Dyspepsia is a common disorder in both primary (PC) and specialised care (SC). Gastroscopy is recommended at the start of the study if there are warning signs, although it is not always available in PC.
Objectives and methodsWe developed a pilot project establishing an early gastroscopy programme for patients with dyspepsia and warning signs in PC, subsequently extending it to the entire healthcare area. The aim was to evaluate the requirements, impact and opinion of this service at the PC level. Demographic, symptomatic and endoscopic variables on the patients referred to SC from the pilot centre were recorded. A satisfaction survey was conducted among the PC physicians.
ResultsThe one-year pilot study and the first year of implementation of the programme were evaluated. A total of 355 patients were included (median age 56.4 years; IQR 45.5–64.3); 61.2% (56.1–66.3%) were women. The waiting time for examination was 1.5 weeks (IQR 1.5–2.5). Gastroscopy was correctly indicated in 82.7% (78.4–86.3%) of patients. The median number of requests per month was 1.1 per 10,000 adults (range 0.8–1.6). Monthly referrals to SC clinics from the pilot centre fell by 11 subjects (95% CI 5.9–16) with respect to the previous median of 58 (IQR 48–64.5). Almost all those polled (98.4%) considered the programme useful in routine practice.
ConclusionsThe availability of an early gastroscopy programme in PC for patients with dyspepsia and warning signs reduced the number of referrals to SC.
La dispepsia es un trastorno frecuente tanto en Atención Primaria (AP) como Especializada (AE). Se recomienda realizar una gastroscopia al inicio del estudio si existen datos de alarma, aunque su accesibilidad desde AP es variable.
Objetivos y métodosDesarrollamos un proyecto piloto estableciendo una agenda de gastroscopia precoz para pacientes con dispepsia y datos de alarma en AP, ampliándolo posteriormente a toda el área sanitaria. El objetivo fue evaluar los requerimientos, el impacto y la valoración desde AP de esta prestación. Recogimos variables demográficas, sintomáticas y endoscópicas de los pacientes remitidos y las derivaciones a AE desde el centro piloto. Se realizó una encuesta de satisfacción entre los facultativos de AP.
ResultadosSe evaluaron el proyecto piloto, de un año de duración, y el primer año de implantación de la agenda, con un total de 355 pacientes (edad mediana 56,4 años; RIQ 45,5-64,3). El 61,2% (56,1-66,3%) eran mujeres. La demora hasta la exploración fue de 1,5 semanas (RIQ 1,5-2,5). El 82,7% (78,4-86,3%) de las gastroscopias fueron indicadas correctamente. La mediana mensual de solicitudes fue de 1,1 por cada 10.000 adultos (rango 0,8-1,6). Las derivaciones mensuales a consultas de AE desde el centro piloto disminuyeron en 11 sujetos (IC 95% 5,9-16), respecto a la mediana previa de 58 (RIQ 48-64,5). El 98,4% de los encuestados consideraron la agenda útil en su práctica habitual.
ConclusionesLa disponibilidad de una agenda de gastroscopia precoz en AP para pacientes con dispepsia y datos de alarma disminuye el número de derivaciones a AE.
Affecting up to 38% of the population, dyspepsia is one of the most common digestive conditions.1 Its estimated prevalence in Spain is 23.9%, and individuals have a 39% chance of experiencing it at some point in their lifetime.2
Although not everyone who experiences dyspepsia seeks medical care, approximately 25% will do so at some stage.3,4 These figures represent a significant burden on the healthcare system. In primary care (PC), between 2.1% and 8.3% of all consultations are dyspepsia-related,5,6 and this proportion has remained unchanged over recent years.7 Furthermore, it is estimated that 13–24% of patients are referred to Secondary Care (SC),8,9 which also generates a significant healthcare burden at this level.
The joint clinical practice guidelines issued by the Asociación Española de Gastroenterología [Spanish Association of Gastroenterology] and the Sociedad Española de Medicina de Familia y Comunitaria [Spanish Society of Family and Community Medicine]10 recommend a test and treat strategy in the initial management of the condition, reserving gastroscopy for patients refractory to symptomatic treatment and for patients who present any of the following warning signs: over the age of 55 years, dysphagia, anaemia, weight loss, frequent vomiting or a physical examination with pathological findings. One of the problems with this strategy is the lack of access to early gastroscopy in PC,11 which may lead some physicians to refer these patients directly to SC to avoid delaying the diagnosis of a potentially serious disease.
To confront this problem, we believe that a specific schedule in PC for patients with dyspepsia and warning signs would lead to more effective management of these situations.
