Cystic fibrosis is the most common life-shortening recessively inherited disorder in the Caucasian population. The genetic mutation that most frequently provokes cystic fibrosis (ΔF508) appeared at least 53,000 years ago. For many centuries, the disease was thought to be related to witchcraft and the “evil eye” and it was only in 1938 that Dorothy H. Andersen characterized this disorder and suspected its genetic origin. The present article reviews the pathological discoveries and diagnostic and therapeutic advances made in the last 75 years. The review ends with some considerations for the future.
La fibrosis quística es la enfermedad con herencia autosómica recesiva más frecuente en la población caucásica que produce una merma de la vida. La mutación genética que más frecuentemente la provoca (ΔF508) parece que hizo su aparición hace unos 53.000años. La enfermedad se relacionó durante siglos con la hechicería y el «mal de ojo», y no fue hasta 1938 en que Dorothy H. Andersen la describió como una entidad con personalidad propia y sospechó su origen genético. En este artículo se presenta una revisión de los descubrimientos fisiopatológicos y de los avances diagnósticos y terapéuticos que se han desarrollado a lo largo de estos tres cuartos de siglo. Finalmente, se plantean algunas consideraciones que deberán tenerse en cuenta en el futuro.
Despite the low incidence—one in 2000–4000 live births—within the pancreatic pathology group, and although prevalence varies depending on ethnic background and region of origin, cystic fibrosis (CF) is the most common autosomal recessive genetic disease in the Caucasian population. It is the result of mutations in the cystic fibrosis transmembrane regulator gene (CFTR), which causes abnormally viscous secretions in the cells of different epithelia. Mutations in this gene, consisting of 27 exons, are located on the long arm of chromosome 7. Frequency in healthy carriers is considered to be 1/30,1 giving some idea of the magnitude of the problem.
This multi-organ disease is classically characterized by a triad that includes lung impairment (chronic obstructive disease with bronchiectasis and repeated infections), pancreatic impairment (exocrine insufficiency) and abnormal sweat test results. It also has various other clinical manifestations, such as nasal polyps, azoospermia, chronic liver disease, cholelithiasis, diabetes mellitus and pancreatitis. Malnutrition and delayed growth are commonly observed in these patients. Up to 10–15% of neonates with CF have bowel obstruction at the level of the terminal ileum, a complication known as meconium ileus.
Although prognosis is difficult to establish, it has been improving over the years as its pathogenesis becomes better understood and different therapeutic advances—as will be discussed throughout this article—are applied. Thanks to these breakthroughs, patient survival improved from 14 to 20 years between 1968 and 1977. Nevertheless, a recent study has predicted that the average life expectancy in children born in 2010 and diagnosed with CF will be 37 years old for women and 40 years old for men, if the mortality rate observed during that year remains the same. However, it is speculated that survival could exceed 50 years if mortality continues to fall at an annual rate of 1.8%, as happened between 2000 and 2010.2 These data indicate the importance that this disease will acquire among the adult population in the coming years, especially if we take into account that a number of less serious clinical forms are not suspected in childhood but are later diagnosed in adulthood.
Despite these favourable expectations, CF remains a cause of major suffering for both patients and their families, as it frequently results in prolonged hospitalization, significantly shortens life spans and often leads to death in very young individuals.3
The evidenceAccording to the estimates of geneticist Xavier Estivill (1955; Barcelona, Spain), the antiquity of the most common mutation in CF (ΔF508) dates back some 53,000 years, while other less common mutations, such as G542X and N1303K, originated at least 35,000 years ago.4 Thus, determining the origins of this disease requires its historical background to be examined.
