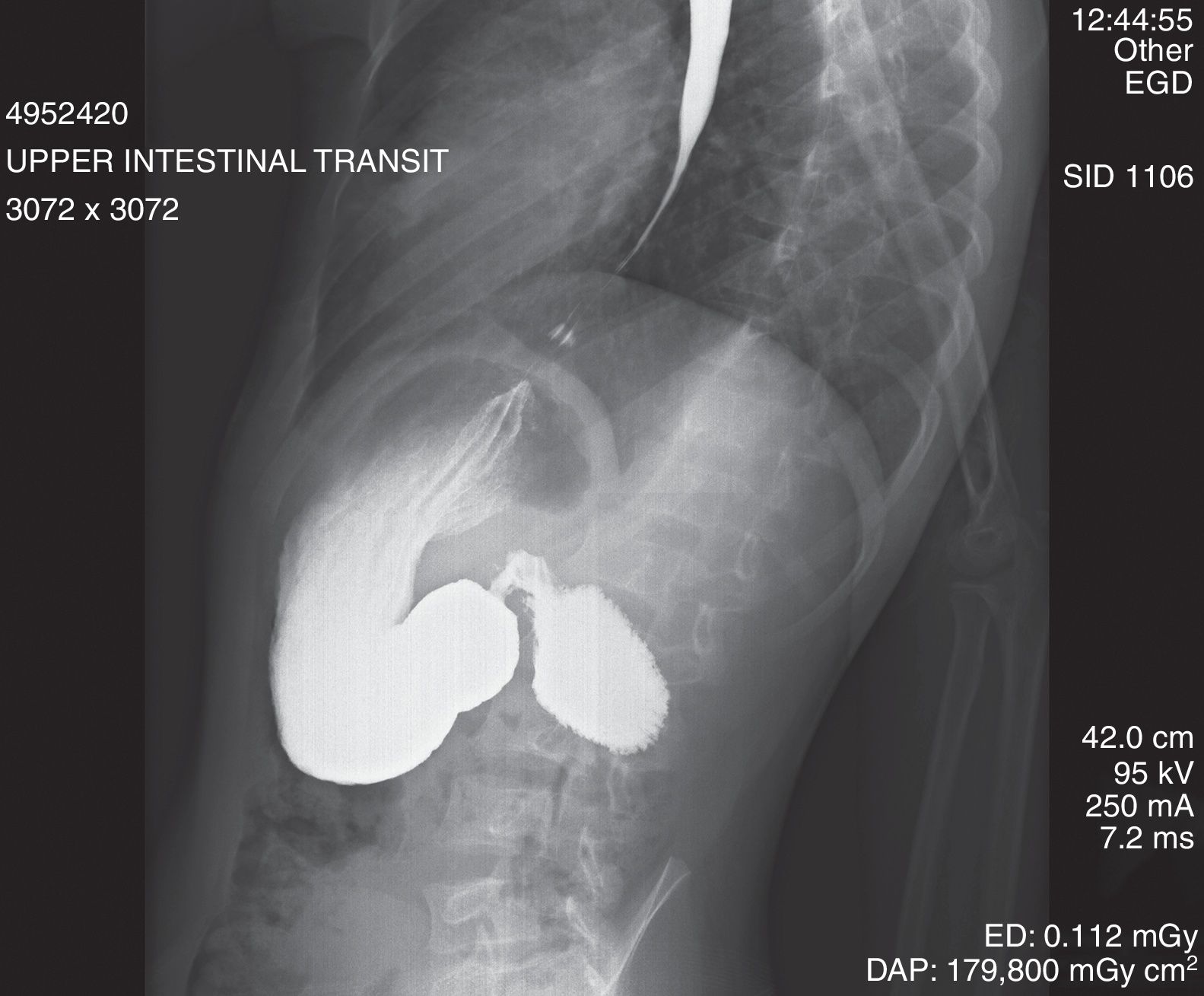
We present the clinical case of an 8-year-old patient with Down syndrome and delayed growth who presented signs and symptoms of vomiting which had started 6 months earlier. A simple X-ray of the patient's abdomen and gastrointestinal transit (Fig. 1) showed extensive dilatation of the stomach and duodenum (“double bubble” sign), with contrast retention and limited distal aeration. Gastroscopy showed partially digested food in the stomach and extensive dilatation of the duodenal bulb with stenosis in the form of a fenestrated membrane, featuring a central opening measuring 5mm.