Material and methodsWe developed an analytical, prospective and observational study to implement the early gastroscopy schedule (less than one month between requesting the gastroscopy and carrying it out) for patients with dyspepsia and warning signs in PC. The project was approved by the centre's Independent Ethics Committee in 2013.
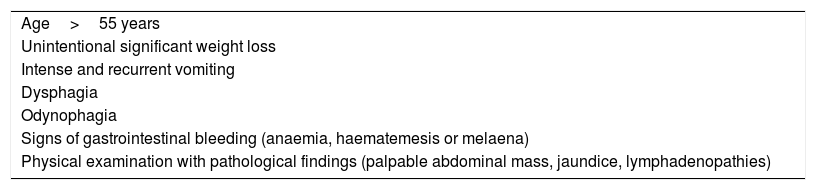
Implementation of the early gastroscopy scheduleThe pilot project was launched in June 2013 in a single health centre (HC). The referral criteria were adjusted to meet the established recommendations,10 that is, at least one warning sign or older than 55 years of age (Table 1). The schedule was defined following numerous meetings with PC and SC physicians to establish the indications and referral criteria. After 6 months, two further HCs joined the pilot project, and one year after the project was started, it was decided to implement the early gastroscopy schedule for dyspepsia with warning signs at the eight HCs affiliated with the hospital, with a catchment population of approximately 260,000 people (215,000 over the age of 15 years). A dedicated leaflet was created for this purpose that set forth the established referral criteria.
Preferential gastroscopy indication criteria.
| Age>55 years |
| Unintentional significant weight loss |
| Intense and recurrent vomiting |
| Dysphagia |
| Odynophagia |
| Signs of gastrointestinal bleeding (anaemia, haematemesis or melaena) |
| Physical examination with pathological findings (palpable abdominal mass, jaundice, lymphadenopathies) |
The study population included all patients referred from the various HCs to undergo a gastroscopy as part of the specific schedule. The exclusion criteria were as follows: failure to perform the gastroscopy or completion of a partial gastroscopy only; the performance of a prior gastroscopy since symptom onset; and a prior diagnosis of gastric cancer, oesophageal cancer or Barrett's oesophagus.
Study objectivesThe primary endpoint of the study was to assess the requirements for the implementation and operation of the early gastroscopy schedule for patients with dyspepsia and warning signs, as well as its impact on referrals from PC to the Gastroenterology Department.
The secondary endpoints were to describe the response of primary care physicians to the early gastroscopy schedule and to ascertain the determining factors that led to patient referral to SC.
Data collectionThe demographic and epidemiological data were collected together with the informed consent during an interview at the hospital's Endoscopy Unit before the examination and without prior assessment of the gastroscopy requests. The endoscopic variables were taken after the gastroscopy had been conducted. The histological variables and the request issued by PC for a Gastroenterology assessment were collected at least two months after the gastroscopy. A satisfaction survey was issued to the primary care physicians at least six months after implementation of the schedule. The survey was completed during a series of training sessions on colon cancer screening given by gastroenterologists in the various HCs. They were handed out to attendees at the beginning of the session and collected at the end. The data concerning referrals from PC to Gastroenterology were sent by the hospital's administration departments. The following were defined as significant findings: histologically confirmed malignant neoplasms, ulcers and severe oesophagitis (grades C and D according to the Los Angeles Classification).12 The examinations were deemed to be correctly indicated if the patient presented at least one warning sign.
Statistical analysisThe statistical analysis was performed with the program STATA (StataCorp 2013, Stata Statistical Software Release 13, StataCorp LP, College Station, TX, United States). The categorical variables are reported as percentages with 95% confidence intervals. The continuous variables with a normal distribution are presented as mean and standard deviation, while those with a non-normal distribution are shown with their median, interquartile range (IQR) and/or range. All the tests conducted were two-tailed. A p-value of 0.05 was established as the threshold for statistical significance. To assess the outcomes of the referrals from PC, referred patients from the pilot HCs were paired with the same months of the two previous years. The number of examinations requested per adult was calculated based on the population treated at each HC at the start of the schedule implementation period. The request rate of each HC was indirectly standardised by age using the values of the entire catchment area as reference. The satisfaction survey for primary care physicians comprised both open and closed questions as well as an overall valuation based on the Likert scale (Annex I). Logistic regression was used to evaluate the factors associated with referrals from PC.
Results355 patients were enrolled between the implementation of the pilot project and July 2015. Two (0.6%) were excluded from the final analysis as they failed to complete the examination due to intolerance.