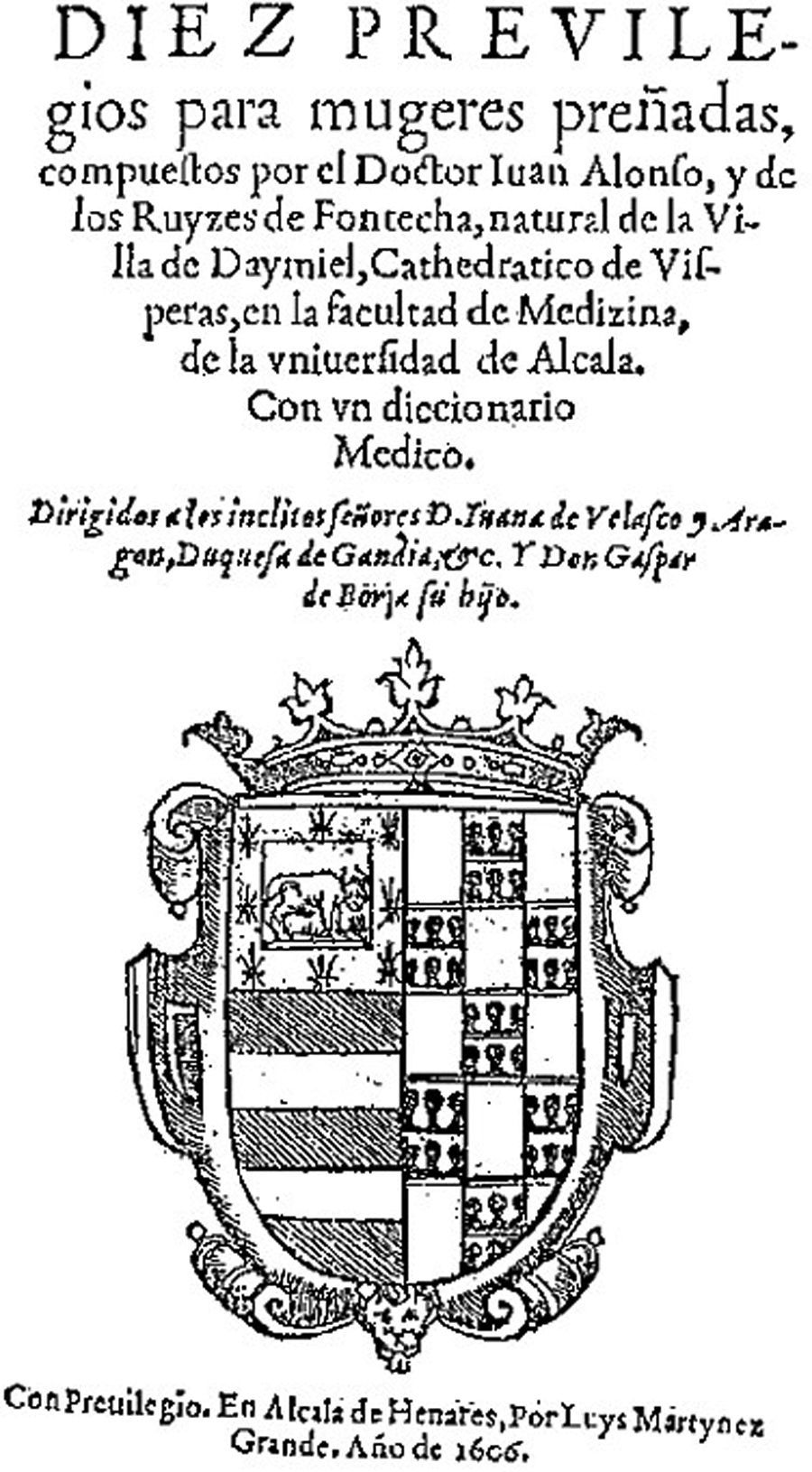
The first suspected reference to the disease is in an Irish proverb from the end of the fifteenth century, which says: “Woe to that child who tastes salty when kissed on the forehead. He is bewitched and soon must die”.5 Such children were considered to be afflicted with the “evil eye” and it was assumed that they would die prematurely. In 1606, a reference to the disease also appeared in the book Diez previlegios para mugeres preñadas, by Juan Alonso y de los Ruyzes de Fontecha (1560–1620; Daimiel, Spain), professor of medicine at the University of Alcalá de Henares (Madrid, Spain) (Fig. 1).6
The first pathological description was probably made in 1595, when Pieter Pauw (1564–1617; Amsterdam, the Netherlands), professor of botany and anatomy at Leiden University, performed an autopsy on a supposedly bewitched 11-year-old girl, who had presented malnutrition and hectic fever for 8 years. In her abdomen he found a swollen pancreas, scirrhous and bright white in colour, and therefore considered that the cause of death had been the pancreas. He also observed signs of pericarditis, which, we know today, appear in certain cases of CF.7 The second case was reported in 1673 by Georg Seger, who treated a 3-year-old girl in the city of Thorn (today Torun, Poland) for fever, vomiting and prolonged undernourishment. The autopsy was conducted by surgeon Bartholomaus Taubenheim, who described a hardened, cirrhotic pancreas. The third case came to light a few years later, in 1677, in a book entitled Observationes Medicae Rarioes, published by Gerardus Leonardus Blasius (1627–1682; Amsterdam, the Netherlands), professor of medicine in Amsterdam; he described the presence of a cirrhotic pancreas in an autopsy performed on a 9-year-old boy with delayed growth.7
Swiss anatomist and naturalist Nils Rosen von Rosenstein (1706–1773), considered the father of paediatrics, published his book De Morbis Infantum in 1752, in which he detailed 12 cases of children with diarrhoea, delayed growth, thinness, asthenia and swollen hands, feet and abdomen. Observing the presence of a hardened pancreas as a common denominator in the autopsy practised on all 12 children, he called this disease fluxus coeliacus.7
