Urgent gastrointestinal endoscopy (UGE) is a worldwide extended medical procedure, being the most frequent the upper and lower gastrointestinal bleeding and impaction of a foreign body the most common emergencies that require this technique.1,2 The activity in endoscopy units has been deeply affected by Covid-19 pandemic. In order to decrease the risk of infection, elective endoscopy has been stopped since “State of Alarm” was declared. However this restriction does not apply to UGE.
We analyzed the UGEs that have been performed from March 1st 2020 to April 30th 2020 and compared with those performed during the same period in the previous year (2019; pre-Covid period).
The UGE is usually performed in our hospital (Donostia University Hospital) from Monday to Friday between 3 p.m and 8 p.m and saturday/sunday during all the day. UGE are usually requested by the Emergency Department and less frequently from hospitalization rooms or intensive care unit. Regarding our protocol, we routinely perform the UGE within the 12h after admission to patients with gastrointestinal bleeding and within 6h to those with impaction of foreign bodies.
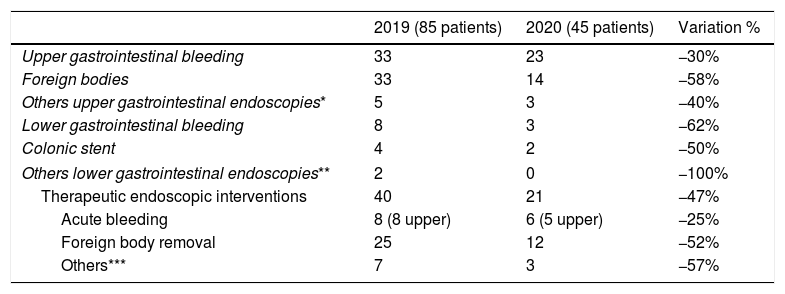
In total 126 UGE were included of which 107 (85%) were upper endoscopy. Upper bleeding was the most common clinical indication in 56 patients (44%), while impaction of a foreign body was the second most common reason for indication reported in 47 cases (37%) (Table 1). On the other hand, lower gastrointestinal bleeding was the main indication for urgent colonoscopy, performed in 11 (9%) cases, followed by 6 patients (5%) who needed stenting due to colonic obstruction related with colorectal cancer. Sixty-four procedures (51%) were performed either in Saturday or Sunday (Table 1).
Type of urgent gastrointestinal endoscopies performed in the months of March and April 2019 and 2020 and the distribution of endoscopies throughout the days of the week.
| 2019 (85 patients) | 2020 (45 patients) | Variation % | |
|---|---|---|---|
| Upper gastrointestinal bleeding | 33 | 23 | −30% |
| Foreign bodies | 33 | 14 | −58% |
| Others upper gastrointestinal endoscopies* | 5 | 3 | −40% |
| Lower gastrointestinal bleeding | 8 | 3 | −62% |
| Colonic stent | 4 | 2 | −50% |
| Others lower gastrointestinal endoscopies** | 2 | 0 | −100% |
| Therapeutic endoscopic interventions | 40 | 21 | −47% |
| Acute bleeding | 8 (8 upper) | 6 (5 upper) | −25% |
| Foreign body removal | 25 | 12 | −52% |
| Others*** | 7 | 3 | −57% |
| Days of the week | 2019 (85 patients) | 2020 (45 patients) | |
|---|---|---|---|
| Monday | 12 | 4 | −67% |
| Tuestay | 7 | 3 | −57% |
| Wednesday | 11 | 5 | −55% |
| Thursday | 7 | 4 | −43% |
| Friday | 8 | 5 | −38% |
| Saturday | 18 | 11 | −39% |
| Sunday | 22 | 13 | −41% |
Comparing the two periods, a reduction of 44% in UGE procedures was observed in the Covid period (45 Covid period vs. 81 pre-Covid). In addition, upper endoscopy was significantly more common in proportion than colonoscopy in the Covid period, 89% (40/45) vs. 83% (67/81). The number of UGE by upper gastrointestinal bleeding fell from 33 patients in the pre-Covid period to 23 patients in the Covid period, therefore constituting a reduction in 30%. In impaction of foreign bodies, a 58% decrease was observed: from 33 in the pre-Covid period to 14 during the pandemics. The percentage of emergency endoscopies that required some therapeutic procedure went from 47% (40/85) in the pre-Covid period to 47% (21/45) in the Covid period (Table 1). The number of colonoscopies needed for colonic stents in obstructive colorectal cancer decreased by half during the Covid period. It is to be noted that the decrease in the number of procedures was higher from Monday to Friday than on weekends (53% vs. 40%) (Table 1).