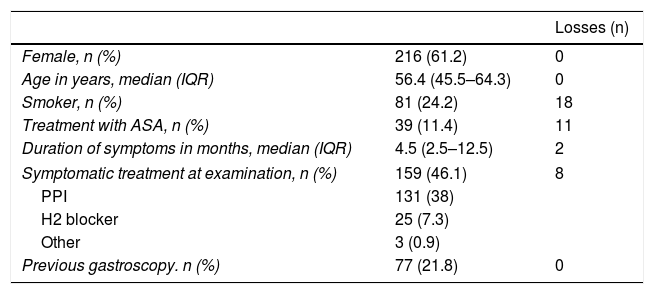
Sample descriptionThe median age was 56.4 years (IQR 45.5–64.3; range 14.7–92.3). 61.2% were female. Table 2 shows the baseline characteristics of the patients enrolled. The most common symptom was epigastric pain (72.4%), followed by pyrosis (45.9%), abdominal distension (38%) and early satiety (30%). Time from the request to the examination was 1.5 weeks (IQR 1.5–2.5; range 0.5–4.5). Among the patients who had already undergone a prior gastroscopy, the time elapsed since the last examination was 4.2 years (IQR 2.9–6.4; range 1.9–12).
Characteristics of enrolled patients.
| Losses (n) | ||
|---|---|---|
| Female, n (%) | 216 (61.2) | 0 |
| Age in years, median (IQR) | 56.4 (45.5–64.3) | 0 |
| Smoker, n (%) | 81 (24.2) | 18 |
| Treatment with ASA, n (%) | 39 (11.4) | 11 |
| Duration of symptoms in months, median (IQR) | 4.5 (2.5–12.5) | 2 |
| Symptomatic treatment at examination, n (%) | 159 (46.1) | 8 |
| PPI | 131 (38) | |
| H2 blocker | 25 (7.3) | |
| Other | 3 (0.9) | |
| Previous gastroscopy. n (%) | 77 (21.8) | 0 |
ASA: acetylsalicylic acid; H2 blocker: H2 receptor antagonist; IQR: interquartile range; PPI: proton-pump inhibitor.
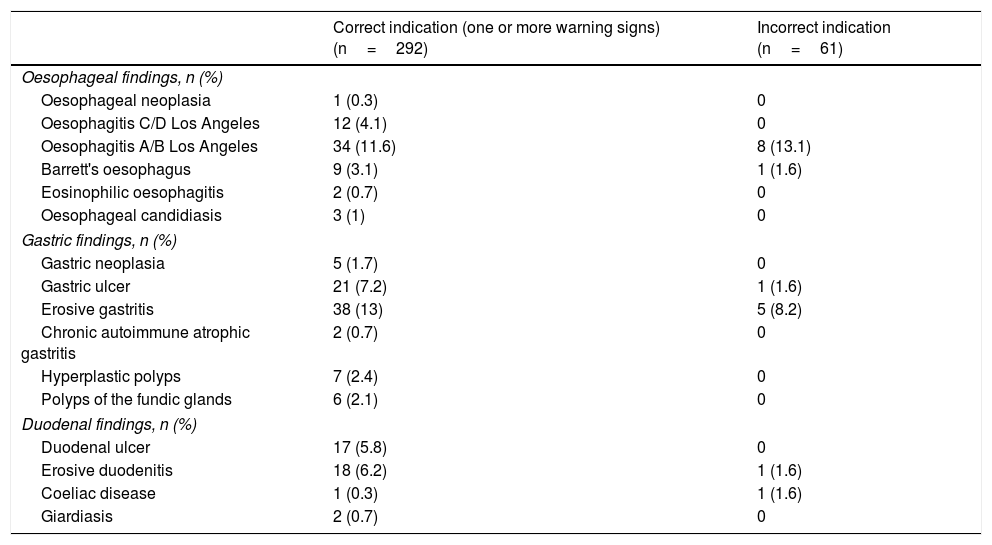
Significant findings were identified in 15.6% of patients (12.2–19.7%); 11% (8.2–14.7%) had ulcers, 3.4% (1.9–5.9%) severe oesophagitis and 1.7% (0.8–3.7%) had malignancies. The malignancies included four gastric adenocarcinomas (two stage IV and two stage IIIa), one stage IIa) oesophageal squamous cell carcinoma and one stage II diffuse large cell lymphoma. Other endoscopic findings of noteworthy prevalence were mild oesophagitis in 11.9% of patients (8.9–15.7%), erosive gastritis in 12.2% (9.1–16%) and erosive duodenitis in 5.4% (3.5–8.3%). Although much less common, other relevant findings included: oesophageal candidiasis in 0.8% of patients (0.3–2.5%), coeliac disease in 0.6% (0.2–2%) and eosinophilic oesophagitis in 0.6% (0.2–2%). The endoscopic findings in relation to warning signs are summarised in Table 3.