Years later, pathologist Carl von Rokitansky (1804–1878; Hradec Králové, Bohemia) described an autopsy that he carried out in 1838 on a 7-month-old foetus, in which he observed perforation of the small bowel and presence of meconium in the peritoneum. This is probably the first reported case of meconium ileus.8,9
In 1850, Viennese paediatrician Alois Bednar (1816–1888; Potterstein, Bohemia) described the case of a newborn girl who died 6 days after birth due to bowel obstruction. The autopsy showed that the small bowel was filled with thick-consistency meconium, while the large bowel was shrunken. This should also be interpreted as another case of meconium ileus.8,9
However, not all children with this condition died young. One example was the great composer and pianist of the Romantic era, Frederic Chopin (1810–1849; Zelazowa Wola, Poland), whose death was traditionally attributed to tuberculosis, a very common disease at the time in which he lived (Fig. 2). Some years ago, in 1998, Kubba and Young10 published an article in which, as well as reviewing the results of the autopsy, they revisited the artist's family history. Two sisters had died of chronic respiratory problems, one at 15 years old and the other at 47 years old. They also reviewed his personal symptoms (recurrent respiratory infections and chronic diarrhoea since childhood) and his very likely sterility. He lived with his lover George Sand for 10 years but she never became pregnant, even though she had already had three children. Furthermore, neither Sand nor her children contracted tuberculosis during the 10 years they lived with Chopin. An eminent pathologist called Jean Cruveilhier (1791–1874; Limoges, France) had performed the autopsy on the musician. Although Chopin's body was buried in Paris, his heart was removed, preserved in cognac and buried in