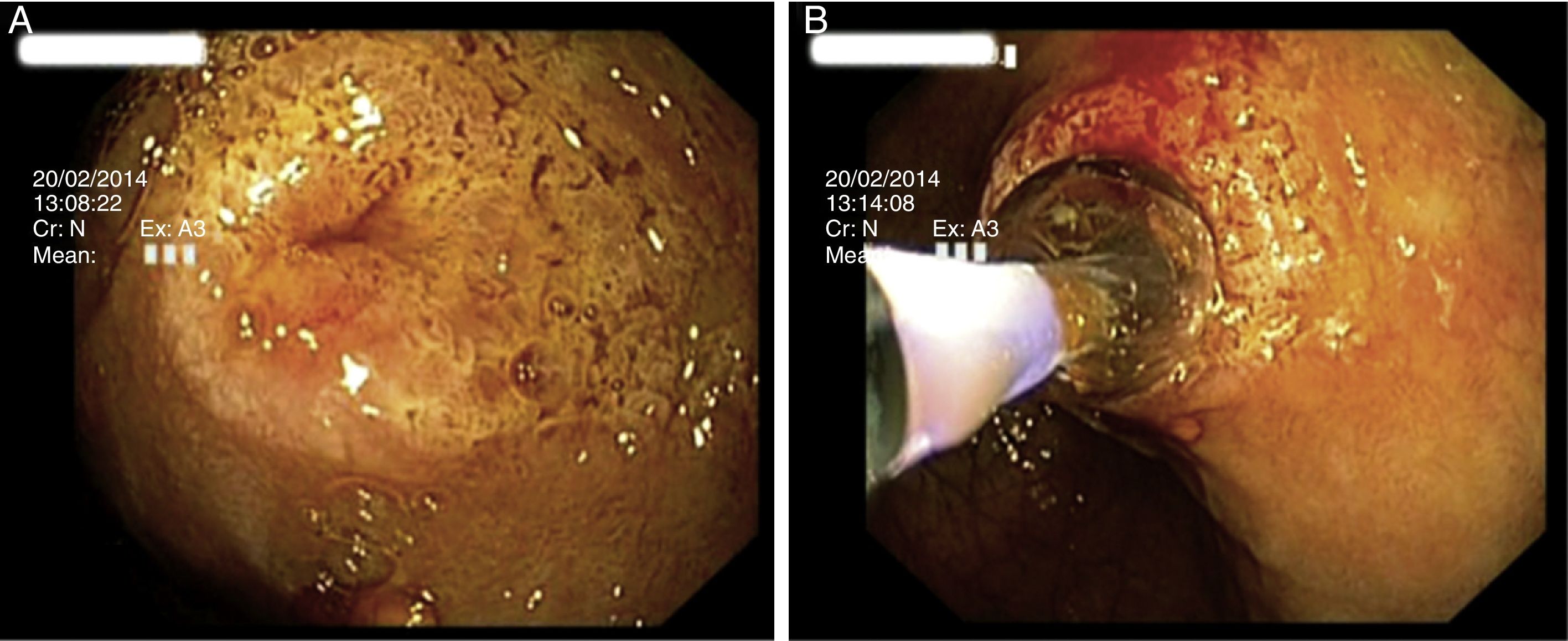
Following joint assessment by the pediatric surgery and gastrointestinal medicine departments, it was decided to treat the patient through a series of endoscopic dilatations with a pneumatic balloon. A total of 2 dilatation sessions were performed under radiological monitoring using a pneumatic dilatator with controlled radial expansion (CRE®, Boston Scientific) from 8mm to 12mm (Fig. 2). No complications arose, and complete remission of symptoms was achieved. All gastroscopies were performed in an operating theater with the patient intubated and managed by an anesthetist.
(A) Endoscopic view at the level of the 2nd segment of the duodenum of fenestrated membrane stenosis, with slightly erythematous villous mucosa, which did not allow the passage of the standard endoscope. (B) The stenosis was cannulised, a stent was passed, the CRE dilatation balloon was slid over this and gradual pneumatic dilatation was performed. The wrinkled appearance of the mucosa folded over the balloon may be seen.
After 5 years had elapsed since treatment, the patient experienced a recurrence of signs and symptoms with vomiting and malnutrition parameters. A gastrointestinal transit study showed an enlarged stomach with good passage of contrast through the pylorus and extensive dilatation of the duodenal bulb and the second segment of the duodenum. Distal passage of contrast was not achieved due to stenosis there. Given the reappearance of the patient's symptoms, it was decided to restart the pneumatic dilatation protocol. As initially the stenosis did not allow the passage of the pediatric gastroscope, the first gastroscopy was performed under radiological monitoring. It identified a short stenosis measuring 10mm. A total of 9 sessions were performed with successive dilatations from 8mm to 18mm, with no immediate complications. The patient gradually showed resolution of signs and symptoms with weight gain. However, 48h after the last dilatation, the patient presented abdominal pain and fever. An abdominal CT scan identified bubbles of ectopic air in the second segment of the duodenum consistent with microperforation. The patient underwent conservative treatment initially and elective surgery as a definitive treatment 10 days later. The surgery performed was a complete duodenal resection with gastrojejunostomy.
Cases of congenital duodenal web treated endoscopically are limited. Isolated cases and very short case series have been published with good outcomes using pneumatic dilatations, incision with a precut needle-knife or submucosal dissection combined with membranectomy with a polypectomy loop2–5; however, these have reflected short-term outcomes.
Pneumatic dilatation is a relatively safe technique, although it is not free of risks and complications. The decision to perform endoscopic treatment in cases of duodenal web should be multidisciplinary, taking into account the experience of the endoscopist and the availability of pediatric surgeons. In our experience, pneumatic dilatation is probably not a technique with long-term effectiveness as a sole treatment for a duodenal web.
Please cite this article as: Sanahuja Martínez A, Peña Aldea A, Sánchiz Soler V, Villagrasa Manzano R, Pascual Moreno I, Mora Miguel F. Tratamiento endoscópico de una membrana duodenal fenestrada mediante dilatación. Gastroenterol Hepatol. 2018;41:369–370.