Endoscopic findings.
| Correct indication (one or more warning signs) (n=292) | Incorrect indication (n=61) | |
|---|---|---|
| Oesophageal findings, n (%) | ||
| Oesophageal neoplasia | 1 (0.3) | 0 |
| Oesophagitis C/D Los Angeles | 12 (4.1) | 0 |
| Oesophagitis A/B Los Angeles | 34 (11.6) | 8 (13.1) |
| Barrett's oesophagus | 9 (3.1) | 1 (1.6) |
| Eosinophilic oesophagitis | 2 (0.7) | 0 |
| Oesophageal candidiasis | 3 (1) | 0 |
| Gastric findings, n (%) | ||
| Gastric neoplasia | 5 (1.7) | 0 |
| Gastric ulcer | 21 (7.2) | 1 (1.6) |
| Erosive gastritis | 38 (13) | 5 (8.2) |
| Chronic autoimmune atrophic gastritis | 2 (0.7) | 0 |
| Hyperplastic polyps | 7 (2.4) | 0 |
| Polyps of the fundic glands | 6 (2.1) | 0 |
| Duodenal findings, n (%) | ||
| Duodenal ulcer | 17 (5.8) | 0 |
| Erosive duodenitis | 18 (6.2) | 1 (1.6) |
| Coeliac disease | 1 (0.3) | 1 (1.6) |
| Giardiasis | 2 (0.7) | 0 |
Malignancies were found at other sites (adenocarcinoma of the colon stages IIa and IIIc, stage IV adenocarcinoma of the pancreas and stage IV renal adenocarcinoma, multiple myeloma and disseminated cancer of unknown origin) within two months of the gastroscopy in 1.7% of cases (0.8–3.7%).
Suitability of the indicationThe 353 gastroscopies were requested by 128 different physicians from eight HCs. Overall, 82.7% (78.4–86.3%) were correctly indicated. Age (>55 years) was the most common warning sign, representing 56.4% (51–51.6%) of all cases; of those, 94.5% (90.2–96.9%) were >55 years of age at symptom onset. Weight loss was recorded in 26.5% (22–31.4%) of patients, anaemia in 20.2% (16.1–24.8%), dysphagia in 14.8% (11.3–19%) and frequent vomiting in 11.7% (5.3–11%). Macroscopic gastrointestinal bleeding and physical examination with pathological findings represented fewer than 10% and 1% of cases, respectively. Once the schedule had been implemented, 46 inappropriate indications were made, 36 of which involved an overestimation of symptoms (in the interview, patients reported weight loss of 0–2kg, infrequent vomiting, etc.).
