Foreign body impaction is a frequent indication of urgent endoscopy. One of the reasons for impaction is eosinophilic oesophagitis (EE). To analyze characteristics of oesophageal foreign body impactions and their relationship with eosinophilic oesophagitis.
MethodsIn this retrospective study, urgent endoscopies in a tertiary care centre were analyzed. We included all urgent endoscopies due to bolus and foreign body impactions performed between September 1st 2018 and September 1st 2020. We reviewed clinical data of all patients who were diagnosed with EE and compared it to impactions that were due to other motives. The mean follow-up time was 18.7 months.
Results693 urgent endoscopy procedures were performed. 239 (34%) of these were due to foreign body ingestion. Mean age of the patients was 63 years old and 135 (63%) were men. EE was diagnosed in 36 (17%) patients. The factors associated with EE were age, to be younger than 50 years (OR, 7.3; 95% CI, 1.1–48.4; p=0.04), asthma/rhinitis/atopic dermatitis (OR, 8.9; 95% CI, 2.3–35.3; p=0.002), findings in the endoscopy as trachealization (OR, 9.7; 95% CI, 1.3–70.9; p=0.03) and psychotropic/calcium channel blocker drugs (OR, 0.09; 95% CI, 0.009–0.9; p=0.04). 15 (7%) patients died. In 6 of them death was impaction-related. None patients with EE died.
ConclusionsForeign body impaction in the upper gastrointestinal tract due to EE is a frequent cause of urgent endoscopy. Being under 50 years of age, having asthma/rhinitis/atopic dermatitis, trachealization on the oesophagus and not taking psychotropic/calcium channel blocker drugs are factors associated with the diagnosis of EE. Mortality in the follow-up of patients without EE is important.
La impactación por cuerpos extraños es una indicación frecuente de endoscopia urgente. Una de las causas de impactación es la esofagitis eosinofílica. Nuestro objetivo es analizar las características de las impactaciones por cuerpos extraños en el esófago y su relación con la esofagitis eosinofílica.
MétodosEn este estudio retrospectivo, se analizan todas las endoscopias urgentes realizadas por impactación de alimentos y cuerpos extraños en un hospital terciario entre el 1 de septiembre de 2018 y el 1 de septiembre de 2020. Se analizan las características clínicas de los pacientes diagnosticados de esofagitis eosinofílica y se comparan con las impactaciones debidas a otros motivos. El seguimiento medio fue de 18,7 meses.
ResultadosSe realizaron 693 procedimientos de endoscopia urgentes; de ellos, 239 (34%) fueron por impactación por cuerpos extraños. La edad media fue de 63 años y 135 (63%) eran hombres; 36 (17%) de todos los pacientes con impactación fueron diagnosticados de esofagitis eosinofílica. Los factores asociados a ella fueron la edad, ser menor de 50 años (OR 7,3; IC 95%: 1,1-48,4; p=0,04), el antecedente de asma y/o rinitis y/o dermatitis atópica (OR 8,9; IC 95%: 2,3-35,3; p=0,002), los hallazgos endoscópicos como traquealización (OR 9,7; IC 95%: 1,3-70,9; p=0,03) y el consumo de fármacos psicotrópicos o antagonistas del calcio (OR 0,09; IC 95%: 0,009-0,9; p=0,04). Fallecieron 15 (7%) pacientes, todos sin esofagitis eosinofílica y en 6 el fallecimiento se relacionó con las impactaciones.
ConclusionesLa impactación por cuerpos extraños en el tubo digestivo por esofagitis eosinofílica es una entidad frecuente en los servicios de endoscopia de urgencia. Tener menos de 50 años, asma, rinitis, dermatitis atópica, traquealización del esófago y no consumir fármacos psicotrópicos o antagonistas del calcio son factores asociados al diagnóstico de esofagitis eosinofílica. La mortalidad en el seguimiento de los pacientes sin esofagitis eosinofílica es importante.
Emergency endoscopy is an established technique in gastrointestinal practice.1 The most common clinical indications are acute gastrointestinal bleeding and foreign body ingestion.1,2
The aetiologies of foreign body ingestion are numerous and include problems with chewing ability, accidental ingestion, suicidal ingestion, oesophageal obstruction due to carcinoma or benign causes, diverticulum and impairment of oesophageal motility.3 In recent years, the incidence of eosinophilic oesophagitis (EE) has increased and it has been recognized as a cause of oesophageal impaction.4
EE is characterized by eosinophil-predominant inflammation of the oesophagus. It is a rare condition but the incidence and prevalence of EE is currently increasing in developed countries.4 Clinical manifestations are diverse and vary depending on the age of patients. Acute food bolus impaction is the most common and it may result in urgent endoscopy. Other clinical presentations are asthma, allergic rhinitis, food sensitivity and atopic dermatitis.5
The diagnosis of EE is based on the finding of 15 or more eosinophils/high-power field (HPF, at magnification ×40) in mucosal biopsies taken during upper gastrointestinal endoscopy. Endoscopic findings include rings and white plaques but there may also be no macroscopic changes.5 Therefore, diagnosis cannot be achieved with endoscopic visualization alone. Performing additional endoscopies may be necessary for follow-up purposes and for assessing response to treatment.