his birth country, on the express wishes of the composer. Cruveilhier mentioned to Chopin's sister, Izabela, that what he had seen, even in the histological sections of the damaged lungs, did not allow him to make a diagnosis. This is understandable, since CF was an unidentified condition until the third decade of twentieth century. We can reasonably assume that the composer could have suffered from a less severe form of CF, although according Kuzemko, another possibility could be congenital α1-antitrypsin deficiency.11
Early descriptions and knowledgeIn 1905, pathologist and biologist Karl Landsteiner (1868–1943; Vienna, Austria)—winner of the 1930 Nobel prize for Medicine or Physiology for identifying the ABO blood groups using a chemical agglutination technique in blood in 1901—reported the existence of meconium ileus in a newborn with abnormal pancreatic secretion. In 1922, he emigrated to the USA to work in the Rockefeller Institute for Medical Research, where, in 1940, together with Alexander Salomon Wiener (1907–1976; New York, USA), he identified the Rhesus factor.5,12
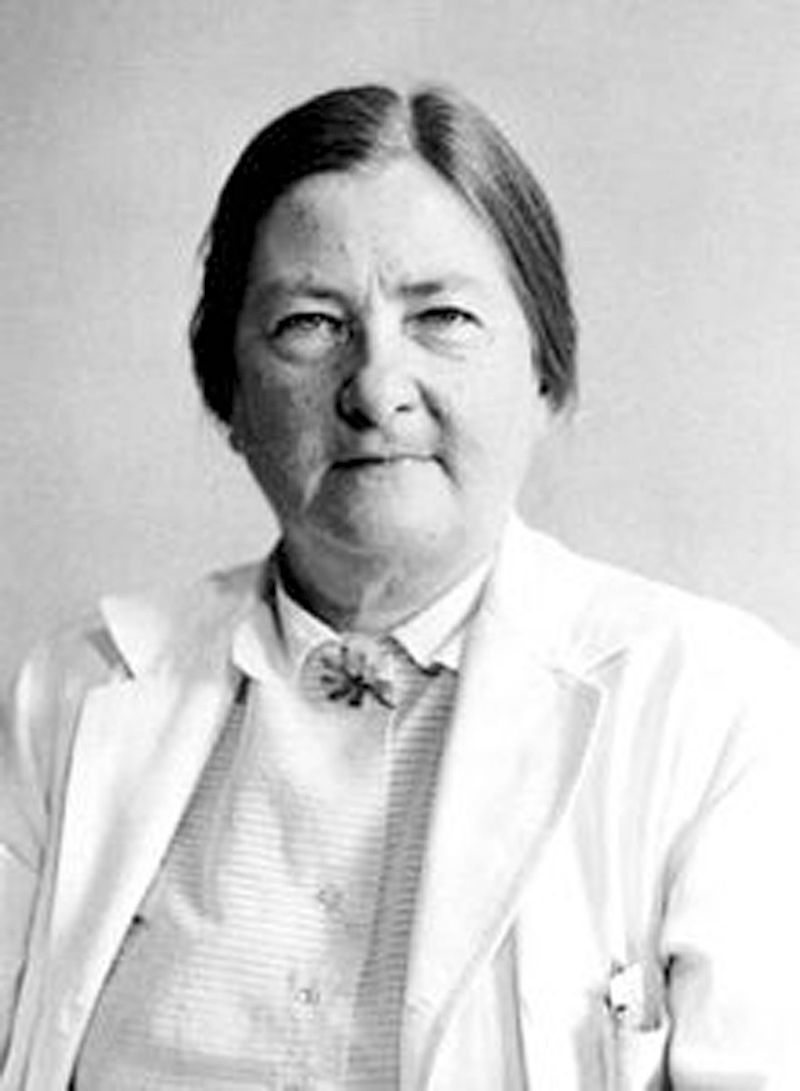
In an article published in 1936, paediatrician Guido Fanconi von Grebel (1892–1979; Pochiavo, Switzerland) used the term “cystic fibrosis” for the first time to describe the association of exocrine pancreatic insufficiency and chronic lung disease in children.13,14 However, his article did not have the impact that might have been expected given its importance, and it was not until 2 years later that pathologist Dorothy Hansine Andersen (1901–1963, North Carolina, USA) described the disease and the histological changes in the pancreas of children, naming it “cystic fibrosis of the pancreas” to distinguish it from other digestive diseases, but especially coeliac disease, which presented similar symptoms (diarrhoea, emaciation, etc.) (Fig. 3).15 That same year, Kenneth Blackfan (1883–1941; Cambridge, New York, USA), professor at Johns Hopkins hospital, described, together with Charles May (1908–1992; St. Louis, Missouri, USA), a microscopic study of the pancreases of 35 infants, reporting findings of dilatated ducts and acini, atrophy and fibrosis that they attributed to the presence of very viscous pancreatic secretions.16,17