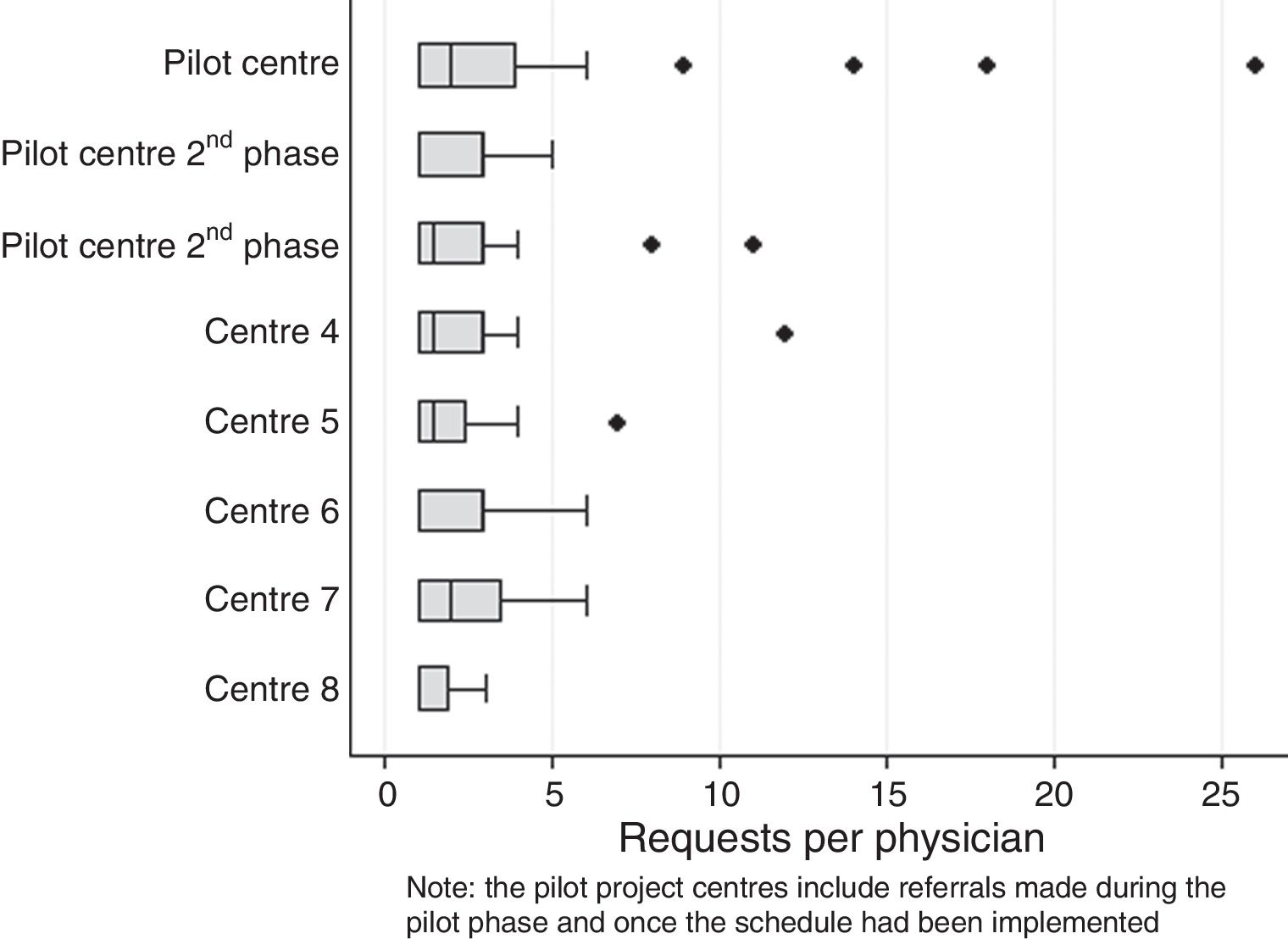
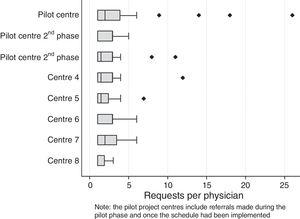
Analysing each participating HC individually, the rate of appropriate indications ranged from 66.7% to 96.2%. The indications issued by the HCs that participated in the pilot project tended to be more appropriate than those issued by the other HCs (88.5% vs 73.3%; 15.2% difference [6.6–23.8%]), p<0.001. No differences were found in the rate of appropriate indications amongst the HCs that participated in the pilot project during this first phase (86.1%; 79.6–92.6%) compared to the indications issued after the implementation of the schedule (90.1%; 85.5–96.3%), p=0.27. Having analysed the requests issued by individual physicians using box plots (Fig. 1), the number of requests issued by the physicians of each HC can be seen to be broadly consistent. Of the 128 individual requests issued, only 8 physicians (6.3%) were identified who issued a sufficiently high number of requests to represent an outlier on the box plot. The indications issued by these physicians were more often correct than those issued by their colleagues (94.1% vs 79.1%), p=0.001.
Request rateOnce the schedule had been implemented, the median number of monthly requests was 25 patients (IQR 22–31; minimum 17; maximum 35), meaning a total of 1.1 applications per month per 10,000 adults (IQR 1–1.4; range 0.8–1.6). By evaluating each individual HC, notable differences were found, with 1.8 requests per month per 10,000 adults from the centre that issued the most requests, and 0.7 from the least active centre. Standardising these rates by age slightly reduced these differences, ranging between 1.6 and 0.6. No correlation was found between the number of requests and the suitability of the indications issued by each centre, p=0.76.
