Granulomatous gastritis (GG) is a rare entity that is characterized by the presence of granulomas within the gastric mucosa or submucosa.1 Common causes of GG include disseminated infections (such as tuberculosis, fungal infections), Crohn's disease, underlying malignancies or foreign bodies.2 When these conditions have been excluded, the diagnosis of idiopathic granulomatous gastritis (IGG) can be made. Nevertheless, most authors have been able to relate gastric granulomas to a particular etiology and the existence of the idiopathic form has been questioned.3
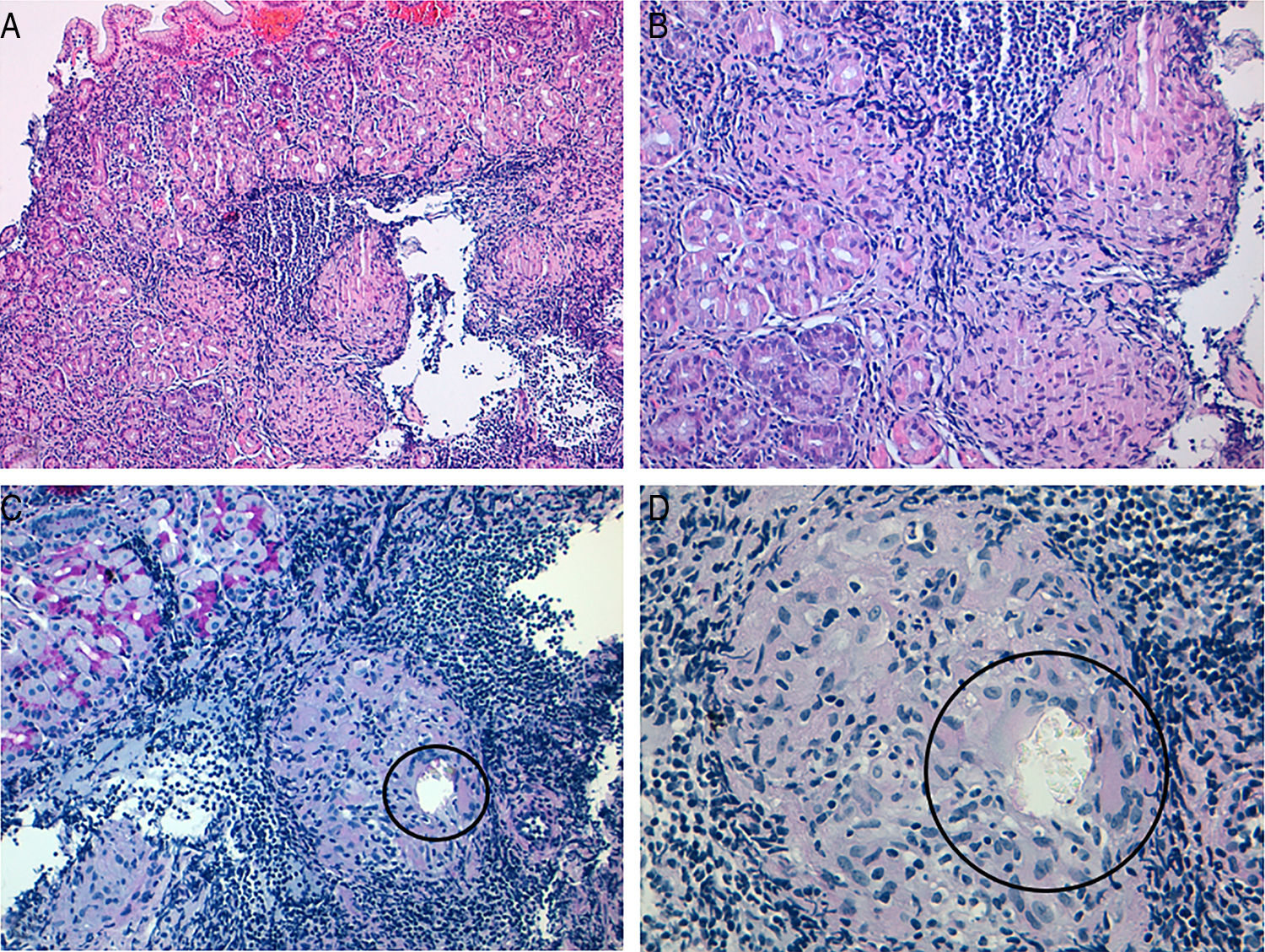
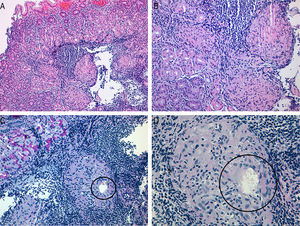
A 27-year-old woman was referred to the Gastroenterology outpatient clinic due to post-prandial vomiting for 10 months with associated weight loss (6kg). Her past medical history was irrelevant and her usual medication was omeprazole 20mg/day due to occasional symptoms of epigastric pain with years of evolution. An upper endoscopy did not reveal lesions, but multiple biopsies of the gastric mucosa were taken. Gastric biopsies revealed chronic inflammatory process with formation of lymphoid follicles and evidence of Helicobacter pylori infection. Additionally, multiple well-defined and non-necrotizing epithelioid granulomas with multinucleated giant cells were found (Fig. 1A and B). In one of the granulomas it was identified a birefringent material compatible with a foreign body (Fig. 1C and D). No acid-fast bacilli (Ziehl–Neelsen stain) or fungal microorganisms (PAS and PAS-D stains) were observed. No additional microbiological studies were performed. A diagnosis of GG, related to a probable foreign material was made.