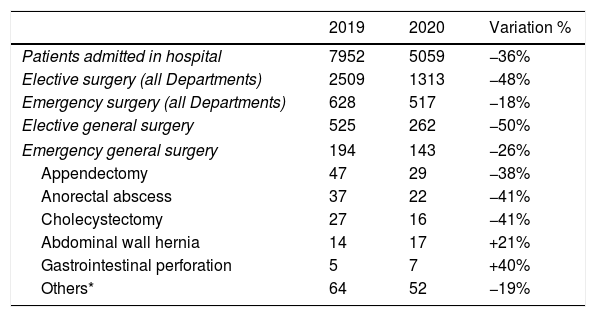
As a result of the collapse of the emergency departments and hospitals, healthcare authorities strongly suggested the population to stay at home and to avoid going to primary healthcare centers or to emergency departments, if it wasn’t essential. The number of hospital admission and elective surgery decreased a 36% and 48%, respectively (Table 2). This fact is one of the main reasons to explain the decrease on the demand for UGE in hospitals. We assume that, in our environment, many UGE do not need any therapeutic maneuver, they are just diagnostic explorations. More than half of the emergency endoscopies were conducted with diagnostic purposes, without changes in both periods (53%). Probably most of these patients presenting with melena or rectal bleeding in the current “State of Alarm,” minimized their symptoms and waited longer before attending healthcare systems. Probably, in some cames, symptoms spontaneously disappeared. In general emergency, surgery experienced a similar pattern and the number of appendectomy, abscess, or cholecystectomy decreased between 38% and 41%. It's possible that antibiotics were used more frequently in the Covid period. Another consequence of this may be an increase in gastrointestinal perforations (Table 2).
General data of the hospital in the months of March and April 2019, compared to the same period in 2020.
| 2019 | 2020 | Variation % | |
|---|---|---|---|
| Patients admitted in hospital | 7952 | 5059 | −36% |
| Elective surgery (all Departments) | 2509 | 1313 | −48% |
| Emergency surgery (all Departments) | 628 | 517 | −18% |
| Elective general surgery | 525 | 262 | −50% |
| Emergency general surgery | 194 | 143 | −26% |
| Appendectomy | 47 | 29 | −38% |
| Anorectal abscess | 37 | 22 | −41% |
| Cholecystectomy | 27 | 16 | −41% |
| Abdominal wall hernia | 14 | 17 | +21% |
| Gastrointestinal perforation | 5 | 7 | +40% |
| Others* | 64 | 52 | −19% |
Similarly, people suffering from impaction of foreign bodies could also have waited a longer time to ask for medical attention or could have tried different attempts to solve the impactation, such as drinking carbonated bevarages. Spending more time at home and having more time to eat could be another reason to explain the reduction of impactions. Probably related to the former reasons the percentage decrease of UGE due to impaction of foreign bodies was higher than the observed for GI bleeding.
On the other hand, decreased demand from hospitalization rooms may be another explanation for the reduction in the number of UGE performed. In fact, during the COVID-19 period, non-urgent surgical activity was lower, therefore the number of post-surgical complications decreased (Table 2).
There is no obvious explanation for the decrease in the treatment of colonic obstruction or volvulus, but it could be related to the probable increase of acute abdomen and peritonitis.
According to our experience, the decrease in UGE was lower on weekdays than on weekends. Perhaps the endoscopy was delayed until the next morning trying to avoid coronavirus infections.
In summary, during the Covid period, an important decrease in the emergency endoscopy and surgery was observed.
ContributionsIG and LB developed the study concept and design and drafted the manuscript. LB, PA, IG, ST, MM, JMN acquired the clinical data, designed and analyzed the database and interpreted the data. LB and IG carried out the statistical analysis of data and contributed to the interpretation of data. All had the opportunity to revise the manuscript.
We thank Arantza Zubizarreta, Javier Basterrechea and Nieves Gonzalez-García for his kind collaboration in this study.