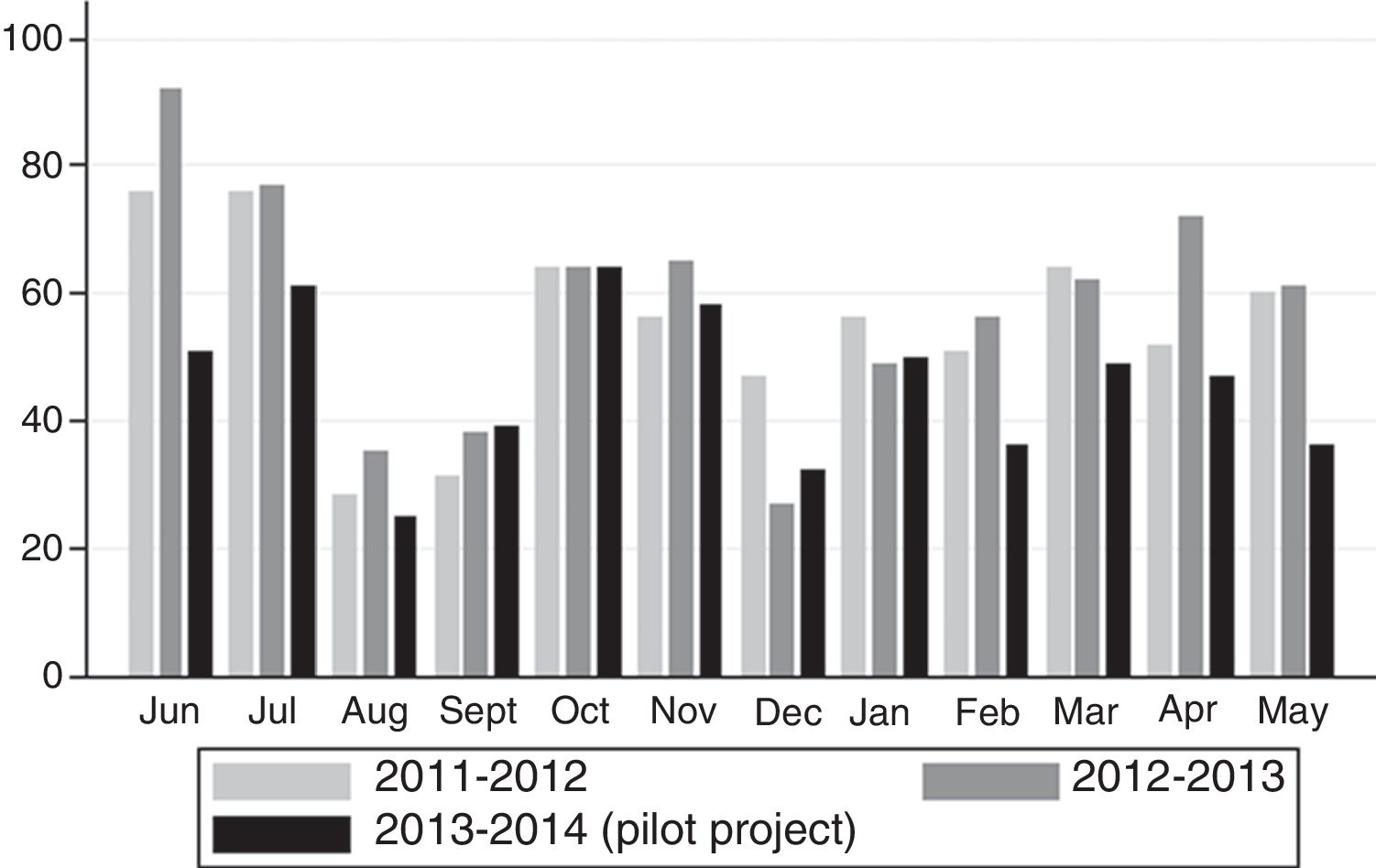
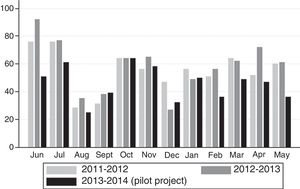
Effect on referrals from primary care to Gastroenterology consultationAt the start of the project, the pilot HC covered a catchment area of 43,000 subjects (37,000 over the age of 15 years). As Fig. 2 shows, in the two years prior to the pilot project, 58 patients (median) were referred from the pilot HC every month (IQR 48–65; range 27–92). During the pilot project, the monthly median was 48 patients (IQR 36–55; range 25–64), representing a decrease in the monthly number of referrals of 11 subjects,5,9–16p<0.001.
18.1% of subjects (14.5–22.5%) were referred to Gastroenterology consultation (from PC or from the same endoscopy unit). None of the variables collected prior to the endoscopy (age, gender, symptom duration, type of symptoms, warning signs, treatment with ASA, treatment with NSAIDs, previous gastroscopy) was significantly associated with referrals to SC. As such, a multivariate analysis was not performed. Concerning the endoscopic findings, all oesophagogastric malignancies identified were referred to SC from the Endoscopy Unit. With the exception of coeliac disease (the 2 cases identified were referred), all the other endoscopic findings were not significantly associated with referrals to SC.