Our objective was to determine the incidence, outcomes and risk factors associated to oesophageal foreign body impactions, as well as the relationship they have with EE.
Material and methodsThis retrospective observational study reviewed all urgent endoscopies performed at Donostia-San Sebastián University Hospital (HUD) from September 1st 2018 to September 1st 2020. We studied all cases involving foreign body and bolus impaction and their clinical data. All patients had a follow-up period of at least 6 months after the inclusion period.
We included all urgent endoscopies due to foreign body impaction in patients who were 14 years old or older.
We excluded endoscopies performed with the radiology service, all lower gastrointestinal endoscopies, upper endoscopies performed due to other motives and endoscopies of which we were not able to identify the clinical indication.
In all patients who were included, medical records were reviewed to determine each patient's age, sex, personal history, previous and/or subsequent endoscopies, treatment received, endoscopic findings and whether biopsies were taken during the procedure. If a patient underwent more than one endoscopy in this period only one of them was considered for the data analysis.
We considered a patient to have chronic disease or comorbidity if they were diagnosed with at least one of the following diseases: diabetes, hypertension, cognitive decline, Alzheimer's disease, chronic pulmonary diseases, cardiovascular, liver, kidney or thyroid disease.
Anxyolitics, antidepressants or antipsychotics were considered to be psychotropic drugs.
EE diagnosis was defined by the presence of 15 or more eosinophils/high-power field (HPF, at magnification ×40) in mucosal biopsies. We considered that the patient had EE when the diagnosis was made prior, during or posterior to the inclusion period.
The decision to perform oesophageal biopsies in the case of impaction was left at the discretion of the performing endoscopist.
HUD is a tertiary referral centre for 710,281 patients. Urgent endoscopy is a service provided outside of regular working hours. This service is available from 3p.m. to 8a.m. Monday to Friday. On Saturday and Sunday the service is available 24h. Urgent endoscopy is performed by trained gastroenterologists and nurses without any general anaesthesia or propofol use. Urgent endoscopies are generally requested by the hospital's emergency room doctors. Less frequently, other doctors request them for admitted patients or for patients coming from other hospitals in the area. In impaction cases, the hospital's protocol is to perform endoscopy within the next six hours since the patient arrives at the emergency room.
We considered spring to be between March and May, summer to be between June and August, autumn to be between September and November and winter to be between December and February.
The study was approved by HUD ethical committee.
Statistical analysisContinuous variables are expressed by means and standard deviation, and categorical variables by percentages. To identify factors associated with EE, a bivariate analysis was performed using the Chi-square test or Fisher's exact test for categorical variables and, in the case of continuous variables, the Student's test. Those variables with p<0.20 are included in a multiple logistic regression analysis used to detect independent risk factors associated with EE. p values <0.05 were considered statistically significant. Analyses were performed using IBM Statistical Package for the Social Sciences (SPSS) software, version 23.0 (SPSS Inc., Chicago, IL).