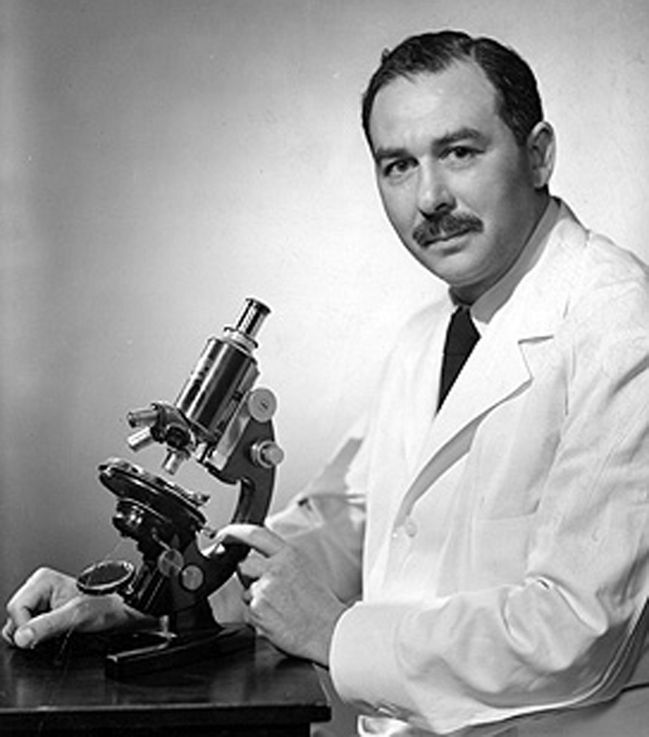
In 1945, paediatric pathologist and father of paediatric oncology Sydney Farber (1903–1973; Buffalo, New York, USA), coining the term “mucoviscidosis”, speculated that CF was not only a localized pancreatic problem but a generalized impairment in mucous production (Fig. 4).18 The following year, the aforementioned Dorothy H. Andersen conducted a series of studies on relatives of patients with CF, arriving at the conclusion that this was a genetic disease with autosomal recessive inheritance.19
DevelopmentsIn 1946, Dorothy H. Andersen and paediatrician Paul di Sant’Agnese (1914–2005; New York, USA) used penicillin (mainly in aerosol form) and sulphonamides to treat repeated respiratory infections, although without achieving the success they expected.20 Penicillin had been discovered accidentally in 1928 by Alexander Fleming (1881–1955; Lochfield, Scotland, UK), who won the Nobel prize for Medicine or Physiology in 1945. The prize was shared with biochemist Ernst Boris Chain (1906–1979; Berlin, Germany) and pharmacologist Howard Walter Florey (1898–1968; Adelaide, Australia), who developed the purification method that allowed chemical synthesis and subsequent commercialization of penicillin.21 The discovery of penicillin marked a fundamental change in modern medicine by launching the what came to be called the “antibiotic era”.
In another vein, the aforementioned Paul di Sant’Agnese became aware of a notable loss of salt in the sweat of patients with CF during a heatwave that swept New York in August 1948, and subsequently published a paper describing these sweat abnormalities.22 His technique for measuring salt loss was improved some years later by Gibson and Cooke,23 resulting in the sweat test still being considered today as essential for the diagnosis of CF.