After a careful clinical history, the patient reported the habit of biting and ingesting nails since childhood. She denied history of onychomycosis, use of nail polish or other nail beauty item lately. The patient had recently begun her work as a teacher and denied contact with chemicals products in her job or at home. Nevertheless, she underwent a colonoscopy and videocapsule endoscopy that excluded Crohn's disease. She was referred to the Infectious Diseases outpatient clinic and tuberculosis was excluded with chest X-ray, Mantoux test and QUANTIFERON®-TB Gold test.
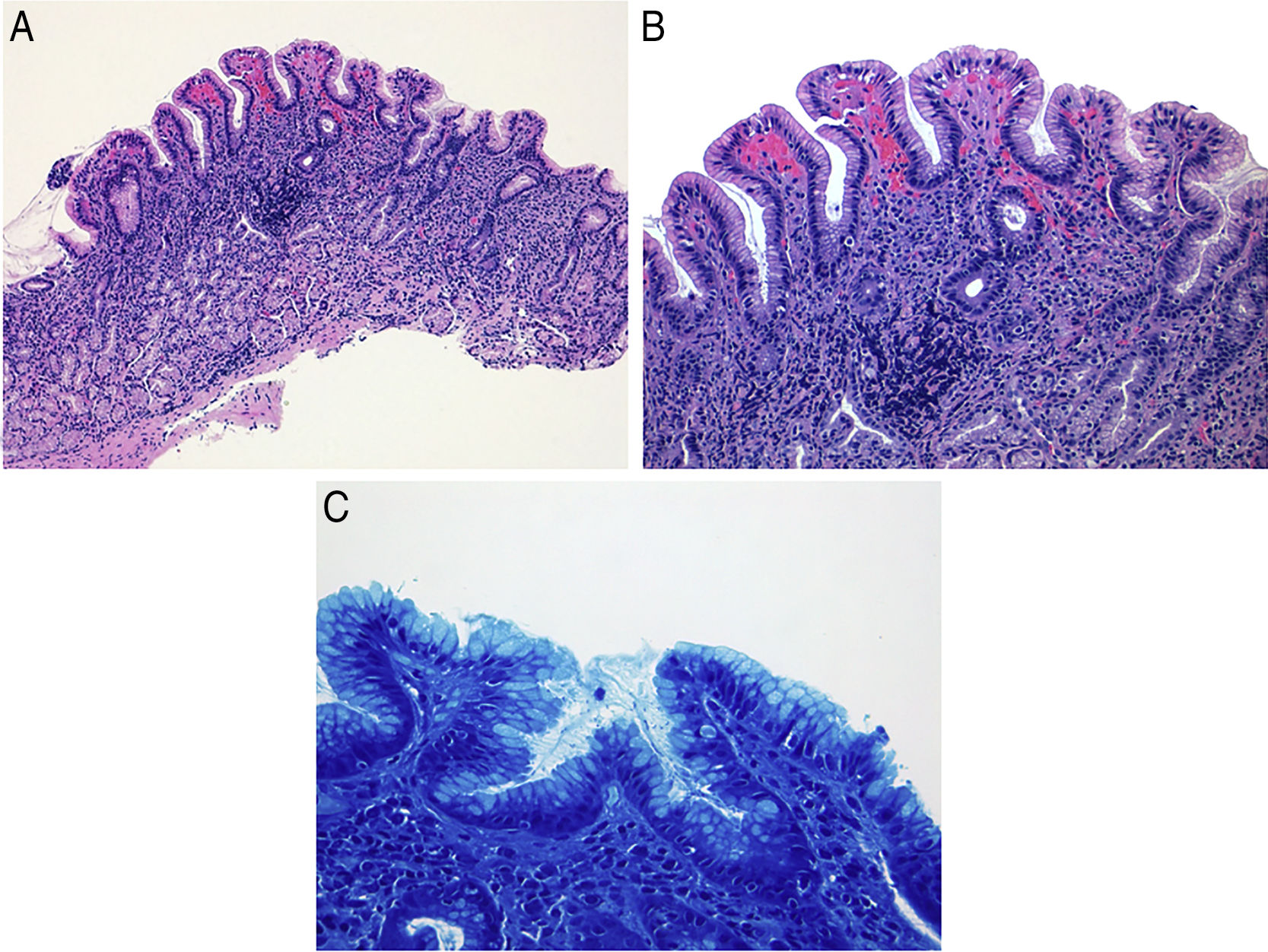
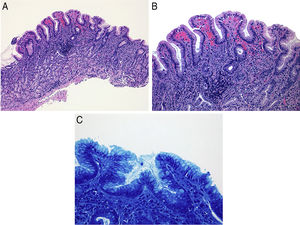
After six months of avoiding nail ingestion, the patient became asymptomatic. She underwent a subsequent upper endoscopy. Multiple gastric biopsies were undertaken and disclosed moderate chronic H. pylori gastritis but no granulomas or foreign material were seen, confirming resolution of GG (Fig. 2A–C).
Granulomatous gastritis is an uncommon pathological finding, with a reported incidence of 0.08–0.35% in the gastric biopsy samples.4,5 The most common cause of GG in the western countries is Crohn's disease accounting for approximately half of the cases.4,6 Other more rare causes include gastric tuberculosis, sarcoidosis, parasitic infections, foreign body reactions, Whipple's disease and adenocarcinoma.7 Miyamoto et al. also described a possible association with H. pylori infection with two reported cases of granulomatous gastritis resolution after successful eradication therapy for H. pylori.8 Nevertheless there is still controversy in relation to the role of H. pylori as a causative factor in GG, with larger studies unable to conclusively associate H. pylori infection with granuloma formation.4,9 In our case, since the patient presented with disabling symptoms and weight loss our priority was to exclude Crohn's disease and tuberculosis. The presence of foreign material in the biopsies, granulomatous gastritis and habit of nail ingestion suggested this association. Since the role of H. pylori in the development of GG is still controversial, we decided not to eradicate H. pylori and evaluate the clinical and histological response to suspension of nail ingestion. In our patient, it is likely that the symptoms of epigastric pain with years of evolution may be related to the habit of nails ingestion. The continuous exposure of the gastric mucosa to a foreign body material probably lead to the development of a granulomatous process with subsequent symptomatic aggravation. Given that the patient became asymptomatic and there was an evident histological improvement, we can conclude that nails ingestion (onychophagia) was the cause of GG in this case.
Conflicts of interestNo conflicts of interest to declare.