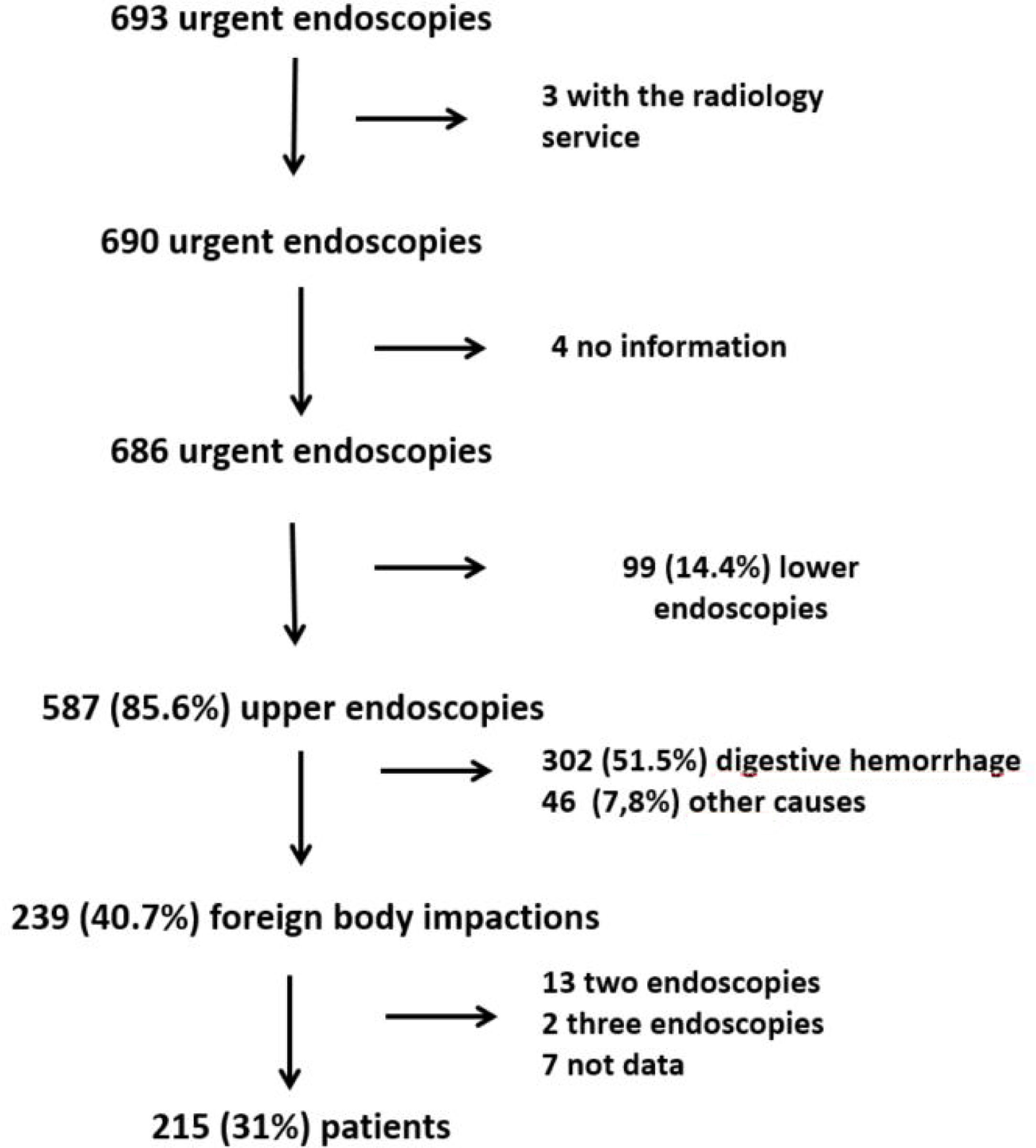
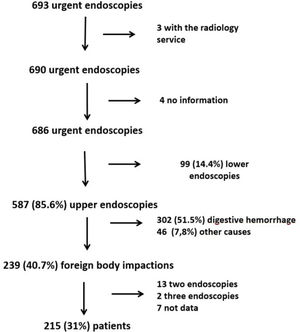
ResultsGeneral characteristics of patients with urgent endoscopy693 urgent endoscopy procedures were performed during the study period (Fig. 1). 587 (85.6%) were upper endoscopies and 99 (14.4%) lower endoscopies. The motives to perform upper endoscopies were acute upper gastrointestinal bleeding in 302 (51.5%), foreign body impaction in 239 (40.7%) and other motives in 46 (7.8%). These include; ingestion of caustic substances in 23 (3.9%), post-surgical complications in 8 (1.4%), unknow in 8 (1.4%) and other indications in 7 procedures (1.2%) which include acute abdominal pain, Anisakis infection and gastroesophageal reflux. It was not possible to find out the reason endoscopy was performed in 8 procedures because it was not listed in their clinical data or endoscopy report.
The indications to perform urgent lower endoscopy were colon stent placement in 43 (43%), colon volvulus in 29 (30%), acute lower haemorrhage in 25 (25%) and other motives in 2 procedures (2%). This last two include a rectosigmoid stricture and a fecaloma.