Valuation of the primary care physiciansThe satisfaction survey was completed by 61 physicians from six different HCs. The median number of participants per centre was 10 (range 6–15). 68.9% of respondents had used the schedule at least once. Of the 19 physicians who had never used the schedule, the most common reason given by 13 physicians was not having assessed any patients who met the criteria, while three claimed not to be aware of the schedule and a further three were not familiar with the referral criteria. In total, 9.8% (4.6–19.8%) of respondents did not use the schedule as they were not aware of its implementation. 98.4% (91.3–99.7%) considered the schedule to be useful in their routine clinical practice and 100% intended to use it in the future.
DiscussionIt is particularly important to optimise dyspepsia management given its high prevalence. Several strategies to achieve this have been proposed. Open-access endoscopy units are well established and almost universally used. They reduce costs by reducing the number of SC consultations, which is offset by a variable rate of inappropriate indications (5–49%).13 Consultation/Investigation/Diagnosis is another option but is much less widespread. This is defined as outpatient healthcare by which a diagnosis is established and appropriate treatment administered in a single day.14 These consultations shorten study times but may lead to an increased number of examinations and higher diagnostic costs.15 Furthermore, gastroenterology departments are not in a position to implement this type of consultation in the same way as other specialties given that many diagnostic procedures require preparation or sedation, or the results are not immediately forthcoming (viral serology, coeliac testing, etc.). As such, the patient is obliged to attend a subsequent visit.16
Prioritising patients with warning signs would be a feasible change for open-access units to adopt. The rate of appropriate indications in our study exceeded 80% with no abuse of the system found. The earlier conduct of these examinations does not affect the waiting list as it merely involves its reorganisation. It must be acknowledged that there is some debate concerning the appropriateness of prioritising patients according to warning signs. However, there is current consensus for its appropriateness despite its low positive predictive value, which ranges from 0% to 11%,17 and the fact that 11–15% of patients with dyspepsia present at least one warning sign.18,19 Nevertheless, even with these figures, the manifestation of warning signs are associated with referrals to SC with odds ratios ranging from 1.5 to 2.8.9
In our study, the difference in the request rate between the different centres is of interest. However, a British study involving more than 6000 primary care centres across the country found that the request rate of the more active centres was 2.5 times higher than the request rate of the least active centres.20 This finding is even more noteworthy given the lack of differences in terms of appropriate referrals between the centres, regardless of the number of requests. As such, these request rate disparities are probably due to varying degrees of compliance with the referral criteria. Finally, 10% of the physicians surveyed had not used the schedule due to ignorance of its implementation or its usage criteria. In centres with high staff turnover, the success of innovative measures may depend on appropriate promotion and communication, with frequent reminders being key.
This study does have several limitations. Firstly, the impact on referrals to SC could only be assessed in the HC of the pilot project. Between the end of 2014 and the end of 2015, other strategies were gradually introduced to reduce the number of referrals from PC (open-access colonoscopy schedule in PC, updating the gastroesophageal reflux disease protocols, modifying the hepatic profile in PC and implementing and promoting an email for discussing consultations between PC and SC). This partially overlapped with the first year of the gastroscopy schedule for patients with dyspepsia and warning signs in the other seven HCs. Referrals did not increase in any of the seven HCs: no significant differences were found in two, while five saw a reduction in the number of referrals of between 10% and 40% compared to the two previous years. Although these data support the correlation between the implementation of the schedule and the fall in the number of referrals, the confounding factors prevent an objective assessment. Secondly, it is difficult to know whether the fall in the number of referrals is due to the availability of the schedule or collaboration with PC to implement it. Although not possible to quantify, we consider this interaction to be particularly important, as shown by the appropriateness of indications issued by the HCs of the pilot project referred to above. The proportion of correct indications issued at the pilot centres remained unchanged in the following phase, showing that the disparities are not the result of a learning curve. What is more, the collaboration between primary care and secondary care did not affect the number of referrals in another study conducted in Spain involving the development of joint protocols and the implementation of an open-access gastroscopy schedule.15 Thirdly, the survey may overestimate the acceptance of the schedule in PC. As the survey was voluntary, there may be selection bias. Finally, level of education and socioeconomic status were not taken into account when standardising the monthly requests per 10,000 population, which have been shown to influence whether people seek medical care.