In 1957, William Wallace, a professor of paediatrics at the Babies and Children's Hospital in Cleveland (USA), instructed young paediatrician LeRoy W. Matthews to set up a programme for preventive treatment of lung infections in children with CF and to assess impact on morbidity and survival.24,25 That same year, Irish physiotherapist Barbara Doyle, who was continuing her professional training at Boston Children's Hospital, commenced—at the suggestion of director Harry Shwachman (1910–1986; Boston, USA)—respiratory therapy using the so-called “English system”, which consisted of moving bronchial secretions by chest percussion and contralateral postural drainage.26 Harry Shwachman, himself a renowned paediatrician and authority on CF, described what came to be called Shwachman-Diamond syndrome, an autosomal recessive disorder that is the second most common cause of exocrine pancreatic insufficiency in children.27,28
An important breakthrough came in 1958, when Canadian Douglas N. Crozier, of Toronto Hospital for Sick Children, gave his patients a diet rich in saturated fats (completely contrary to what had been done up until then) and high doses of oral pancreatic enzyme supplements, thereby managing to improve nutritional status and growth and lengthen survival.29 The publication of these results in 1974 led to a complete overhaul of the dietary criteria applied until then and to the addition of nutritional supplements in the diet. An important role was also played by pancreatic enzyme supplement preparations in the form of microspheres with an acid-resistant capsule; these enabled the nutritional status of patients to be improved using a much smaller dose, since the enteric coated microspheres were not inactivated on passing through the stomach.30 The large number of capsules that children with CF have to take is known to be a major treatment complication, so this significant reduction in quantity greatly improved patients’ quality of life. Although studies of pancreatic enzyme therapy commenced in 1872 under Wilhelm Oliver von Leube (1842–1922; Ulm, Germany), then rector of the University of Würzburg, it was not until 1900 that this kind of therapy was demonstrated to reduce excess faecal fat and nitrogen loss. The year 1900 was also when the first commercial preparation (Pankreon) appeared, obtained from bovine and porcine pancreatic extracts.31
In 1981, Michael Knowles, a respiratory medicine specialist at the University of North Carolina, demonstrated the presence of an abnormally increased potential difference across the nasal mucosa that resulted in an abnormal epithelial function.32 This led Paul Quinton (b. 1944), professor at the University of California in San Diego, who had himself been diagnosed with CF at the age of 19 years, to study the problem of the sweat ducts. He demonstrated that impermeability to chloride meant that this could not be reabsorbed into the blood, thereby causing sweat to remain on the skin surface. This finding, applied to other epithelia, would explain the viscosity of mucus in these patients.33
Major advances in terms of genetic knowledge of CF were made in the 1980s. In 1985, the CFTR gene was mapped; 4 years later, Francis Sellers Collins (1950; Virginia, USA), Lap-Chee Tsui (1950; Shanghai, China) and John Richard Riordan (1943; New Brunswick, Canada) discovered the first and most common mutation of this chromosome, which they called ΔF508. The possibilities of diagnosis have now been enhanced by the more than 1800 mutations linked to this disease.1,34,35
Neonatal screening programmes also began to be implemented in the 1980s, as the result of an article published by New Zealander Jeannette Crossley (b. 1949), who used a simple dried blood spot to detect (by immunoanalysis) high concentrations of trypsin in patients with CF.36,37 The development of these programmes has made it possible to initiate proper treatment in early stages of the disease, with better child development achieved by early prevention of respiratory infections and improvements to nutritional status.38
In this same decade, treatment programmes based on the use of nebulized or intravenous antibiotics were also implemented to prevent and eradicate respiratory infections caused by Pseudomonas aeruginosa.39–41
However, the most spectacular breakthrough took place in 1985, when Magdi Yacoub (b. 1935; Egypt) in London and John Wallwork in Cambridge performed heart-lung transplants in patients at very advanced disease stages, achieving a 72% of 2-year survival rate.42,43 Successful outcomes were also obtained for liver transplant in patients with CF and severe liver disease.44 That same year, ursodeoxycholic acid therapy at doses of 10–15mg/kg/day was tested in cases of less severe liver disease, reporting improvements in liver function at 2–6 months, although to a lesser degree than observed in adults with chronic liver disease due to other causes.45
In 1990, Michael J. Welsh's team from the University of Iowa was the first to correct the defective chloride channels of the epithelial cells in CF and to demonstrate a causal relationship between mutations in the CFTR and defective chloride ion transport.46 In 1993, Hyde et al.47 from the University of Oxford managed to correct conductivity defects in the trachea of transgenic mice using liposomes for gene transfer. This opened the door to the possibility of gene therapy in humans with CF. Michael Welsh's team made the first attempt at this type of treatment via the mucosa of the nasal passage and using adenovirus as a vector, thereby making further progress in improving long-term lung function using gene therapy.48
Again in the 1990s, treatments that improved the expulsion of mucus and corrected respiratory infections in patients were introduced. Recombinant human DNase was shown to be an excellent mucolytic that decreased the viscosity of sputum.49 Inhaled tobramycin and oral azithromycin treatments were also shown to be useful for patients with chronic Pseudomonas infection.50,51
The 1990s also saw the introduction, in Germany and the English-speaking world, of commercial pancreatic enzyme preparations with high doses of lipase (25,000IU per capsule), which enabled steatorrhoea to be reduced using fewer capsules with an overall higher dose of lipase; although some cases of stenosis at the level of the colon were reported,52 these were soon attributed to a component in the capsule coating. No further reports in this regard have appeared since capsule modification. Pancreatic enzyme preparations also became available in Spain, but more than a decade later.