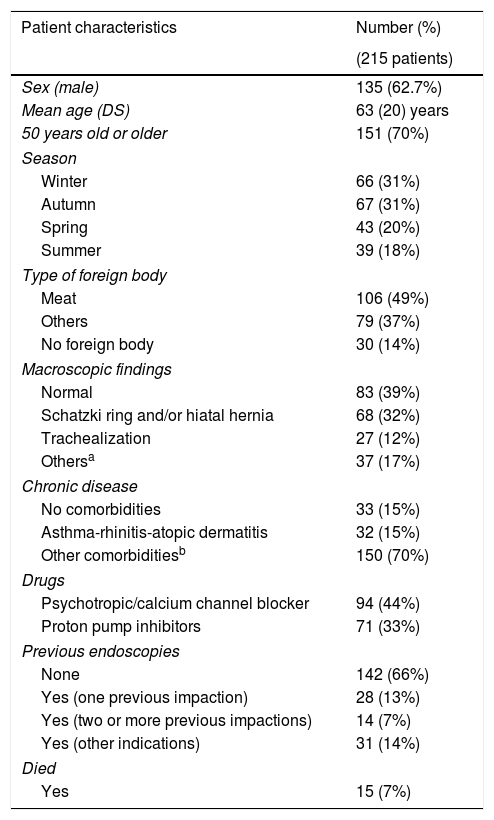
Upper endoscopy due to foreign body impaction239 (40.7%) of upper endoscopies were performed due to foreign body ingestion. During the study period 13 patients required two urgent endoscopies and two patients required three urgent endoscopies due to impaction. Seven endoscopies were excluded because we were unable to find information. Therefore, 215 patients with impaction were analyzed. Median follow-up was 18.7 months (1–30 months). In Table 1 clinical characteristics of patients with foreign body impactions are presented. 135 patients (63%) were men and 151 patients (70%) were 50 years old or older. 73 patients (34%) had undergone at least one previous endoscopy. In 30 patients (14%) no foreign body was found during the procedure.
General characteristics of patients with foreign body impaction.
| Patient characteristics | Number (%) |
|---|---|
| (215 patients) | |
| Sex (male) | 135 (62.7%) |
| Mean age (DS) | 63 (20) years |
| 50 years old or older | 151 (70%) |
| Season | |
| Winter | 66 (31%) |
| Autumn | 67 (31%) |
| Spring | 43 (20%) |
| Summer | 39 (18%) |
| Type of foreign body | |
| Meat | 106 (49%) |
| Others | 79 (37%) |
| No foreign body | 30 (14%) |
| Macroscopic findings | |
| Normal | 83 (39%) |
| Schatzki ring and/or hiatal hernia | 68 (32%) |
| Trachealization | 27 (12%) |
| Othersa | 37 (17%) |
| Chronic disease | |
| No comorbidities | 33 (15%) |
| Asthma-rhinitis-atopic dermatitis | 32 (15%) |
| Other comorbiditiesb | 150 (70%) |
| Drugs | |
| Psychotropic/calcium channel blocker | 94 (44%) |
| Proton pump inhibitors | 71 (33%) |
| Previous endoscopies | |
| None | 142 (66%) |
| Yes (one previous impaction) | 28 (13%) |
| Yes (two or more previous impactions) | 14 (7%) |
| Yes (other indications) | 31 (14%) |
| Died | |
| Yes | 15 (7%) |
EE diagnosis was confirmed in 36 patients (16.7%). In 9 patients (25%) the diagnosis had been made prior to the impaction and in the rest of them it was made in a subsequent endoscopy performed during the follow-up. There were no oesophageal perforations during the procedures and no patient required surgery to remove the foreign body.