Despite these limitations, our results show that the implementation of an early gastroscopy schedule for PC is simple and efficient, as it merely requires reorganisation of gastroscopy requests and schedules, which could reduce the number of subsequent referrals to SC. Our study also provides sufficient data to forecast the examinations to offer in order to implement a schedule of this type in different treatment areas. 1.4 monthly examinations per 10,000 adults would cover the needs of 75% of the participating HCs. Finally, its positive valuation by PC could be the first step towards improving collaboration between the different echelons of healthcare.
Conflicts of interestThe authors declare that they have no conflicts of interest.
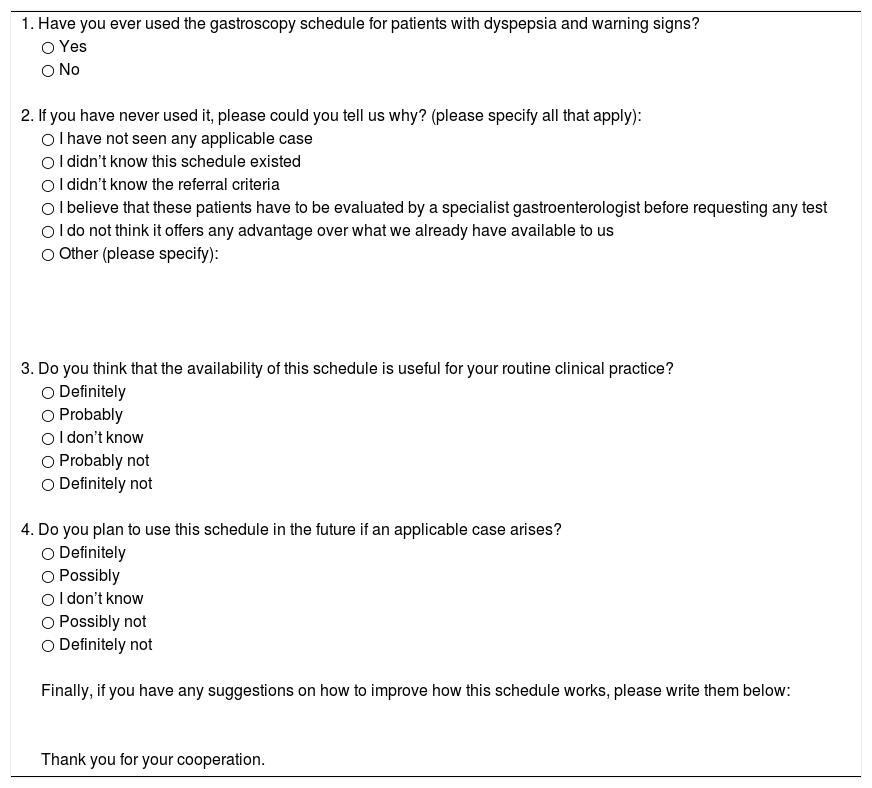
Dear colleague:
In recent months, a high-resolution gastroscopy schedule for patients with dyspepsia with warning signs has been made available to physicians at your health centre. In order to evaluate its true usefulness, it would be very useful for us to know your opinion.
We would greatly appreciate it if you would complete the following survey. The information you provide is anonymous and will help us to improve this service.
| 1. Have you ever used the gastroscopy schedule for patients with dyspepsia and warning signs? |
| ○ Yes |
| ○ No |
| 2. If you have never used it, please could you tell us why? (please specify all that apply): |
| ○ I have not seen any applicable case |
| ○ I didn’t know this schedule existed |
| ○ I didn’t know the referral criteria |
| ○ I believe that these patients have to be evaluated by a specialist gastroenterologist before requesting any test |
| ○ I do not think it offers any advantage over what we already have available to us |
| ○ Other (please specify): |
| 3. Do you think that the availability of this schedule is useful for your routine clinical practice? |
| ○ Definitely |
| ○ Probably |
| ○ I don’t know |
| ○ Probably not |
| ○ Definitely not |
| 4. Do you plan to use this schedule in the future if an applicable case arises? |
| ○ Definitely |
| ○ Possibly |
| ○ I don’t know |
| ○ Possibly not |
| ○ Definitely not |
| Finally, if you have any suggestions on how to improve how this schedule works, please write them below: |
| Thank you for your cooperation. |
Please cite this article as: García-Alonso FJ, Hernández Tejero M, Rubio Benito E, Valer P, Guerra I, García Ceballos VG, et al. Implantación y evaluación de una prestación de gastroscopia precoz para pacientes con dispepsia y datos de alarma en Atención Primaria. Gastroenterol Hepatol. 2017;40:331–338.