Since the start of the new millennium, research groups have been very active, persisting in efforts—initiated in the 1990s—to test animal models and satisfactorily implement gene therapy. Pigs and ferrets that have been bred with alterations in both CFTR alleles are proving especially useful for studying the pathogenesis of the disease and testing treatments, as they have defective chloride ion transport mechanisms that mimic the clinical manifestations of humans with CF.53,54
Several CFTR modulators have been tested in recent years. In 2011, two phase-3 studies were completed, one with Ataluren (PTC 124) and the other with Lumacaftor, both of which improved respiratory function in patients. The latter has ostensibly been useful in patients with two copies of ΔF508.55,56 In January 2012, the American Food and Drug Administration (FDA) approved use of Kalydeco, also known as Ivacaftor, the first oral medicinal product available for patients aged over 6 years old with the G178R, S549N, S549R, G551S, G551D, G1244E, S1251N, S1255P, G1349D and R117H mutations.55
In another vein, respiratory exacerbations in children aged over 6 years old have been reduced with the use of inhaled hypertonic saline solutions to improve hydration of the airway surface and mucociliary clearance.55,57
The futureThe prediction that children born in 2010 and diagnosed with CF could survive to 50 years old2 suggests that the problems associated with CF are not limited to paediatrics but—as already observed due to the existence of milder cases that are diagnosed late—will affect adult specialities such as respiratory medicine, gastroenterology and even sterility, family planning and genetic counselling. We therefore should consider improving cross- and multidisciplinary patient care units in the coming years. Registries of patients with CF need to be upgraded and screening programmes, launched in the USA (Colorado), UK, Australia and New Zealand in the 1980s, need to be expanded. In Spain, neonatal screening programmes were set up in 1999 in Catalonia and Castilla-León and have been gradually rolled out in other Spanish regions.58
Although there is no consensus on neonatal screening strategies, determination of immunoreactive trypsin for a blood spot obtained 3–5 days after birth and dried on absorbent paper would appear to be the most widely approved approach. Tests should be repeated at 3–5 weeks if initial results indicate values greater than 65ng/mL. If the second test is positive, a sweat test should be performed and, if also positive, a genetic study.58
With respect to treatments, those based on drugs administered in the form of nebulizers need to be improved and protocols need to be developed to prevent cross-infection, bearing in mind the emergence of new microorganisms and allergies and resistance to existing antibiotics.
The expansion of lung transplant programmes is also advisable, while bearing in mind possible difficulties in obtaining sufficient donor organs.
It is also to be hoped that all the expectations that have been placed in gene therapy will be fulfilled, as this offers the only way forward to a possible solution for CF. Nevertheless, we should not lose sight of the fact that this disease generates very significant healthcare costs, so funding could become its biggest problem.
Conflict of interestsThe author declares that he has no conflict of interests.
Please cite this article as: Navarro S. Recopilación histórica de la fibrosis quística. Gastroenterol Hepatol. 2016;39:36–42.