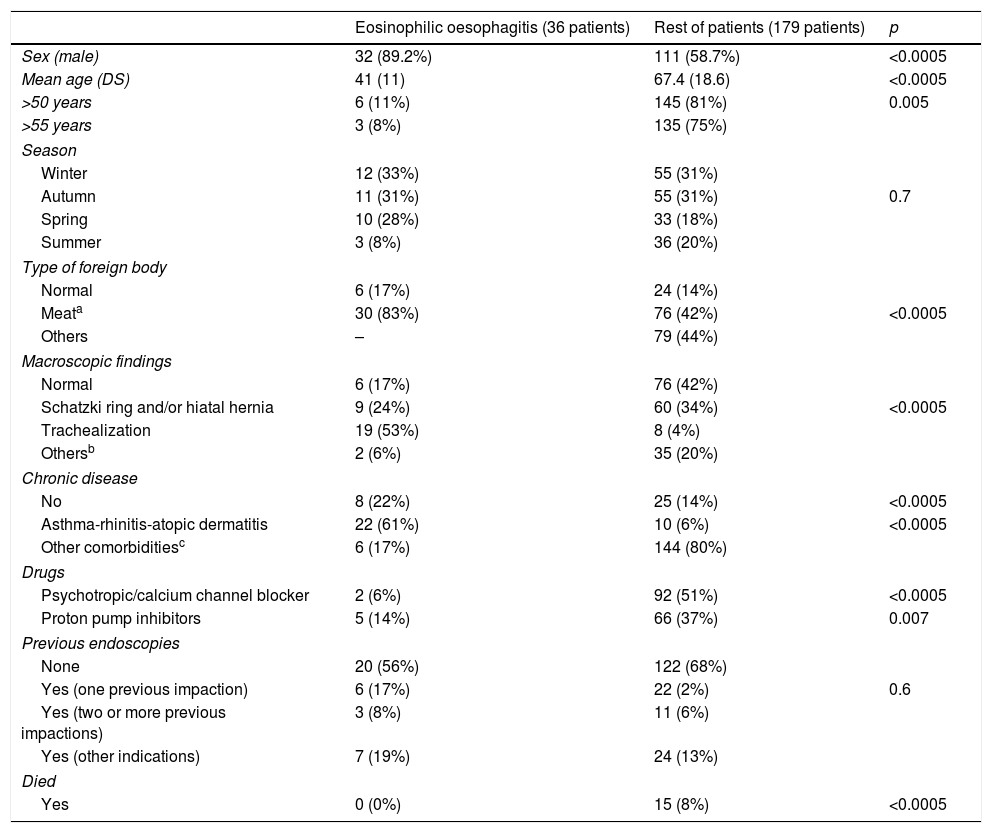
It was statistically significant for EE patients to be young men who referred meat ingestion (Table 2) compared to the other patients. Two patients with EE were initially diagnosed with gastroesophageal reflux disease (esophagitis). Furthermore, patients without EE had a higher frequency of comorbidity and need for psychotropic/calcium channel blocker drugs. On the other hand, patients with EE were more likely to have a history of asthma/rhinitis/atopic dermatitis.
Clinical characteristics of patients with eosinophilic oesophagitis compared to the rest of patients with foreign body impaction.
| Eosinophilic oesophagitis (36 patients) | Rest of patients (179 patients) | p | |
|---|---|---|---|
| Sex (male) | 32 (89.2%) | 111 (58.7%) | <0.0005 |
| Mean age (DS) | 41 (11) | 67.4 (18.6) | <0.0005 |
| >50 years | 6 (11%) | 145 (81%) | 0.005 |
| >55 years | 3 (8%) | 135 (75%) | |
| Season | |||
| Winter | 12 (33%) | 55 (31%) | |
| Autumn | 11 (31%) | 55 (31%) | 0.7 |
| Spring | 10 (28%) | 33 (18%) | |
| Summer | 3 (8%) | 36 (20%) | |
| Type of foreign body | |||
| Normal | 6 (17%) | 24 (14%) | |
| Meata | 30 (83%) | 76 (42%) | <0.0005 |
| Others | – | 79 (44%) | |
| Macroscopic findings | |||
| Normal | 6 (17%) | 76 (42%) | |
| Schatzki ring and/or hiatal hernia | 9 (24%) | 60 (34%) | <0.0005 |
| Trachealization | 19 (53%) | 8 (4%) | |
| Othersb | 2 (6%) | 35 (20%) | |
| Chronic disease | |||
| No | 8 (22%) | 25 (14%) | <0.0005 |
| Asthma-rhinitis-atopic dermatitis | 22 (61%) | 10 (6%) | <0.0005 |
| Other comorbiditiesc | 6 (17%) | 144 (80%) | |
| Drugs | |||
| Psychotropic/calcium channel blocker | 2 (6%) | 92 (51%) | <0.0005 |
| Proton pump inhibitors | 5 (14%) | 66 (37%) | 0.007 |
| Previous endoscopies | |||
| None | 20 (56%) | 122 (68%) | |
| Yes (one previous impaction) | 6 (17%) | 22 (2%) | 0.6 |
| Yes (two or more previous impactions) | 3 (8%) | 11 (6%) | |
| Yes (other indications) | 7 (19%) | 24 (13%) | |
| Died | |||
| Yes | 0 (0%) | 15 (8%) | <0.0005 |
15 patients (7%) died during the follow-up period, none of them were EE patients. The causes of death were bronchoaspiration in 6 patients, respiratory failure in 1 patients, oesophageal cancer in 4 patients and craneoencephalic trauma in 1 patient, 1 patient ischaemic stroke, 1 patient acute myocardial infarction and 1 unknown. The 7 patients with respiratory insufficiency had cognitive impairment or psychiatric disorders. Time between impaction and death was 6.4 months (1–12 months).
