The current coronavirus (COVID-19) pandemic has limited access to medical care, drugs and endoscopic procedures, which could affect treatment adherence by patients with inflammatory bowel disease (IBD), with the subsequent risk of relapse, deterioration in quality of life, higher financial cost in health care and an increased risk of disability and complications.1 Furthermore, this pandemic has raised questions about the use of immunomodulators, biologic therapy and small molecules, with regard to patients and medical teams. Although different societies have recommended maintaining these therapies during the pandemic,2,3 little is known about treatment adherence in patients with IBD.
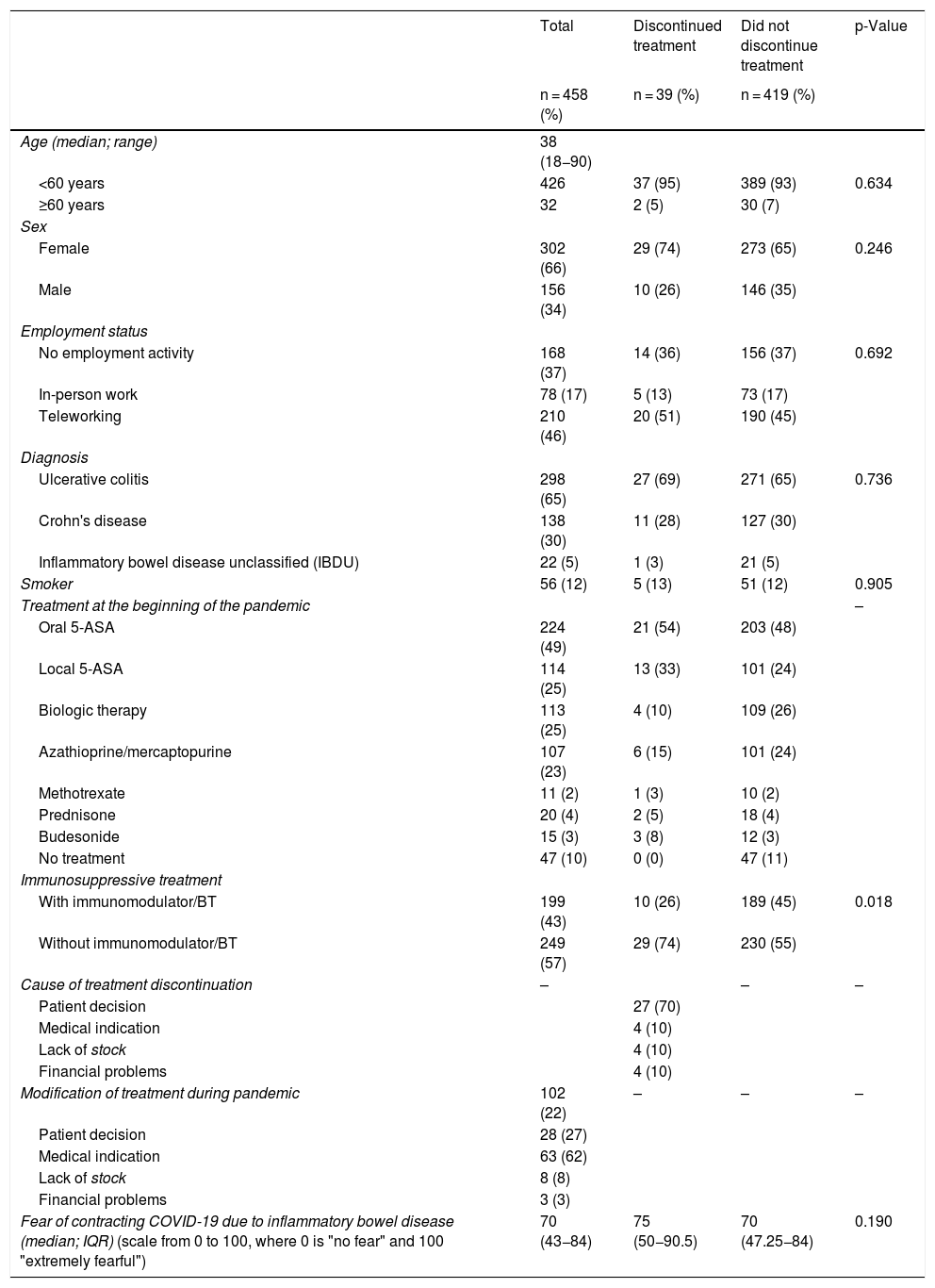
To answer this question, we conducted a descriptive, cross-sectional study between 24 August and 10 September 2020 in patients on follow-up on the IBD Programme of the Clínica Las Condes [Las Condes Clinic] (n = 1432). A survey was sent out by e-mail (REDCap®) to find out about the treatment for IBD and adherence, causes of treatment discontinuation or modification and the fear of contracting COVID-19. Demographic and clinical data were obtained from the IBD registry and the statistical analysis was performed using frequency, medians and the Mann-Whitney test (p < 0.05). A total of 458 (32%) patients responded to the survey during the study period; 66% were women, 65% had ulcerative colitis (Table 1). The drugs most often used at the beginning of the pandemic were oral and/or topical salicylates (30%) and immunomodulators and/or biologics (27%). 9% of the patients discontinued treatment, mainly at the patient's own decision (70%), and 22% modified the treatment (62% for medical indication in the context of IBD management, either due to flare-up or modification of treatment on reaching clinical remission). In the univariate analysis, patients on immunomodulator/biologic therapy abandoned treatment less frequently (p = 0.018). Treatment adherence was not related to other variables such as age, gender, type of IBD, comorbidities or employment status. 70% of the patients reported fear of contracting COVID-19 due to IBD. Women reported a significantly greater fear of developing the infection (women 73 [IQR 50–90] vs. men 57 [IQR 30–78.7]; p = 0.0008). On the other hand, although patients with other comorbidities reported a significantly greater fear of developing COVID-19 (comorbidity 72.5 [IQR 50–90] vs. no comorbidity 69 [IQR 40.5–80]), this was not reflected in a greater rate of discontinuation of therapy. Immunomodulator/biologic therapy treatment was not related to an increased fear of developing COVID-19.
