Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection generally presents with respiratory symptoms. However, in a recent meta-analysis of 35 studies, Mao et al. reported that 10–21% of patients with respiratory Coronavirus disease 2019 (COVID-19) had gastrointestinal manifestations. The most frequent gastrointestinal symptomatology was diarrhea (9%) and SARS-CoV-2 RNA was detected in stool in 54% of cases.1 In the reported studies radiologic and endoscopic examinations, when performed, were normal.
By contrast, other studies had found endoscopic and radiological changes. Thus, Carvalho et al. reported a patient admitted for hemorrhagic colitis attributed to COVID-19 due to a negative etiologic study and the development of respiratory symptoms, being diagnosed of SARS-CoV-2 by nasopharyngeal swab.2 Tullie et al. reported eight cases of isolated ileal involvement detected by abdominal ultrasound or CT scan attributed to COVID-19 in children diagnosed by a positive nasopharyngeal swab test, in these patients, neither ileal biopsies nor stool detection was not performed.3 No similar cases have been reported in adults.
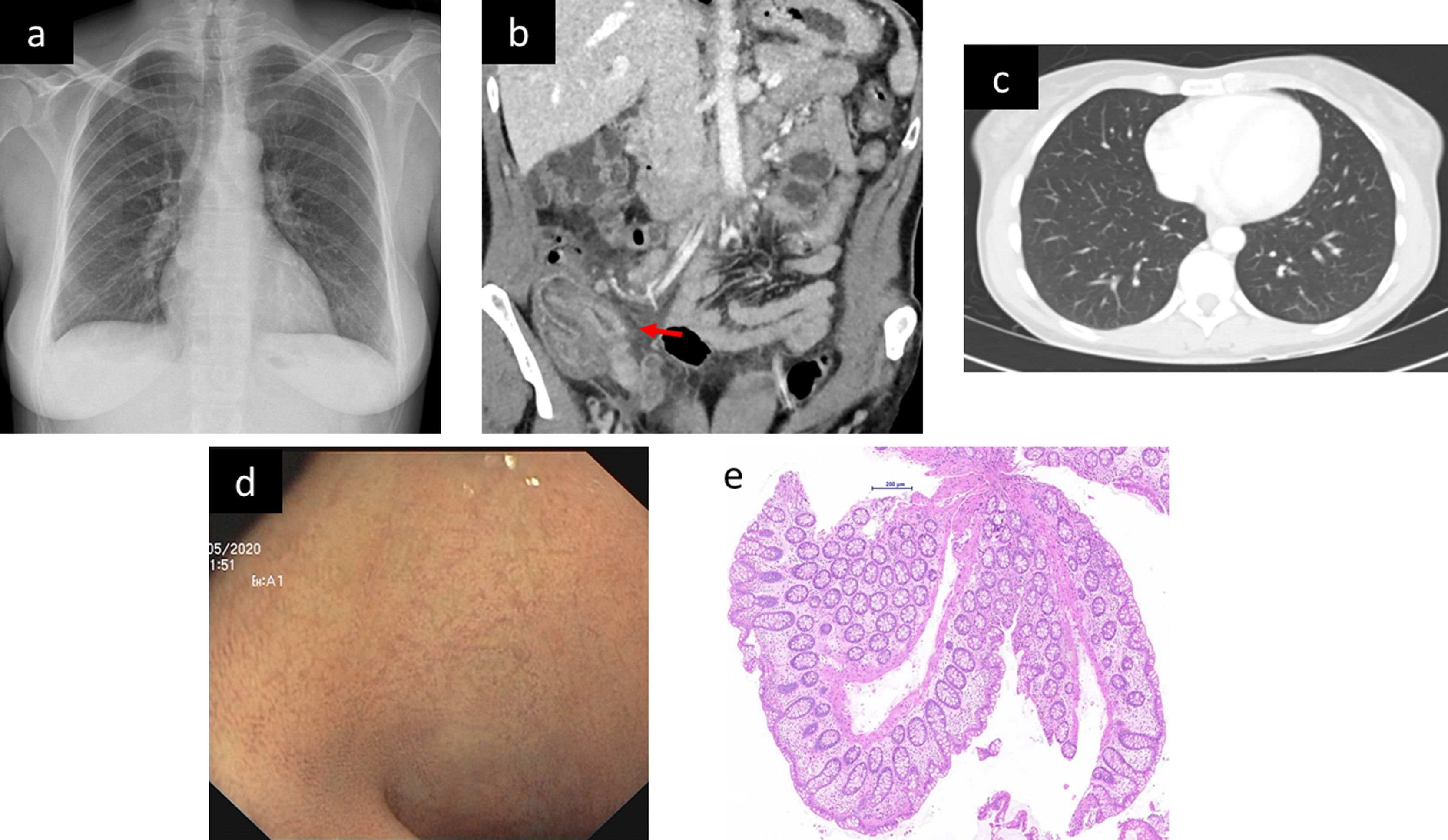
We present the case of a 47-year-old female worker of an elderly nursing home with no previous significant medical history was admitted to the emergency room. She reported 10 days of right lower quadrant abdominal pain, high fever (maximum 39.5°C) and non-bloody diarrhea. The patient did not report any respiratory symptoms. No other family members were affected. Two nasopharyngeal and oropharyngeal swab specimens performed before admission had been negative for SARS-CoV-2. Respiratory auscultation was strictly normal, and pain was noted on the palpation of the right lower abdominal quadrant. Blood test showed markedly increased inflammatory parameters (leukocytes, D-Dimer, ferritin C-reactive protein). Chest X-ray was normal (Fig. 1a). Abdominal CT scan showed inflammatory signs in the distal ileum (Fig. 1b). The pulmonary images of the abdominal CT scan were normal (Fig. 1c).