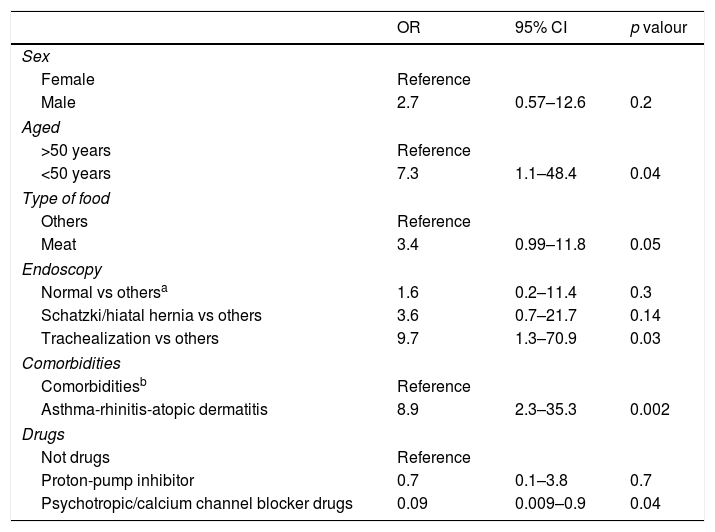
In the multiple logistic regression analysis the variables that were statistically significant were age below 50 years old, asthma or rhinitis or atopic dermatitis, visualization of trachealization in endoscopy and not taking psychotropic/calcium channel blocker drugs (Table 3).
Factors associated with presenting eosinophilic esophagitis in multivariate analysis.
| OR | 95% CI | p valour | |
|---|---|---|---|
| Sex | |||
| Female | Reference | ||
| Male | 2.7 | 0.57–12.6 | 0.2 |
| Aged | |||
| >50 years | Reference | ||
| <50 years | 7.3 | 1.1–48.4 | 0.04 |
| Type of food | |||
| Others | Reference | ||
| Meat | 3.4 | 0.99–11.8 | 0.05 |
| Endoscopy | |||
| Normal vs othersa | 1.6 | 0.2–11.4 | 0.3 |
| Schatzki/hiatal hernia vs others | 3.6 | 0.7–21.7 | 0.14 |
| Trachealization vs others | 9.7 | 1.3–70.9 | 0.03 |
| Comorbidities | |||
| Comorbiditiesb | Reference | ||
| Asthma-rhinitis-atopic dermatitis | 8.9 | 2.3–35.3 | 0.002 |
| Drugs | |||
| Not drugs | Reference | ||
| Proton-pump inhibitor | 0.7 | 0.1–3.8 | 0.7 |
| Psychotropic/calcium channel blocker drugs | 0.09 | 0.009–0.9 | 0.04 |
OR relative risk CI denotes confidence interval.
In our study more than one third of urgent upper endoscopies were performed due to foreign body impaction. 17% of these were caused by EE. It is very important to suspect this disease in patients who are 50 years old or younger, in patients who do not take psychotropic/calcium channel blocker drugs and when the patient has other risk factors for EE such as asthma, rhinitis or trachealization in endoscopy.
Studies that quantify the number of foreign body impaction patients treated by urgent endoscopy teams are very heterogeneous. Our data is higher of which presented in other studies where endoscopies performed due to foreign body ingestion were less than 10%.1,2 The reasons may be cultural, religious and gastronomical differences of the populations, age differences, hospital and endoscopy unit characteristics, prevalence of chronic disease in the populations and differences in EE prevalence according to the characteristics of the geographical areas.6,7 Older age is recognized as a cause of foreign body impaction in the gastrointestinal tract. Older patients suffer from higher rates of impairment of oesophageal motility and worse chewing ability due to dentures. These patients take more medications that can impair oesophageal motility like anxiolytics, antidepressants and calcium blockers, which are prescribed in cases of hypertension. In our study, 44% of patients took these kinds of medications. In addition, mental and neurodegenerative diseases, thyroid disease and diabetes can impact oesophageal motility and increase unnoticed ingestion of food or other foreign bodies. In our study 10% of patients suffered from dementia and 22% had thyroid disease or diabetes. Another issue associated to food bolus impaction is oropharyngeal dysphagia. This greatly increases risk of respiratory infections and ultimately risk of death. Our data shows that 6% of patients died in 12 months following urgent endoscopy and half of them in relation to infectious respiratory complications. For this reason, it is essential to follow-up and have nutrition protocols established for these patients.