Demographic and clinical characteristics of patients with inflammatory bowel disease in relation to discontinuation of treatment during the COVID-19 pandemic.
| Total | Discontinued treatment | Did not discontinue treatment | p-Value | |
|---|---|---|---|---|
| n = 458 (%) | n = 39 (%) | n = 419 (%) | ||
| Age (median; range) | 38 (18−90) | |||
| <60 years | 426 | 37 (95) | 389 (93) | 0.634 |
| ≥60 years | 32 | 2 (5) | 30 (7) | |
| Sex | ||||
| Female | 302 (66) | 29 (74) | 273 (65) | 0.246 |
| Male | 156 (34) | 10 (26) | 146 (35) | |
| Employment status | ||||
| No employment activity | 168 (37) | 14 (36) | 156 (37) | 0.692 |
| In-person work | 78 (17) | 5 (13) | 73 (17) | |
| Teleworking | 210 (46) | 20 (51) | 190 (45) | |
| Diagnosis | ||||
| Ulcerative colitis | 298 (65) | 27 (69) | 271 (65) | 0.736 |
| Crohn's disease | 138 (30) | 11 (28) | 127 (30) | |
| Inflammatory bowel disease unclassified (IBDU) | 22 (5) | 1 (3) | 21 (5) | |
| Smoker | 56 (12) | 5 (13) | 51 (12) | 0.905 |
| Treatment at the beginning of the pandemic | – | |||
| Oral 5-ASA | 224 (49) | 21 (54) | 203 (48) | |
| Local 5-ASA | 114 (25) | 13 (33) | 101 (24) | |
| Biologic therapy | 113 (25) | 4 (10) | 109 (26) | |
| Azathioprine/mercaptopurine | 107 (23) | 6 (15) | 101 (24) | |
| Methotrexate | 11 (2) | 1 (3) | 10 (2) | |
| Prednisone | 20 (4) | 2 (5) | 18 (4) | |
| Budesonide | 15 (3) | 3 (8) | 12 (3) | |
| No treatment | 47 (10) | 0 (0) | 47 (11) | |
| Immunosuppressive treatment | ||||
| With immunomodulator/BT | 199 (43) | 10 (26) | 189 (45) | 0.018 |
| Without immunomodulator/BT | 249 (57) | 29 (74) | 230 (55) | |
| Cause of treatment discontinuation | – | – | – | |
| Patient decision | 27 (70) | |||
| Medical indication | 4 (10) | |||
| Lack of stock | 4 (10) | |||
| Financial problems | 4 (10) | |||
| Modification of treatment during pandemic | 102 (22) | – | – | – |
| Patient decision | 28 (27) | |||
| Medical indication | 63 (62) | |||
| Lack of stock | 8 (8) | |||
| Financial problems | 3 (3) | |||
| Fear of contracting COVID-19 due to inflammatory bowel disease (median; IQR) (scale from 0 to 100, where 0 is "no fear" and 100 "extremely fearful") | 70 (43−84) | 75 (50−90.5) | 70 (47.25−84) | 0.190 |
BT: biologic therapy; IBD: inflammatory bowel disease; IQR: interquartile range; 5-ASA: 5-aminosalicylates.
The negative impact of the COVID-19 pandemic on stress and anxiety can affect the clinical outcomes of patients with chronic conditions, as is the case of IBD, whose development and evolution are linked to these factors. As in other studies,4 a significant percentage of patients feared developing COVID-19. Despite this, and in line with other studies,4,5 our results demonstrate that a high percentage of patients have continued to adhere to their treatment during this pandemic period, which could be attributed in part to ready access by patients to their medical team (nurse specialised in IBD or treating gastroenterologist) by e-mail, phone or telemedicine. This has allowed recommendations to be made not only for the prevention of SARS-CoV-2 infection, but also on the need to maintain treatment, thus reducing the possibility of flare-ups, use of corticosteroids or hospitalisations.2,3
It is these communication mechanisms between the medical team and the patient that could explain why, in our results, patients on immunomodulator/biologic therapy, regarded as a more severe group, presented greater treatment adherence than those treated with mesalazine. Additionally, factors such as advanced age and the presence of comorbidities, such as diabetes, hypertension and other cardiovascular diseases, have been associated with an unfavourable evolution in patients with IBD and COVID-19. Although our results show that patients with a comorbidity reported a significantly greater fear of developing COVID-19, this was not reflected in lower treatment adherence, confirming that communication between the medical team and the patient is essential during the pandemic.
In this study, whether or not the patient had an IBD flare-up during the pandemic was not included in the variables, which is a limitation since it was not possible to establish an association with lack of treatment adherence.
In conclusion, the results of this survey allow us to adequately estimate the global impact of COVID-19 on treatment adherence in patients with IBD. Education about the relationship between IBD, drugs and COVID-19 is undoubtedly crucial in allaying fears and in maintaining adequate treatment adherence. Clear educational strategies must be established to reduce the possibility of unnecessary morbidity and mortality through a lack of treatment adherence.
Please cite this article as: Quera R, Simian D, Flores L, Ibáñez P, Figueroa C. Impacto de la pandemia covid-19 en la adherencia al tratamiento en pacientes con enfermedad inflamatoria intestinal: experiencia de un centro terciario en Chile. Gastroenterol Hepatol. 2021;44:654–656.