Empiric treatment with ceftriaxone, metronidazole and azithromycin was started. The patient was admitted to the gastroenterology unit after a confirmatory negative SARS-CoV-2 NAAT (nucleic acid amplification test) (GeneFinder™ COVID-19 Plus RealAmp Kit, Osang Healthcare Korea) by amplification of RdRp, E and N genes in a nasopharyngeal swab.
The study was completed with an enzyme immunoassay which revealed negative Yersinia spp and Campylobacter spp antibodies. A rectal swab was performed and NAAT was positive for SARS-CoV-2. A fourth nasopharyngeal swab resulted negative.
Ileocolonoscopy was performed eleven days after because of the pandemic situation and the recommendation by our infectiology department of avoid the colonic preparation to prevent the possible risk of fecal SARS-CoV-2 elimination and the contagious to the medical team (currently this fact is not proved). No mucosal changes were found in the ileocolonic mucosa (Fig. 1d). Biopsies were taken and histology study showed no significant changes (Fig. 1e). NAAT of SARS-CoV-2, intestinal bacteria, viruses and parasites (Gastrointestinal panel Filmarray®, Biomerieux France) were performed being positive for SARS-CoV-2 and negative for Salmonella spp., Shigella spp., Yersinia enterocolitica, Aeromonas spp., Vibrio spp., Plesiomonas shigelloides, Clostridioides difficile, Campylobacter spp., Cryptosporidium spp., Entamoeba histolytica, Giardia intestinalis, Cyclospora cayetanensis, norovirus, astrovirus, sapovirus, adenovirus and rotavirus. At that time, serology was performed and both SARS-CoV-2 IgM+IgA and IgG antibodies were positive (Vircell SL®, Spain).
The patient recovered completely, with normalization of the previous blood test abnormalities. A SARS-CoV-2 control NAAT in rectal swab was negative before discharge from hospital. The patient remains asymptomatic after three-month follow-up.
To our knowledge, our report is the first well-documented case of SARS-CoV-2 intestinal infection without evidence of pulmonary involvement. The multiple negative nasopharyngeal swabs plus the normal chest X-ray and CT findings rule out pulmonary infection. Intestinal involvement was suspiced by the finding of an ileitis in the CT scan. Ileal mucosa was normal, showing a mismatch between radiology and endoscopy. However SARS-CoV-2 confirmed by two independent rectal and intestinal NAAT. The diagnosis of ileitis due to SARS-CoV-2 was made by the exclusion of other potential causes. In this context, it seems probable that the patient became infected by fecal-oral transmission.
No other studies detected the SARS-COV-2 in intestinal samples. However, during the SARS-CoV-1 epidemic in 2003 studies in patients with gastrointestinal manifestations detected the virus in intestinal cells by molecular methods.4 In our case, no immunohistochemical or FISH study was performed because commercial tests were not yet available.
We report a patient with SARS-CoV-2 infection apparently limited to the bowel. However, no recommendations or conclusions can be drawn from this case report. The patient had an important delay between the admission and the colonoscopy and, despite we found a radiological ileitis, endoscopic mucosa was normal.
In conclusion, SARS-CoV-2 may occur with an exclusive intestinal symptoms. Is important for clinicians to know and recognize this clinical presentation, a rectal swab may be necessary to establish the diagnosis.
Authors’ contributionEduard Brunet and Albert Villoria managed the patient during hospitalization and wrote the manuscript. Antonio Casabella and Sonia Calzado critically reviewed the text and provided important intellectual content. All authors definitively approved the submitted version.
Conflict of interestAlbert Villoria has served as a speaker and consultant from MSD, Abbvie, Jansen and Falk. Eduard Brunet, Antonio Casabella, and Sonia Calzado, have not conflicts of interest.
We thank Xavier Calvet, Luigi Melcarne, Pilar Garcia-Iglesias, Laura-Patricia Llovet, Mateu Espasa, Àlex Casalots, Eva Van den Eynde and Manuel Cervantes for their help with the management of the patient and for his critically review of the manuscript. We also thank Michael Maudsley for his help with the English.
The patient has given his informed consent to publish the information included in the article.