Another interesting aspect of our study is that in 14% of urgent endoscopies no foreign body was found at the time of the procedure. This could be caused by spontaneous disimpaction or provoked by other means like the administration of glucagon in the emergency room. In other studies this occurs in 6–47% of cases (7–10). This is why it is necessary to adequately assess the patient before performing urgent endoscopy. Gastrointestinal endoscopy is an invasive procedure that can cause complications like perforation, aspiration pneumonia or abscesses. Severe complications or the need for surgery to remove the foreign body account for less than 4% of cases.7,11,12 In our study no patient required surgery or had major complications such as perforation or abscess.
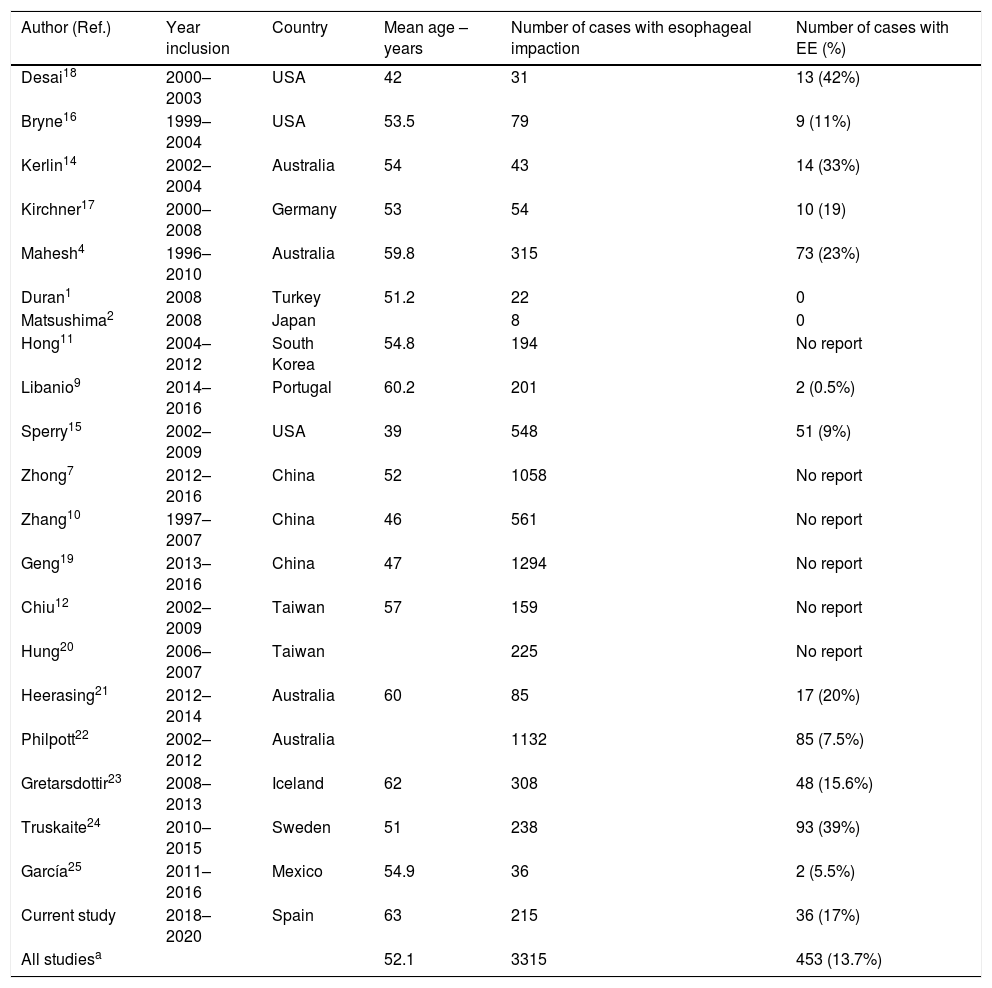
EE is a disease with an increasing prevalence. Foreign body impaction can be its clinical manifestation. In our study, 16% of patients with foreign body impactions were diagnosed with EE. These patients were 14 years old or older. However, it is possible that our series is infra-diagnosed because mucosal biopsies of the oesophagus were not taken systematically. This also occurs in other studies which review cases of adults or children.13 EE prevalence amongst adults with oesophageal impaction is very variable and can range from 1% to 42%4,8,14–25 (Table 4). In children with oesophageal impaction EE prevalence ranges between 7.9% and 28% 9,13,14 but it may also be infra-diagnosed since biopsies are not taken in all cases.
Studies describing series of esophageal impaction and the number of cases of eosinophilic esophagitis.
| Author (Ref.) | Year inclusion | Country | Mean age – years | Number of cases with esophageal impaction | Number of cases with EE (%) |
|---|---|---|---|---|---|
| Desai18 | 2000–2003 | USA | 42 | 31 | 13 (42%) |
| Bryne16 | 1999–2004 | USA | 53.5 | 79 | 9 (11%) |
| Kerlin14 | 2002–2004 | Australia | 54 | 43 | 14 (33%) |
| Kirchner17 | 2000–2008 | Germany | 53 | 54 | 10 (19) |
| Mahesh4 | 1996–2010 | Australia | 59.8 | 315 | 73 (23%) |
| Duran1 | 2008 | Turkey | 51.2 | 22 | 0 |
| Matsushima2 | 2008 | Japan | 8 | 0 | |
| Hong11 | 2004–2012 | South Korea | 54.8 | 194 | No report |
| Libanio9 | 2014–2016 | Portugal | 60.2 | 201 | 2 (0.5%) |
| Sperry15 | 2002–2009 | USA | 39 | 548 | 51 (9%) |
| Zhong7 | 2012–2016 | China | 52 | 1058 | No report |
| Zhang10 | 1997–2007 | China | 46 | 561 | No report |
| Geng19 | 2013–2016 | China | 47 | 1294 | No report |
| Chiu12 | 2002–2009 | Taiwan | 57 | 159 | No report |
| Hung20 | 2006–2007 | Taiwan | 225 | No report | |
| Heerasing21 | 2012–2014 | Australia | 60 | 85 | 17 (20%) |
| Philpott22 | 2002–2012 | Australia | 1132 | 85 (7.5%) | |
| Gretarsdottir23 | 2008–2013 | Iceland | 62 | 308 | 48 (15.6%) |
| Truskaite24 | 2010–2015 | Sweden | 51 | 238 | 93 (39%) |
| García25 | 2011–2016 | Mexico | 54.9 | 36 | 2 (5.5%) |
| Current study | 2018–2020 | Spain | 63 | 215 | 36 (17%) |
| All studiesa | 52.1 | 3315 | 453 (13.7%) |
EE; eosinophilic esophagitis.
In our study food was a more common cause for impaction than other foreign bodies like spines or bones. The most common food associated to impaction was meat. This is also shown in other studies.13,17,26
Risk factors associated with secondary impactions due to EE were being younger than 50 years old, meat impaction and having a history of asthma. Mackenzie et al.27 observe how 12% of patients who are studied because of dysphagia have EE. This prevalence increases to 35% in patients younger than 50 years old (OR=9.5). In our case, the risk of EE, increased to OR=7.3 in patients below the age of 50.
Therefore, these patient characteristics should make us suspect EE and take measures to reduce the risk of perforation, which is more likely in these patients. We should also consider taking mucosal biopsies for EE diagnosis in the same urgent procedure, especially if macroscopic findings include white exudates, linear furrows or trachealization. One third of the patients in our series required a subsequent endoscopic procedure for diagnosis of EE. This is also observed in other studies.13,15 Unlike other studies6,28,29 we did not observe a higher frequency of impactions in spring and summer amongst the EE patients compared to the non EE patients. A reason for this may be reduced pollen fluctuations given that it is a coast area. Besides, dietary factors may be more influential than environmental factors.
It is important to acknowledge the strengths and limitations of this study. Firstly, we systematically reviewed all urgent endoscopies performed in a defined population during regular clinical practice. In addition, there are few non-paediatric (14 or older patients) studies that analyze the impact of EE in the total number of gastrointestinal endoscopies performed and that analyze risk factors that may be associated with EE before urgent endoscopy. However, it is a retrospective study which makes it impossible to evaluate all clinical variables such as foreign body size, endoscopy duration, time between impaction and urgent endoscopy, use of glucagon, spontaneous resolution, etc. In addition, some EE patients may not have been diagnosed since oesophageal biopsies have not been taken in all patients.
In conclusion, oesophageal foreign body impactions are a common indication for urgent endoscopy with a not negligible mortality rate. We should always consider EE as a cause of impaction in patients younger than 50 years old or with asthma/rhinitis/atopic dermatitis or trachealization in endoscopy or who do not take psychotropic/calcium channel blocker drugs.
Authors’ contributionPA and LB developed the study concept and design and drafted the manuscript. PA, IG, JC, AI, TA, AE and LB acquired the clinical data, designed and analyzed the database and interpreted the data. LB and CS carried out the statistical analysis of data and contributed to the interpretation of data. All had the opportunity to revise the manuscript.
Conflict of interestNone of the authors have any potential conflict of interest to disclose.